Abstract
Aims: This study sought to investigate the incidence of stent thrombosis (ST) in patients treated with drug-eluting stents (DES) and clearly defined short-term dual antiplatelet therapy (DAT) for three or six months for sirolimus-eluting stents (SES) or paclitaxel-eluting stents (PES), respectively.
Methods and results: A series of 1,023 consecutive patients with 1,414 stented lesions and prescribed short-term DAT were followed for at least two years after DES implantation. The individual durations of DAT, the rate of ischaemic events, and survival status were assessed.
Follow-up was completed for 1,017 patients (99.4%) with a mean follow-up of 3.0±0.7 years. DAT duration was 2.8±0.4 and 5.9±0.8 months in patients with SES and PES, respectively. Adherence to continued single antiplatelet therapy was 98.4%. We identified 14 patients with definite ST (1.4%) and no patients with probable ST with a cumulative incidence of 0.6% at 30 days, of 0.8% at one year, of 1.2% at 2 years, and of 1.4% at three years.
Conclusions: Definite or probable ST after DES implantation and short DAT occurs with a cumulative incidence of 1.4% at 3 years if excellent patient adherence to the continued single antiplatelet therapy can be achieved.
Introduction
Compared to bare-metal stents (BMS), drug-eluting stents (DES) effectively reduce the risk of repeated revascularisation1-5. However, a considerably high rate of delayed stent thrombosis (ST) of up to 0.6% per year may detract from these beneficial effects6-11.
Though ST in DES also occurs during dual antiplatelet therapy (DAT) and no exact chronological correlation between cessation of clopidogrel and delayed ST has yet been identified, there is statistical evidence that prolonged DAT can reduce the risk of serious cardiac events also more than six months after DES implantation12-14. Therefore, all major cardiology societies currently recommend DAT for 6-12 months after DES implantation, if well tolerated15,16.
Because DAT significantly increases the risk for major bleeding complications17 and numerous patients require unplanned non-cardiac interventions after DES implantation, the safety of discontinuing at least clopidogrel within the first year post DES implantation is an important issue. However, available safety evidence pertaining to this post-DES implantation period is based on the results of trials that allowed prolonged DAT and did not assess the exact duration of antiplatelet treatment in their study populations2-5.
In our institution, DES implantation has been the standard of care since June, 2002. Between 2002 and 2004, all patients with sirolimus-eluting stents (SES) and paclitaxel-eluting stents (PES) were prescribed clearly defined, short-term DAT for three and six months, respectively. We wanted to confirm the individual durations of DAT and to investigate the incidence of ST in a DES population treated with short-term DAT.
Methods
Patient population
We performed a long-term (minimum 2 years) follow-up observational study on a cohort of patients treated with DES from June, 2002 through December, 2004. After completion of the index procedure (first implantation of a SES or PES), all subsequent ischaemic events in these patients were prospectively recorded in a DES-database. All patients had a routine outpatient clinical control at our institution six months after DES implantation, which included an assessment of the clinical course, and the adherence to DAT after stent implantation, as well as the prescription of the future medical therapy. At this visit, clopidogrel was stopped in all patients still on DAT and each patient was counselled to categorically maintain indefinite single antiplatelet therapy with aspirin. In patients with gastrointestinal intolerance of aspirin, a proton pump inhibitor therapy was initiated. Only in the case of ongoing gastrointestinal symptoms was single antiplatelet therapy with aspirin changed to clopidogrel. All relevant information about DAT was documented in the database. Additionally, in January, 2007, all patients were contacted by phone and interviewed about their clinical course as well as any changes of the antiplatelet therapy following the outpatient visit six months after stent implantation and the exact duration of their antiplatelet therapy following stent implantation. For patients who suffered from myocardial infarction or had to undergo coronary angiography in other hospitals, discharge summaries, medical records, and compact discs of the angiograms were ordered and systematically reviewed. General practitioners, referring cardiologists and emergency doctors were contacted for additional information. In the case of fatalities, all available information including emergency protocols, interviews of witnesses and relatives, and autopsy reports were analysed. Survival status of patients for whom no post-discharge information could be obtained was provided by the municipal civil registries. These patients were counted as loss of follow-up if they were alive; otherwise, the cause of death was assumed to be probable or possible ST.
This study was approved by the local ethics committee and was performed in accord with the Declaration of Helsinki.
Stent implantation and periprocedural antiplatelet management
We used SES (Cypher, Cordis Corporation, Johnson & Johnson, Miami Lakes, FL, USA) or PES (Taxus, Boston Scientific Corporation, Natick, MA, USA) for all patients in this study. All interventions were performed according to standard techniques with the decision about the appropriate strategy and stent type in each case left to the judgment of the operator. In accordance with our institution’s implant strategy, stents were routinely deployed with high pressure (≥12 atmospheres). Patients were pre-treated with aspirin and a loading dose of 300 mg clopidogrel. Only patients with primary intervention for acute ST-elevation myocardial infarction received a weight-adjusted intravenous abciximab bolus immediately before the intervention. In all other patients, administration of abciximab was reserved for bail-out use in cases of peri-interventional intravasal thrombus formation. Post-interventional abciximab infusion was not mandatory and left to the discretion of the operator.
Duration of combined antiplatelet therapy
All patients were strongly advised to maintain lifelong aspirin therapy (100 mg daily) in combination with clopidogrel (75 mg daily) for three or six months (for patients with SES or PES, respectively). Longer combined antiplatelet therapy was not prescribed for patients with acute coronary syndromes or for patients with bifurcational lesions or in-stent restenosis. At discharge, each patient received a handout with information about the duration of their clopidogrel therapy, a prescription for aspirin and clopidogrel, a passport-sized “DES-card”, and a provisional medical summary stressing the important points about DAT for their referring physician.
Definition of stent thrombosis
According to the definitions established by the Academic Research Consortium (ARC) in December 2006, ST was classified as definite, probable, or possible, and as acute (occurring during intervention or within the following 24 hours), subacute (occurring within one to 30 days post intervention), late (occurring between 31 to 360 days post intervention), or very late (occurring more than one year after DES implantation). Definite ST required angiographic or autopsy evidence of thrombus or occlusion in the clinical setting of an acute coronary syndrome. Probable ST included unexplained deaths within 30 days after the index procedure or acute myocardial infarction involving the target-vessel territory but no angiographic thrombus confirmation. Possible ST included all unexplained deaths >30 days after DES implantation18.
Statistical analysis
Continuous data are presented as mean±standard deviation. Dichotomous variables are described as counts and percentages. For comparison of continuous variables, we used a paired or unpaired t-test, as appropriate. Kaplan-Meier curves were used to calculate the time-dependent occurrences of events. All statistical analysis was performed using SPSS for Windows (version 13.0, SPSS Inc., Chicago, Ill, USA).
Results
Patients and procedural characteristics
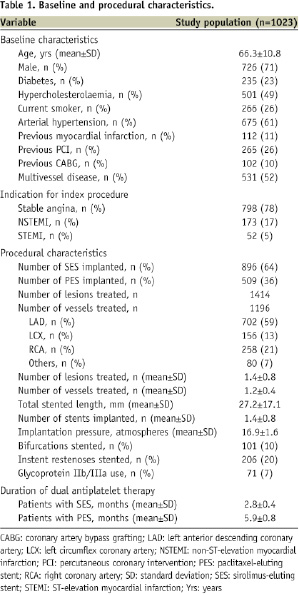
Between June 2002 and December 2004, 1,023 patients were treated with a DES implantation as the index procedure. The average age of our patients was 66 years, and 71% of patients were male. Over half of the patients had angiographic multivessel disease, 17% underwent DES implantation for non-ST-segment elevation myocardial infarction, and 5% for ST-segment elevation myocardial infarction. In total, 1,405 DES (896 SES and 509 PES) were implanted. An average of 1.4 lesions in 1.2 vessels were treated with the implantation of 1.4 stents and a stented length of 27 mm per patient (Table 1).
Follow-up and duration of dual antiplatelet therapy
All telephone contacts occurred during January, 2007. Accurate medical follow-up was completed for 1,017 patients (99.4%) with a mean follow-up of 3.0±0.7 years. Mean duration of DAT after DES implantation, as determined by telephone interview, was 2.8±0.4 months and 5.9±0.8 months for patients with SES and PES, respectively. Only 3.3% of patients with SES and 1.9% of patients with PES reported a longer clopidogrel intake than that recommended at discharge. Because clopidogrel is distributed in packets of 84 pills in Austria, many patients with SES or PES were on DAT for only 84 or 168 days, and not exactly three or six months, respectively. Compliance to ongoing single antiplatelet therapy, as reported by the patients at follow-up, was 98.4% (97.8% of these patients were on single aspirin and 2.2% on single clopidogrel).
Incidence and timing of stent thrombosis
There were 14 cases of definite ST in 14 patients (1.4%, 95% confidence interval =0.8% – 2.3%), nine with SES and five with PES. We identified no patients with probable ST. Thus, when these two major ARC criteria, definite and probable ST, were applied, the cumulative incidence of ST was 1,4% (14/1023 patients), with a cumulative incidence of 0.6% at 30 days, of 0.8% at one year, of 1.2% at 2 years and of 1.4% at 3 years. Another twenty patients (2.0%), had possible ST. Thus, when all three ARC criteria were applied, the cumulative incidence of ST was 3.4% (34/1023 patients, 23 with SES and 11 with PES; Table 2), with a cumulative incidence of 0.6% at 30 days, of 1.2% at one year, of 2.3% at 2 years and of 3.2% at 3 years (Figure 1).
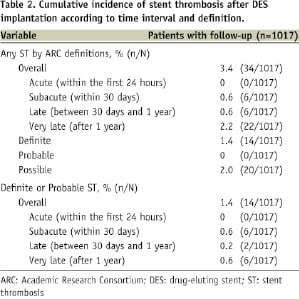
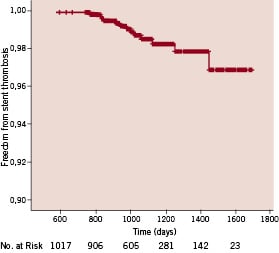
Figure 1. Freedom from stent thrombosis Kaplan Meier curve showing cumulative freedom from stent thrombosis.
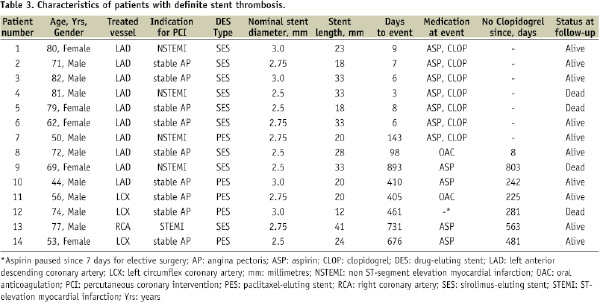
In the patients with definite ST, no acute cases occurred, but six subacute cases (occurring between three and nine days post intervention), two late cases (occurring after 98 and 143 days), and six very late cases (occurring between 405 and 893 days) occurred. No patients with subacute ST suffered from late or very late ST. All patients with subacute definite ST were on DAT. Of the two patients with late definite ST, one was on DAT (patient 7, ST occurred 143 days after PES), whereas the other patient was on sole oral anticoagulation (patient 8, ST occurred 98 days after SES, international normalised ratio [INR]=3.2) and had stopped aspirin and clopidogrel eight days prior. The six patients with very late definite ST were on aspirin in four cases, on sole oral anticoagulation in one case (patient 11, ST occurred 405 days after PES, INR=2.3), and on no medication in one case (patient 12, ST occurred 461 days after PES and seven days after stopping aspirin for elective surgery). In the patients who suffered from definite ST after completion of the prescribed dual antiplatelet protocol, the mean interval between cessation of clopidogrel and ST was 370±243 days (range, 8-803 days). One case of definite ST (patient 8) and three cases of possible ST occurred between cessation of clopidogrel and one year after DES implantation. In three cases of definite ST (21%), both clopidogrel and aspirin had been discontinued.
All 14 patients with definite ST presented with ST-segment elevation myocardial infarction. Rescue percutaneous coronary intervention was performed in all cases. No Thrombolysis in Myocardial Infarction (TIMI) flow 2 or 3 could be restored in two cases. Both patients (patients 1 and 13) are still alive. There were four deaths related to definite ST (33%) despite successful rescue intervention, two each in the settings of early (patient 4 died of pump failure 20 days after ST, patient 5 died of cardiogenic shock one day after ST) and very late ST (patients 9 and 12 died of pump failure 14 and 19 days after ST, respectively). Autopsy was performed for all patients and demonstrated an open infarct-related coronary artery in each case. Characteristics of all patients with definite ST are listed in Table 3.
Total mortality of the entire population was 9% (90/1023 patients). Four patients died of definite ST, 20 patients died of possible ST (unexplained death >30 days after DES implantation), and 66 patients died of other causes in hospital (autopsy was performed in 50%).
Discussion
To our knowledge, this is the first long-term follow-up study that reports the incidence of ST in patients with DES and documented short-term DAT. We prescribed adjunctive clopidogrel for three or six months in addition to indefinite aspirin treatment after implantation of SES or PES, respectively, and showed that clopidogrel therapy did not extend beyond the prescribed limits in our patient population. Applying the ARC criteria, we found a rate of definite and probable late and very late ST of 0.8%, consistent with previous reports6-11.
These results are clinically important because they provide insight into the incidence and time course of ST following cessation of short-term adjunctive clopidogrel treatment after DES implantation, and may be particularly helpful in determining the risk of discontinuing clopidogrel, if medically necessary, three to 12 months after DES implantation. At the time of patient enrolment in this study, prolonged DAT for six to 12 months after DES implantation was not recommended by the major cardiology societies as it is today15,16; therefore, it is unlikely that future studies with a comparably short term of DAT will be conducted.
Comparison with previous studies
The use of DES reduces the risk of in-stent restenosis; however, this beneficial effect is threatened by the risk of late and very late ST1-12. Delayed endothelialisation, incomplete neointimal healing, or hypersensitivity reactions after DES implantations are the most probable underlying mechanisms19,20. Currently, prolonged DAT seems to be the only means to moderately reduce the risk of ST in DES10-14,21. As a consequence, all major cardiology societies recommend DAT for six to 12 months, if well tolerated, after DES implantation15,16. However, general application of these guidelines
is likely to increase the number of bleeding complications or delay diagnostic and therapeutic interventions17. Therefore, the question remains: at what point can the clopidogrel portion of DAT be stopped at a risk of ST not overwhelming that of bleeding complications or delayed interventions? Currently available scientific evidence cannot provide the answer. Guidelines demand continued DAT for at least three and six months after implantation of SES and PES, respectively15,16, and refer to the proven safety of the prescribed minimum duration in major randomised DES trials conducted in 2002 and 20032-5. However, because late decisions regarding antiplatelet therapy were not regulated by the study protocols and prescription of DAT for up to 12 months was widely performed after publication of the “Clopidogrel in Unstable angina to prevent Recurrent Events” (PCI-CURE) and “Clopidogrel for the Reduction of Events During Observation” (CREDO) trials in 2001 and 2002, respectively2-5,11,13,14,22, the portion of patients on prolonged DAT in these trials was substantial. A meta-analysis of the TAXUS IV, V, and VI – trials, for example, found that more than half of the patients had been on continuous DAT 9 months after PES implantation8, and a pooled analysis of four randomised trials evaluating the safety of SES admitted that duration of DAT was not ascertained beyond the protocol-recommended duration of two to three months11. Moreover, the results from randomised trials do not apply to all real-world applications. However, evidence for the incidence of ST in all-income populations is derived exclusively from studies that prescribed DAT for six to 12 months after DES implantation or that did not assess the actual duration of antiplatelet treatment6-12,23-25. Even the “Basel Stent Kosten Effektivitäts Trial – LAte Thrombotic Events” (BASKET-LATE), that evaluated the rate of ST following discontinuation of clopidogrel after six months, reported one case of late ST despite continued DAT for more than a half year23. In contrast to these studies, our patients were on documented short-term DAT for exactly three and six months after implantation of SES and PES, respectively. This close adherence to the prescribed duration of DAT can be explained by the precise protocol provided to patients and referring physicians at discharge and the fact that patients were not transferred to other hospitals after DES implantation.
Clinical implications
We found two definite and no probable ST cases (0.2%) occurring late after DES implantation. Of these, one definite ST occurred on DAT and one on sole oral anticoagulation. This observed rate of late ST in our study corresponds with earlier reports on late ST after DES implantation but longer duration of DAT6,23,25. There are several potential explanations for the observed low incidence of ST after discontinuation of short-term DAT: (1) Good adherence to single antiplatelet therapy after cessation of clopidogrel due to effective education of patients and referring physicians. Discontinuation of aspirin therapy has been shown to be closely associated with ST after implantation of BMS and DES26,27. Withdrawal of aspirin treatment in patients undergoing surgical procedures is known to be potentially hazardous because peri-operative stress and surgical trauma enhance platelet aggregation and thus enhance the risk of ST27. Numerous reports on late ST after discontinuation of aspirin for non-cardiac procedures highlight the importance of maintaining at least single antiplatelet therapy6,27,28. (2) The limited ability of adjunctive clopidogrel treatment to prevent late and very late ST in DES. Although several studies reported that most cases of late and very late ST occurred in the absence of clopidogrel treatment, no investigation identified a chronological correlation between clopidogrel cessation and the development of ST6,23,24. Moreover, Daemen et al (2007) reported a similar incidence of late ST in two large populations of patients who were prescribed DAT for six
or 12 months after DES implantation6. In contrast, a recent study found a significantly increased risk for death and major cardiac events in patients who had discontinued clopidogrel within 12 months after DES implantation. However, in this study, 15% of all patients had ceased single antiplatelet therapy within the first year post stenting; therefore, it was impossible to attribute all events to the cessation of clopidogrel alone12. (3) Accurate interventional technique, reflected by the high mean stent implantation pressure of 17 atmospheres and the low incidence of acute or subacute ST of 0.6%. It is widely accepted, that malapposition of improperly deployed BMS and DES can trigger ST, which then predominantly occurs during the first months after implantation29,30. (4) In our patient cohort, a relatively small percentage of patients (22%) underwent the index procedure for acute coronary syndromes, including acute myocardial infarction, compared to rates of 55% to 63% reported in other studies6,23-25. Percutaneous coronary interventions in the context of acute coronary syndromes are associated with a significantly increased rate of subsequent ST. A large cohort study including more than 8,100 consecutive patients with DES reported that 70% of all ST cases occurred in patients who underwent the index percutaneous coronary intervention for acute coronary syndromes6. Furthermore, it could be shown that clopidogrel discontinuation after prolonged use of about 300 days was still associated with an increased mortality risk in patients with implantation of BMS or DES for acute coronary syndromes31.
Limitations
As intravascular ultrasound studies were neither performed during the index procedures nor during percutaneous interventions for ST, possible accompanying pathologies, such as instent restenosis or stent malapposition, could not be excluded.
Conclusions
Our data suggest that definite or probable ST after DES implantation and short DAT occur in 1.4% with high pressure stent implantation and excellent patient adherence to the prescribed antiplatelet therapy. Cessation of DAT after three to six months is rarely complicated by ST within the first year after DES implantation if single antiplatelet therapy treatment is continued, indicating a strategy that should also be followed for non-cardiac interventions.

