Abstract
Aims: To determine whether repeat revascularisation (RR) in diabetic patients treated with prior drug-eluting stents (DES) is the result of either DES restenosis or native progression of atherosclerotic disease in the coronary vasculature, and to evaluate the impact of atherosclerotic disease progression on the mid-term clinical outcome.
Methods and results: We followed 316 consecutive diabetic patients (227 men, age 69±9 years) treated between June 2005 and September 2006 with at least one DES. During the follow-up (mean 590±194 days) the cumulative incidence of major adverse clinical events (MACE; death, non-fatal myocardial infarction [MI] and target vessel revascularisation [TVR]) was 17.1%. Thirty-eight patients underwent RR (37 PCI, 1 coronary artery bypass graft [CABG]). In 22 patients RR was performed for restenosis (18 after DES implantation and 4 after BMS implantation); four of these patients also required treatment for atherosclerotic disease progression (ADP). In 16 patients, PCI was performed for symptomatic ADP without restenosis. Thus ADP contributed to 53% of RR procedures and to 42% of TVR. Furthermore, in 6 of 10 patients (60%) admitted for MI, the culprit lesion was the result of ADP. Only history of PCI and PCI of the left main before the index procedure were found to be independent predictors for development of significant de novo lesion at follow-up (OR 4.1, 95% CI 1.6-10.4, p=0.002 and OR 4.7, 95% CI 0,003, p=0.003). No traditional risk factors were found to be predictors.
Conclusions: Atherosclerotic disease progression was the cause of repeat revascularisation in more than 50% of diabetic patients treated previously with DES and had an important impact on their mid-term clinical outcome. MACE rates in clinical trials with long-term follow-up of diabetic patients can thus be influenced by native disease progression rather than DES failure and therefore should be interpreted with caution when addressing comparison of DES efficacy in diabetic patients.
Abbreviations
DES: Drug-eluting stent
BMS: Bare metal stent
RR: Repeat revascularisation
ADP: Atherosclerotic disease progression
MACE: Major adverse clinical events
MI: Myocardial infarction
TVR: Target vessel revascularisation
TLR: Target lesion revascularisation
CABG: Coronary artery bypass graft
PCI: Percutaneous coronary intervention
Introduction
Patients with diabetes are known to have an accelerated and more aggressive form of atherosclerosis and they have substantially higher rates of restenosis compared with nondiabetics.1,2 Drug-eluting stent (DES) implantation is effective in reducing clinical and angiographic restenosis in patients with diabetes mellitus.3,4 Nevertheless, the presence of diabetes mellitus remains an independent predictor of target lesion revascularisation (TLR) and is associated with unfavourable mid-term outcomes including higher rates of repeat revascularisation (RR).5-7 This higher risk of RR is attributed to restenosis and to the systemic nature of the disease and atherosclerotic disease progression (ADP). However, although current trials and registries have carefully evaluated major adverse cardiac events (MACE) after DES implantation, the impact of native ADP on MACE has not been well established.
The aim of this study was to assess the impact of ADP on mid-term outcome in real-world diabetic patients with previous DES implantation.
Methods
Study population
Our study included 318 consecutive diabetic patients who had received at least one DES between June 1, 2005 and July 31, 2006 at our institution. The database used in this study was developed in 2005 for the purpose of collecting information on all patients who undergo percutaneous coronary intervention (PCI) at our institution. The database contains information on demographics, coexisting conditions, left ventricular function, diseased vessels and vessels in which PCI was attempted, type or types of device used for each patient including bare-metal stents (BMS) and DES, quantitative coronary angiography (QCA) before and after intervention, and in-hospital adverse outcomes. Uniform definitions for these elements are used in the database.
This observational registry was based on current clinical practice; therefore only ordinary written informed consent to perform coronary intervention was obtained from all patients.
Procedural details
Interventional strategy and device use, including type of DES, were left to the discretion of the attending physicians. Quantitative coronary angiography (QCA) was used for luminal narrowing estimation before and after interventional procedure. Patients were pre-treated with aspirin (75 mg/day) and clopidogrel (600 mg followed by 75 mg/day). Weight-adjusted heparin (70 U/kg) was administered at the beginning of the procedure. Glycoprotein IIb/IIIa inhibitors were used according to operator decision and current guidelines. Dual-antiplatelet therapy was recommended for a period of 12 months.
Definitions and follow-up
The primary endpoint of the survey was the occurrence of MACE, defined as (1) death (cardiac and noncardiac), (2) nonfatal acute myocardial infarction (MI), (3) target-vessel revascularisation (TVR). MI during follow-up was diagnosed by a cardiologist at the hospital of admission according to standard criteria (rise in the creatine kinase level to more than twice the upper limit of the normal value with an increased creatine kinase-MB and/or newly developed Q waves). TVR was defined as any reintervention (surgical or percutaneous) to treat a luminal stenosis occurring in the same coronary vessel as the index procedure, within or beyond the target-lesion limits. Revascularisation for progressed atherosclerotic disease was defined as the need for PCI or CABG due to the development of a new lesion that was either not present or was not significant (less than 50%) during previous coronary intervention. In case of RR, all angiograms were reviewed by two different interventional cardiologists, who decided whether the patient had restenosis or ADP. Stent thrombosis within the stented segment was defined according the Academic Research Consortium (ARC) criteria.8 Follow-up data were obtained by hospital consultation and telephone contact in 316 patients (99.4%).
Statistical analysis
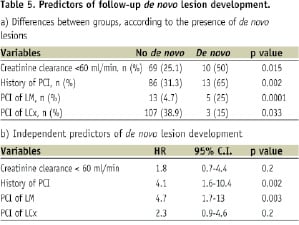
Continuous variables were expressed as mean±SD. Categorical variables were expressed as counts and percentages. The following covariates were first entered into the univariate regression models: age, gender, renal insufficiency (creatinine clearance <60 ml/min), hypertension, hypercholesterolaemia, history of smoking, insulin-dependent diabetes mellitus, history of MI, history of PCI, history of CABG, left ventricular ejection fraction, multivessel intervention and location of PCI. Covariates with p <0.1 were subsequently entered into a multivariate Cox regression model. A stepwise model selection method was further used to identify the significant independent predictors of survival, MACE and development of de novo lesions. A p value <0.05 was considered to indicate statistical significance.
Results
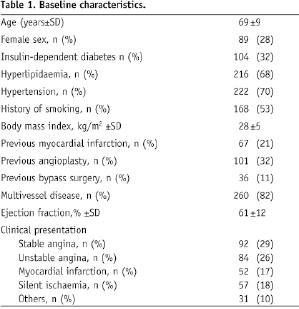
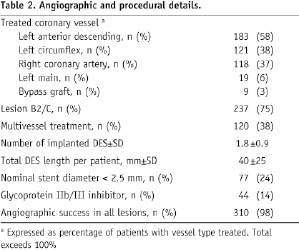
Of the 316 patients included, 273 (86%) were treated solely with DES, while 43 (14%) patients received both DES and BMS. Sirolimus-eluting stents were used in 185 patients, paclitaxel-eluting stents were implanted in 132 patients and zotarolimus-eluting stents in 5 patients. A total of 440 lesions were treated. Multivessel intervention was performed in 120 (38%) patients, and 14% of patients received peri-procedural glycoprotein IIb/IIIa inhibitors. Table 1 and Table 2 show the baseline demographic and angiographic characteristics of the study group.
Mid-term clinical outcome and impact of atherosclerotic disease progression
Patients were followed up for a mean of 590±164 days. The cumulative incidence of MACE was 17.1%. There were 21 (7%) deaths during the follow-up period (15 cardiac, 5 noncardiac, 1 unknown cause), 10 nonfatal MIs and 28 patients required TVR. According to ARC criteria no definitive stent thrombosis (ST), 1 probable late ST, 3 possible late ST and 1 possible very late ST occurred during follow-up.
In 38 patients, RRs were performed during follow up (37 PCI, 1 CABG) (Table 3).
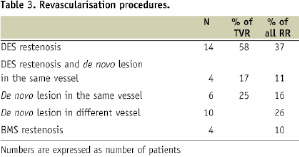
RR was performed for restenosis of the last PCI in 22 patients (18 after DES implantation, 4 after BMS implantation); 4 of these patients also required treatment for ADP. In 16 patients, PCI was performed for symptomatic ADP without restenosis. Thus, a total of 42 lesions (22 restenosis [18 DES, 4 BMS] and 20 ADP) were treated in 38 patients. Among patients treated for ADP, 10 had a de novo lesion in a vessel that had not previously been treated. The other 10 patients had de novo lesions within the previously treated vessel, but in segments remote from the target site. ADP contributed to 53% (20/38) of RR (16 patients with de novo lesions and 4 patients with de novo lesions along with restenosis). Furthermore, by treating 10 de novo lesions in previous target vessel, ADP contributed to 42% (10/24) of TVR. ADP in vessels remote from the previous target vessel represented 26% (10/38) of RR. In patients with MI, culprit lesions remote from the target site were identified in 6 of 10 patients (60%). Excluding events caused by atherosclerotic disease progression resulted in a MACE rate of only 12.3% (absolute MACE reduction of 4.8%).
Predictors of MACE and atherosclerotic disease progression
Univariate and multivariate analyses were performed to identify the predictors of MACE at follow-up. Age, renal insufficiency, left ventricle ejection fraction, history of MI, history of CABG, PCI of the left anterior descending coronary artery (LAD) and PCI of bypass graft were identified as univariate predictors (Table 4).
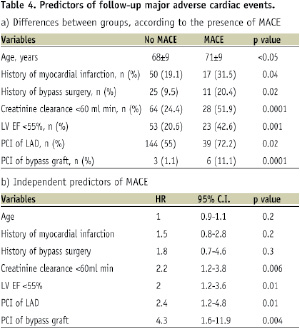
Of these predictors, renal insufficiency, ejection fraction < 55%, PCI of LAD and PCI of bypass graft were found to be independent predictors for follow-up MACE.
Previous PCI, previous PCI of the left main or of the left circumflex artery and renal insufficiency were identified as univariate predictors for the development of de novo lesions. Of these predictors, only previous PCI and PCI of the left main were found to be independent predictors for development of significant de novo lesions at follow-up (Table 5).
HbA1c level at the time of PCI (7.2±1.3%) was not a predictor of either ADP or MACE at follow-up.
Discussion
This study has demonstrated that in a real-world diabetic population treated with DES, mid-term clinical outcome is influenced by either restenosis or coronary artery disease progression. Repeat intervention and TVR were required because of ADP at the same frequency as revascularisation for restenosis. Furthermore, culprit lesions in patients who presented with MI were caused by ADP and not by restenosis in the majority of cases.
Recently, published results of a meta-analysis of randomised trials and large real-world registries, which studied long-term clinical outcome of DES compared to BMS, have shown no differences in death and MI during follow up.9,10,14 The presence or absence of diabetes did not alter the effect of any stent on the incidence of death or MI.9 DES efficiently reduces the need for new revascularisation compared to BMS, however in the large registry reported by Marzocchi et al,10 diabetes was a strong predictor of TVR (36% increase in TVR risk). Other studies have also found a trend toward a higher frequency of restenosis and repeat intervention in diabetic patients compared to nondiabetic patients in the DES era, which has worsened outcomes in this high-risk group of patients.11,12 ADP is often cited as a major reason for these unfavourable outcomes. The first study in the DES era that addressed the impact of ADP after DES implantation in diabetics was performed by Jiménez-Quevedo et al,14 who showed that ADP was responsible for 50% of the total revascularisation rate at 2 years. However, the study group was very small; only selected patients were included and the study did not show the impact of disease progression on MACE, a typically reported outcome. We have evaluated the impact of ADP on a large cohort of diabetic patients in a real-world setting, the first such study in the DES era. In agreement with the findings of Jiménez-Quevedo, we found that ADP contributed to 50% of all RR during follow-up. After more detailed analysis, we have demonstrated that ADP has a major influence on TVR due to the development of new lesions in the same vessel remote from the target site. Thus, it seems essential to carefully distinguish TVR from TLR when evaluating the efficacy of DES in diabetic patients. Furthermore, angiographic examination of patients admitted for MI showed that ADP was responsible for the culprit lesion in 60% of patients. This confirms the need for precise analysis of MACE after DES implantation in diabetic patients. Excluding events caused by disease progression resulted in a MACE rate of only 12.3% (absolute MACE reduction of 4.8%). This fact may also explain the unequivocal results of long-term clinical outcomes in diabetic patients seen in head-to-head comparisons of different types of DES.15-18 There is one limitation in evaluating MACE. This is a clinically driven study and TVR could be much more frequent in angiographic studies especially in diabetic patients. Interestingly, none of the traditional risk factors and only previous PCI and PCI of the left main were found to be independent predictors for clinical onset of significant de novo lesions. This can be explained by the presence of a more advanced stage of coronary artery disease with a subsequent more rapid evolution. By more detailed evaluation of angiograms, we found that these independent factors could be related to a more diffuse pattern of coronary disease and risk profile of these patients. The need for PCI is a marker of coronary disease progression and/or poor control of risk factors, since patients continue to have coronary events despite treatment. Also, left main disease is rarely isolated and is often related to multivessel disease; at the index angiogram most patients with PCI of the left main who presented with de novo lesions already had mild stenosis or lesions (<50% stenosis) in the three main coronary arteries. This supports a non-selective aggressive approach to secondary prevention of coronary artery disease in diabetic patients. Two recent studies have clearly demonstrated the benefit of an intensified multifactorial intervention -with behaviour modification, tight glucose regulation and the use of renin-angiotensin system blockers, aspirin, and lipid-lowering agents- in diabetic patients to reduce the risk of cardiovascular complications and also the risk of death.19,20 These data suggest that the quality of the pharmacological intervention will impact mid- and long-term clinical outcomes after DES implantation in diabetic patients, and should be carefully evaluated in DES comparison studies to avoid any misinterpretation about DES clinical efficacy.
Conclusion
Based on our findings, it seems to be very important to interpret mid-term DES safety and efficacy in diabetic patients with caution and to consider the aggressive and diffuse nature of atherosclerotic disease in this population. Future randomised trials should evaluate the effect of both pharmacological interventions and glycemic control when assessing the causes of MACE after DES implantation in diabetic populations.
Acknowledgements
The authors acknowledge the support of Boston Scientific Corporation Inc. in the data analysis, as well as Mrs. Alison McTavish who kindly revised this paper.

