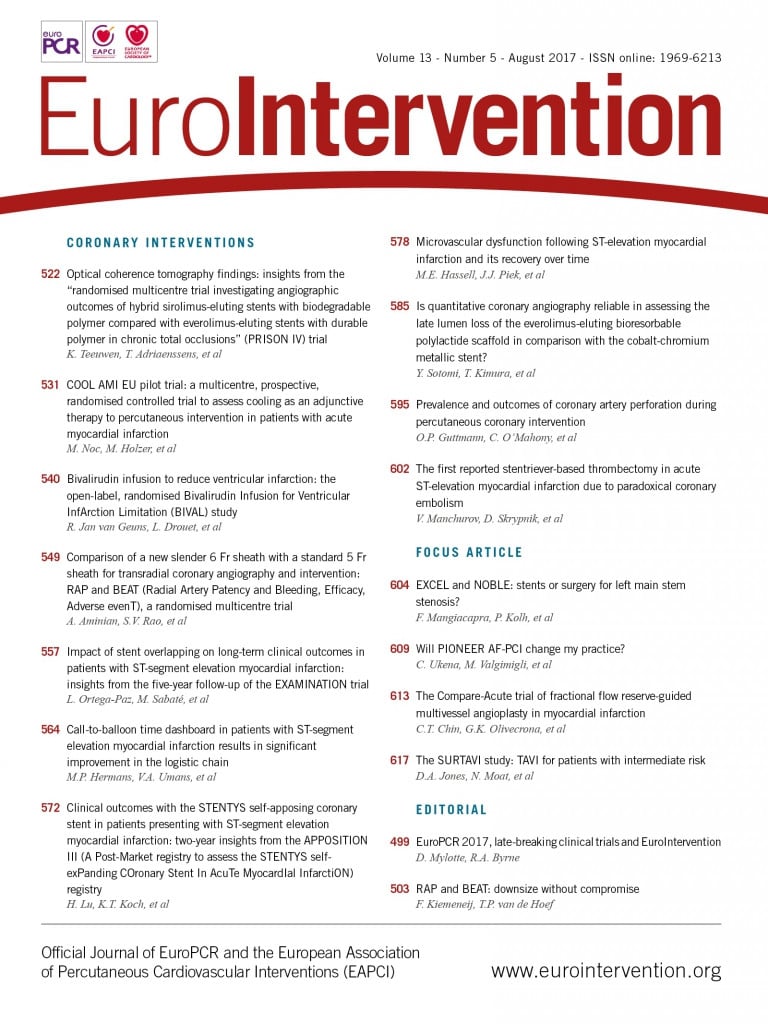
In this edition of EuroIntervention we publish reports from three late-breaking clinical trials presented at EuroPCR 2017 and simultaneously published online in EuroIntervention1-3. In addition, three other late-breaking trial reports from single-arm studies also simultaneously published online appeared in print in our July issue4-6. Each year, through our co-operation with the Scientific Programme Committee of EuroPCR, the editors of EuroIntervention invite the authors of selected presentations to submit a full original manuscript for expedited review, with the aim of publishing accepted manuscripts online at the time of presentation. The potential to publish online concurrent with abstract presentation is attractive for readers, authors, and publishers alike.
It affords the reader an immediate opportunity to assess in depth the findings of an abstract presentation, allows authors to release their observations to the community immediately, and is in line with the mission of the scientific press to disseminate new data in a timely manner. We will continue to promote and expand this service to our readers and authors in the years to come and look forward to being able to publish more and more high-quality research in interventional cardiology in an expedited fashion at the time of the annual EuroPCR meeting. Indeed, this initiative builds on our existing commitment to timely publication of scientific findings through expedited editorial publications (EEP) for selected high-impact papers, as well as immediate online publication of all other accepted manuscripts as just accepted articles (JAA).
In the first report in the current issue, Koen Teeuwen and colleagues present an optical coherence tomography (OCT) substudy from the randomised PRISON IV trial, which compared a novel thin-strut sirolimus-eluting stent (SES) with biodegradable polymer (Orsiro; Biotronik, Bülach, Switzerland) to an established thin-strut second-generation everolimus-eluting stent (EES) with durable polymer (XIENCE®; Abbott Vascular, Santa Clara, CA, USA) in patients undergoing recanalisation of chronic total occlusions (CTO)1. Few studies have compared various new-generation DES in this specific lesion subset, and thus the current study affords a unique opportunity to understand more about the impact of stent design in challenging CTO anatomy often characterised by long areas of diffuse disease and extensive calcification. In the main PRISON IV trial report, the hypothesis that SES would be non-inferior to EES in terms of angiographic antirestenotic efficacy in this challenging lesion subset could not be proved7. The primary endpoint of in-segment late lumen loss was 0.13±0.63 mm for SES compared to 0.02±0.47 mm for EES (mean difference 0.11 mm, 95% confidence interval [CI]: –0.01 to 0.25 mm; pre-specified non-inferiority margin 0.20 mm, pnoninferiority=0.11). Moreover, angiographic in-stent/in-segment binary restenosis was higher with the SES compared to the EES (8.0 vs. 2.1%, p=0.028).
In the current substudy of 117 patients enrolled at two of the participating study centres, 108 underwent angiographic follow-up at nine months, and 71 were selected for OCT imaging, 60 of whom had analysable data1. The main findings were that, in these selected patients, morphometric measures of stent and lumen diameter as well as neointimal thickness were similar in both groups. Moreover, while the number of uncovered struts was higher with EES (6.2±7.5% and 11.9±13.4%, p=0.04), the number of malapposed struts and the mean number of coronary evaginations were higher with SES (2.9±4.0% and 1.2±2.4%, p=0.02; 18.5±17.7 and 5.3±3.1, p=0.004).
The authors should be congratulated for undertaking systematic OCT analysis of an interesting patient subgroup, which comprises an increasing proportion of the patients treated in daily practice8,9. Indeed, the findings are of interest for a number of reasons. For example, although the relevance of stent evagination on OCT is unclear, increased incidence might represent a warning signal for increased risk of stent thrombosis10. The higher rates observed with SES might be of particular relevance in challenging CTO anatomy where long segment stenting is often performed and stent thrombosis risk is increased. However, the precise mechanism of evagination and malapposition in this study remains unclear, and serial OCT data incorporating post-implantation data were not available. Moreover, the data are somewhat at odds with prior OCT surveillance studies comparing both stents, which did not detect any difference11. On the other hand, the findings are unable to explain the difference in angiographic antirestenotic efficacy observed in the main study. A number of important limitations must be considered when interpreting the results. Specifically, the external validity of the observations is limited by the impact of patient selection and the enrolment of patients with relatively straightforward CTO lesions (lower mean J-CTO score, higher percentage of lesions treated with anterograde wire escalation, and higher success rate of intervention compared with recent CTO registry reports12). Ultimately, larger-scale studies with longer-term follow-up will be required to investigate whether important differences exist between contemporary new-generation DES devices in patients treated for CTO.
In a second paper, Marko Noc et al report the results of the COOL AMI EU pilot randomised trial, investigating the feasibility and safety of rapid induction of therapeutic hypothermia in patients with anterior ST-elevation myocardial infarction (STEMI)2. Therapeutic hypothermia aims to reduce the impact of myocardial reperfusion injury and appears to attenuate infarct size in experimental models13-15. However, clinical trials have provided mixed results to date, in terms of both clinical outcomes and infarct size16-18, and the place of this intervention outside of resusciated cardiac arrest is uncertain at present19. However, subgroup analyses of prior data have suggested benefit in early presenters with anterior STEMI who were cooled effectively prior to reperfusion20. In the present COOL AMI EU pilot study, therefore, 50 patients with anterior STEMI within six hours of symptom onset were randomised to rapid cooling, achieved by the controlled central infusion of cold saline for the duration of PCI and three hours post intervention using the ZOLL® Proteus™ Intravascular Temperature Management System (ZOLL Medical Corporation, Chelmsford, MA, USA), or standard therapy. Cardiac magnetic resonance (CMR) imaging was performed at four to six days to assess infarct size.
The results show that hypothermia was successfully and rapidly induced with the Proteus system – tympanic (33.6°C) and core (33.0°C) temperatures after about 20 minutes of cooling. Among those undergoing cooling, the incidence of new atrial fibrillation was numerically increased (32% vs. 8%, p=0.07), a finding not observed in any of the previous cooling studies. Left ventricular ejection fraction (42% vs. 40%) and infarct size/left ventricular mass (16.7% vs. 23.8%) were similar between groups. Two patients in the test group had acute/subacute stent thrombosis, a potential concern. From a methodological point of view, the study of Noc et al has important limitations, including the small sample size and absence of a clear clinical hypothesis. Moreover, incomplete data are presented on CMR, and it would be important to know about additional parameters including myocardial salvage, microvascular obstruction, etc. Finally, as anticipated from the study design, time from randomisation to reperfusion was significantly longer among patients undergoing the cooling protocol (+17 minutes [95% CI: 4.6-29.8 minutes]), and it is important to assess lack of benefit in terms of this potential risk. The COOL AMI EU pilot study is an important foundation stone for a large prospective randomised trial of this intervention using a device capable of rapid and effective cooling. Only results from this type of trial can provide further insight into the role of systematic cooling in STEMI patients.
Finally, in the third trial report, Robert van Geuns and colleagues report the primary results of the Bivalirudin Infusion for Ventricular InfArction Limitation (BIVAL) randomised trial3. In this multicentre, open-label trial, patients undergoing primary angioplasty for STEMI were randomised to a four-hour bivalirudin infusion or unfractionated heparin (UFH), with a primary endpoint of infarct size, assessed by CMR five days post intervention. Secondary endpoints included invasive microcirculatory resistance and CMR-assessed microvascular obstruction.
An interim analysis of the day-5 CMR data after enrolment of 78 of a planned 200 patients demonstrated no significant between-group difference in the primary endpoint (infarct size: bivalirudin 25.0±19.7% vs. UFH 27.1±20.7%; p=0.75), and the study was terminated for futility. Interestingly, microcirculatory resistance was lower with bivalirudin than UFH (43.5±21.6 vs. 68.7±35.8 mmHg, p=0.014), while CMR microvascular obstruction was comparable in both groups. Clinical outcomes and bleeding events were similar between groups.
The authors should be commended for undertaking a randomised trial aiming to provide novel mechanistic insight into the comparative efficacy differences observed in some trials comparing bivalirudin and UFH in patients with STEMI21, as well as for pursuing analysis and publication of a negative trial terminated for futility. Indeed, the observations in relation to the differences observed in some of the secondary endpoints deserve further investigation. Nevertheless, important limitations in study design should also be acknowledged when interpreting the results. Foremost among these is that the assumptions on which the test hypothesis was based are not clearly supported by prior published literature. The authors do not clearly describe the basis for the assumption that bivalirudin could reduce infarct size by 23% in comparison to UFH. A CMR substudy from HORIZONS-AMI failed to show any benefit with bivailrudin versus UFH plus abciximab in terms of infarct size within seven days or at six months22, and abciximab versus placebo had shown only a small magnitude effect in infarct size reduction by CMR in another randomised trial23. In addition, in common with other studies in this field, it is difficult to interpret treatment effects with bivalirudin versus UFH when the overwhelming majority of patients had already been treated with heparin prior to randomisation. For the moment, UFH remains the anticoagulant of choice for most patients with STEMI around the world. Nevertheless, van Geuns and colleagues provide a further piece of evidence in the long-running saga of bivalirudin and UFH and do our community some service by the publication of negative trial results, a vital part of the landscape of evidence-based medicine.