Abstract
Aims: The aim of this study was to determine the impact of bifurcation lesions on outcomes after primary percutaneous intervention (PCI) for acute myocardial infarction.
Methods and results: We retrospectively reviewed a single-centre database of 646 patients admitted for primary angioplasty within 12 hours after AMI. We compared baseline characteristics and outcomes between bifurcation and non-bifurcation lesions.
Bifurcation lesions were found in 23% of patients. They predominantly involved the left anterior descending artery. Provisional T-stenting was used in 89.3% of patients (with stenting of the main branch in 82% and of both branches in 7.3%), side-branch protection in 54.6%, and final kissing balloon inflation in 33%. The procedural success rate was 92% for the main branch of bifurcation lesions compared with 93% for non-bifurcation lesions (P=0.65). Major adverse cardiac event (MACE) rates were comparable in the two groups: in-hospital MACE was 13.3% in the bifurcation group versus 11.4% in the non-bifurcation group (P=0.72), and the 1-year total MACE rate was 22.6% in the bifurcation group versus 19.5% in the non-bifurcation group (P=0.56).
Conclusions: Bifurcation lesions are common in patients with AMI. In a population with AMI, immediate and mid-term outcomes of primary PCI were similar in patients with and without bifurcation lesions.
Introduction
Bifurcation lesions account for about 15% to 20% of coronary artery stenosis managed by percutaneous coronary intervention (PCI)1. The best strategy for treating bifurcation lesions remains controversial. Factors that influence treatment decisions include target vessel size, nature and angle of the side branch, whether the ostium is involved, plaque volume, and likelihood of plaque shifting2-5. Although PCI techniques have improved substantially with the introduction of new stent designs, side-branch protection, kissing balloon inflation, and debulking, bifurcation lesions raise technical challenges6,7. Lower angiographic success rates and higher restenosis and thrombosis rates were noted after PCI for bifurcation lesions, especially when multiple stents were used8-10,22. Little is known about the impact of bifurcation lesions on procedural success rates and long-term outcomes after primary PCI in patients with acute myocardial infarction (AMI). We evaluated immediate and mid-term outcomes of PCI used to treat bifurcation lesions compared to non-bifurcation lesions in patients referred to our institution for AMI.
Methods
Patients and study design
We examined data of 646 consecutive patients who were admitted to our centre within 12 hours after AMI, who were eligible for primary PCI and were free of cardiogenic shock at presentation. We retrospectively analysed the database comparing patients with and without bifurcation on the treated culprit vessel. AMI was diagnosed according to American College of Cardiology/American Heart Association criteria: typical chest pain, ST segment elevation by more than 2 mm in one or more leads of a 12-lead electrocardiogram, new left bundle branch block, and/or elevation of biochemical markers for myocardial damage (CPK MB and/or cardiac troponins)11.
To evaluate the impact of bifurcation lesions on clinical outcomes of primary PCI for AMI, we compared the rate of major adverse cardiac events (MACE) during the hospital stay and during the first post-procedure year in patients with and without bifurcation lesions. MACE encompasses death, recurrent myocardial infarction, and target lesion revascularisation (TLR). Recurrent myocardial infarction was defined as recurrent ischaemic symptoms and or ECG changes following the procedure together with an elevation of biomarkers of cardiac damage (CK MB, or troponin) three times above the 99th percentile of upper reference limit (URL)27. TLR was defined as a repeated revascularisation procedure (PCI or CABG) driven by symptoms or laboratory test results combined with control angiographic evidence of at least 50% stenosis within the treated lesion.
Angioplasty procedures
Primary PCI was performed in all study patients using 6 Fr material. Percutaneous access was via the femoral or radial approach. Diagnostic and angioplasty materials (e.g., catheters, guide wires, balloons, and stents) were selected according to the target vessel, lesion type, and lesion morphology. Aspirin in a dosage of 250 mg to 325 mg was given before the procedure, either before arrival at the hospital or in the catheterisation laboratory, together with a 300-mg loading dose of clopidogrel or an equivalent dose of ticlopidine unless the patient was on antiplatelet therapy before the AMI. Intravenous heparin was given to maintain an activated clotting time greater than 300 seconds during the procedure, and glycoprotein IIb/IIIa inhibitors were used when indicated. Intracoronary vasodilators were injected before balloon inflation to allow accurate lesion assessment. In the bifurcation-lesion group, the treatment strategy was determined according to the type of the bifurcation lesion, size and accessibility of the side branch, and likelihood of plaque shifting. Lesions were pre-dilated if needed, and final kissing balloon inflation was performed to optimise the results. After the procedure, aspirin was continued indefinitely, and clopidogrel 75 mg/day or ticlopidine 250 mg twice daily was used for at least 12 months according to the ESC guidelines for acute coronary syndromes. Procedural success was defined as less than 30% residual stenosis in the treated vessel and TIMI 3 flow without acute complications during the hospital stay.
Follow-up
Follow-up data were obtained by telephone interview or during an outpatient clinic visit one year after the procedure. Patients who reported symptoms or signs of recurrent ischaemia underwent a full physical examination, a 12-lead electrocardiogram, biochemical assays, and tests to evaluate myocardial ischaemia and viability. Selective coronary angiography with angioplasty or CABG was performed in patients who had evidence of recurrent ischaemia.
Quantitative coronary assessment
Quantitative coronary assessment (QCA) was performed in the bifurcation-lesion group. Minimal luminal diameter (MLD), reference vessel diameter (RVD), and diameter stenosis (%DS) of the target lesion were measured for both the main vessel and the side branch on similar angiographic views before and after PCI, using dedicated software (CAASII, Pie Medical Imaging, Maastricht, The Netherlands). For control angiography during follow-up, in-stent restenosis was defined as (%DS) > 50% within the stented segment.
Bifurcation lesions were categorised using the Medina classification recently adopted by the European Bifurcation Club12.
Statistical analysis
Continuous variables were expressed as means±SD and compared using Student’s t tests. Chi-square tests were used to compare categorical variables. P values <0.05 were considered statistically significant.
Results
Patients and lesions characteristics
Bifurcation lesions were detected in 150 (23%) of the 646 patients. The baseline characteristics of the patients are reported in Table 1.
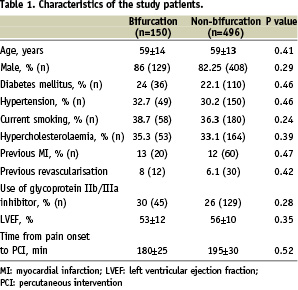
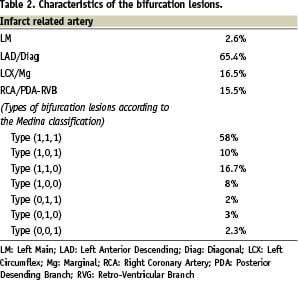
No statistically significant differences were found between the bifurcation and non-bifurcation groups regarding age, gender distribution, diabetes, smoking, hypertension, dyslipidaemia, left ventricular function, history of myocardial infarction, history of CABG, need for GPIIb/IIIa inhibitors, or time from chest-pain onset to PCI. The distribution of bifurcation lesions according to Medina classification12 was as follows: type (1,1,1) 58%; type (1,0,1) 10%; type (1,1,0) 16.7%; type (1,0,0) 8%, type (0,1,1) 2%; type (0,1,0) 3% and type (0,0,1) 2.3%. In the bifurcation group, the lesion involved the left anterior descending/diagonal arteries in 65.4% of cases, left circumflex/marginal arteries in 16.5%, right coronary artery/crux in 15.5%, and left main bifurcation in 2.6%. Characteristics of the bifurcation lesions are shown in Table 2.
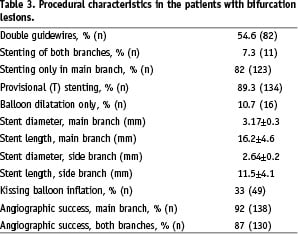
The percentage of TIMI flow 0 in the main branch of the bifurcation lesion group before PCI was 56.7% while it was 41.3% in the side branch respectively, compared with 65.7% in the non-bifurcation group (see further, Table 6).
Procedural data
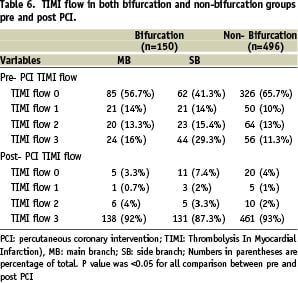
The procedural success rate was 92% in the bifurcation group and 93% in the non-bifurcation group (P=0.65). All procedural failures were characterised by 30% or greater residual stenosis with a TIMI flow grade less than 3 at the end of the procedure. Post-PCI no-reflow (TIMI 0) was 3.3% in the main branch and 7.4% in the side branch in the bifurcation lesion group, compared with 4% in the non-bifurcation lesion group. Slow-flow (TIMI 1,2) was 4.7% in the main branch and 5.3% in the side branch post-PCI in bifurcation group, compared with 3% in the non-bifurcation group (Table 6). In the bifurcation group, provisional T-stenting was performed in 89.3% of cases, with stenting of the main branch only in 82% of cases (direct stenting in 53% of cases) and of both branches in 7.3% of cases. Decision of stenting of the side branch was taken by the operators according to size of the side branch and the territory supplied by this branch and persistence of TIMI less than 2. The small RVD of the side branch (2.32 mm) partly explain the low rate of side branch stenting. BMS were exclusively used in this study. In the remaining 10.7% of cases, revascularisation was performed by balloon angioplasty without stenting. Double guidewire protection was used in 54.6% of cases and final kissing balloon inflation in 33% of cases. Mean stent diameter was 3.17±0.3 mm for the main branch and 2.64±0.2 mm for the side branch; mean stent length was 16.2±4.6 mm for the main branch and 11.5±4.1 mm for the side branch (Table 3).
Quantitative coronary angiography in the group with bifurcation lesions
Quantitative angiographic measurements for the main branch and side branch are reported in Table 4.
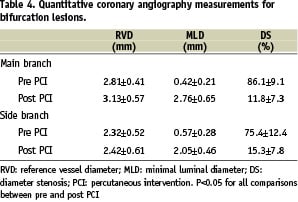
Mean RVD for the main branch was 2.81±0.41 mm before PCI and 3.13±0.57 mm after PCI; corresponding values for the side branch were 2.32±0.52 mm and 2.42±0.61 mm, respectively. MLD for the main branch was 0.42±0.21 mm before PCI and 2.76±0.65 mm after PCI; corresponding values for the side branch were 0.57±0.28 mm and 2.05±0.46 mm, respectively. The %DS before PCI was higher in the main branch than the side branch (86% versus 75%), whereas the %DS after PCI was higher in the side branch than in the main branch (15% versus 11%) (P<0.05 for all comparisons).
Clinical follow-up
Data were obtained at least one year after PCI for 96% of the patients, in whom mean follow-up was 1.2 year; 26 patients were lost to follow-up (eight patients in the bifurcation group, 18 patients in the non-bifurcation group). The in-hospital MACE rate was 13.3% in the bifurcation group and 11.4% in the non-bifurcation group (P=0.72). Corresponding rates were 3.3% vs. 2% for in-hospital mortality (P=0.35), 4% vs. 4.4% for recurrent myocardial infarction (P=0.81), and 6% vs. 5% for target lesion revascularisation (TLR), respectively (P=0.94). The acute and sub- acute stent thrombosis rate (certain and probable according to ARC definitions) was 3.3% in the bifurcation lesion group compared with 2% in the non-bifurcation group (P=0.38; see further, Table 5).
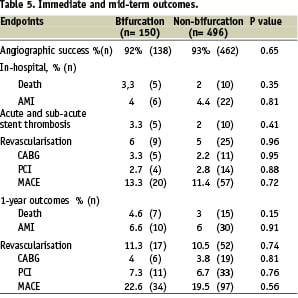
After one year, mortality was 4.6% in the bifurcation group versus 3% in the non-bifurcation group (P=0.15); corresponding rates were 6.6% vs. 6% for recurrent myocardial infarction (P=0.91), 11.3% vs. 10.5% for TLR (P=0.74), and 22.6% vs. 19.5% for MACE (P=0.56) after one year, respectively (Table 5).
Discussion
Angioplasty of bifurcation lesions remains challenging. In most studies, long-term outcomes were less favourable compared to non-bifurcation lesions. To our knowledge, no previous studies specifically assessed the impact of bifurcation lesions on the immediate and mid-term outcomes of PCI used to treat AMI. Patients with bifurcation lesions were excluded from most of the randomised studies of AMI. In our study, the prevalence of bifurcation lesions was 23% among 646 consecutive patients referred to our catheterisation laboratory for AMI. Lower prevalences, usually less than 20%, were found in studies of PCI in the absence of acute coronary syndrome; for example, bifurcation lesions were found in only 12.3% of patients in the large cohort studied by Garot et al13. Rheologic considerations are consistent with a higher prevalence of bifurcation lesions in patients with acute arterial occlusion. In our study, the bifurcation and non-bifurcation groups were similar regarding the history of myocardial infarction and CABG, left ventricular function, diabetes, and other risk factors. The procedural success rate was not significantly different between the two groups, i.e., 92% for the bifurcation main artery and 93% for the non-bifurcation lesions. Failure rates in bifurcation lesions ranged from 3% to 13% in previous studies14,15, being higher than for non-bifurcation lesions. The absence of a significant difference in our study may be ascribed to the techniques used to treat bifurcation lesions and to the comparable times from pain onset to PCI in the two groups. In previous studies, provisional T-stenting, the technique used for most of the lesions in our patients, yielded higher feasibility rates and lower complication rates than other techniques. Furthermore, provisional T-stenting may predict a favourable outcome, according to a study done by Lever et al16 on a large single-centre registry of 1,149 bifurcation lesions seen over seven years. Many techniques for bifurcation treatment have been described in the literature28, but in the specific setting of acute myocardial infarction, simple and rapid techniques such as provisional T stenting is probably the most suitable. Final kissing has been recommended to optimise stent apposition, correct stent deformation or distortion and improve side branch access, but systematic use was not a consensus in all bifurcation PCI. In our study final kissing balloon was performed in only 33% of cases. This was the operator’s choice, probably to avoid possible thrombus mobilisation in this critical thrombotic setting.
The in-hospital MACE rate was not significantly different between the bifurcation and non-bifurcation groups (13.3% versus 11.4%, P=0.72). Lower rates were found in the previous studies of PCI for AMI. The 30-day MACE rates after PCI were 8.4% in the AIR-PAMI trial17 and 6.2% in CAPTIM18. The higher MACE rate in our study may be ascribed to the absence of patient selection. The rate of acute and sub acute stent thrombosis which was 3.3% in the bifurcation group and 2% in the non-bifurcation group was a contributing factor for the rate of in-hospital reinfarction and TLR and is comparable with BMS arm of recent studies like TYPHOON29.
MACE rates after one year in our study were not significantly different in the two groups (22.6% in the bifurcation group and 19.5% in the non-bifurcation group, P=0.56). The 6-month MACE rates in Stent-PAMI19 were 12.6% with stenting and 20.1% with balloon dilatation alone. In STOPAMI20, 6-month MACE rates were 8.5% after stenting and 23.2% after thrombolysis. Our results also militate against an association between bifurcation lesions and adverse 1-year outcomes after AMI. In patients treated at a distance from AMI, Lever et al16 recorded 7-month MACE rates of 13.7% with provisional T-stenting followed by implantation of a single stent, 18% with provisional T-stenting followed by implantation of two stents, 24.5% with primary implantation of two stents, 42.8% with the culotte technique, and 33.8% with kissing stents; they concluded that provisional T-stenting significantly reduced the MACE rate and the need for repeat TVR within the first seven months. Similarly, in a prospective two-centre study using the Bestent™21, provisional T-stenting was associated with a low 6-month MACE rate of 14.3%, including a 9.4% TVR rate. Several other studies found better outcomes with one stent than with two stents in patients who had bifurcation lesions22-24. In the PRESTO trial13, angioplasty of bifurcation lesions was associated with an increased 9-month MACE rate (18% versus 15% for non-bifurcation lesions). This difference was mainly ascribable to a higher TVR rate in bifurcation lesions (17% versus 14%), whereas death (1%) and AMI (1%) were not different between the two groups. The increased need for TVR in patients with bifurcation lesions in PRESTO was due in part to the “oculo-stenotic reflex” and in the other part to lesion and procedural factors (larger numbers of treated lesions, ostial lesions, lower stent use, and different techniques). The low TLR rate in our study may be ascribed to technical factors and the higher MACE rate to the prognostic impact of AMI. Whether drug eluting stents will overcome the technical challenges raised by bifurcation lesions remains debated. In the sirolimus bifurcation study by Colombo et al18, results were improved compared to bare-metal stents, with a 25.7% restenosis rate and an 8.1% TLR. However, routine side branch stenting was associated with a higher rate of restenosis compared to provisional side branch stenting (28% vs. 18.7%)18. In the recent Nordic Bifurcation study, a sirolimus-eluting stent only in the main branch produced similar clinical and angiographic results to routine stenting of both branches. These findings indicate that technical factors exert a major influence on outcomes even when drug-eluting stents are used, as confirmed by the recent analysis of the bifurcation subgroup of the ARTS II trial26.
In our study, location of the culprit lesion on a bifurcation had no impact on immediate or mid-term outcomes, most notably death, AMI and need for repeat revascularisation. The prognostic impact of bifurcation lesions is probably small compared to that of other factors (e.g., size of the infarction and time to revascularisation). A well-standardised technique designed to ensure complete revascularisation by preserving the side branches produces immediate and mid-term outcomes similar to those of non-bifurcation lesions.
Conclusion
This study of a single-centre database showed that angioplasty with bare metal stents of bifurcation lesions for AMI produced good immediate and mid-term outcomes when a well standardised provisional T-stenting technique was used. In the specific setting of AMI, involvement of a bifurcation by the culprit lesion dose not impact the prognosis.

