Abstract
Aims: The aim of the current study was to compare the short and mid-term outcome between males and females treated with percutaneous coronary intervention (PCI) with bare metal stent implantation or coronary artery bypass graft (CABG) surgery and drug-eluting stent implantation in the Arterial Revascularisation Therapies Study I and II (ARTS I and II).
Methods and Results: The patients included in ARTS I were randomised to PCI with bare metal stents or to CABG. The patients enrolled in ARTS II were treated with Cypher™ stent implantation. All patients were scheduled for clinical follow-up at one, six and twelve months, and after three and five years. Major adverse cardiac and cerebrovascular events (MACCE) included death, cerebrovascular accident (CVA), myocardial infarction (MI), repeat target vessel PCI (RPCI) and CABG. At one and three-year follow-up in ARTS II, both the female and male patients had an incidence of MACCE similar to ARTS I-CABG. When comparing the female and male population of ARTS II, there were no differences between the two genders in terms of in-hospital outcome. At one year and three years there were no gender specific differences in the incidence of MACCE.
Conclusions: Female and male patients in ARTS II had significantly lower MACCE rates compared with ARTS I-PCI, but similar to that of ARTS I-CABG. In ARTS II, MACCE free survival was similar for the two genders at three years follow-up.
Introduction
Although coronary artery disease is the leading cause of death in both genders, its prevalence and impact on women’s health has been only recently recognised1. In most clinical trials evaluating optimal coronary revascularisation strategies, women are consistently under-represented, with the majority including no more than 30% of females2-5. As a consequence, women were treated on evidence extrapolated from studies mainly based on male populations, even though it was observed that certain risk factors constituted a greater risk for women than men, and that women who sustained coronary events had less favourable outcomes than their male counterparts.
From the 1980s and the early 1990s studies comparing gender-related differences following coronary revascularisation procedures demonstrated higher in-hospital mortality, lower procedural success rates and higher complication rates in women6. However, more recent studies showed a general improvement in overall success rates in women submitted to PCI, despite the fact that they had more comorbid factors7-9. Similar results have been reported after CABG10.
ARTS I was designed to compare CABG and PCI with bare metal stent implantation for the treatment of patients with multivessel disease11. The study demonstrated a similar early and long-term outcome between female and male subjects. The only difference observed was an increased risk of bleeding complications in women treated with PCI. In both genders of the ARTS I population, treatment with CABG was associated with a lower incidence of MACCE compared to PCI at five years12.
The introduction of drug-eluting stents for the treatment of coronary artery disease has resulted in significant reductions of angiographic and clinical restenosis13,14. In the recently published ARTS II study it was reported that the overall MACCE rate at one year was similar to that of the ARTS I-CABG arm and significantly reduced when compared to the ARTS I-PCI arm15. The aim of the current study was to compare the short and mid-term outcome between males and females treated with bare metal stent implantation or CABG and sirolimus-eluting stent implantation in ARTS I and II.
Methods
Study design
ARTS II is a multicentre, non-randomised, open-label study, which was designed to evaluate sirolimus-eluting stent (Cypher™ stent, Cordis, Warren, NJ, USA) implantation in patients with multivessel coronary artery disease15. The study population randomised to either PCI with bare metal stents (Crown™ or CrossFlex™ stent, Cordis, Warren, NJ, USA) or to surgical revascularisation in ARTS I was used as a historical control11. Inclusion and exclusion criteria were identical in both studies. In order to ensure the comparability of the populations and the inclusion of at least 1/3 of patients with three-vessel disease, stratification was done by clinical site and enrolment was accomplished via a central telephone service. The treatment decisions were left to the operators’ discretion. The study stents had a diameter of 2.5 to 3.5 mm and a length of 13 to 33 mm. All patients were scheduled for clinical follow-up visits including an ECG at one and six months, and subsequently at one, three and five years.
Each participating centre’s ethical committee approved the study. Written informed consent was obtained before the procedure.
Study population
The study population consisted of patients with stable or unstable angina or silent ischaemia and at least two new significant lesions (>50% diameter stenosis) one of them located mandatorily in the left anterior descending artery (LAD), and the other in a different major epicardial vessel. Exclusion criteria were left main disease, the presence of more than one total occlusion, a history of previous coronary intervention, severe congestive heart failure or a left ventricular ejection fraction less than 30%. Also excluded from the study were patients with a history of cerebrovascular accident, transmural myocardial infarction in the preceding week, severe hepatic or renal disease, neutropenia or thrombocytopenia, intolerance or contradiction to acetylsalicylic acid or thienopyridines, the need for concomitant major surgery and life-limiting concomitant non-cardiac disease. Patients were divided into two groups according to gender.
Study objectives
The primary aim of this analysis was to assess the 30 day, one year and three years clinical outcome of the female patients enrolled in ARTS I and ARTS II and to determine whether it is comparable with that of the male patients. The secondary objective is to evaluate any differences in the one year and three years outcome between women and men in ARTS II.
Endpoint definitions
Death from all causes were reported, and categorised as cardiac unless there was documentation to the contrary. Cerebrovascular events (CVA) included: stroke, transient ischaemic attacks, and reversible ischaemic neurological deficits. Within seven days after the intervention, a diagnosis of MI was made if new abnormal Q-waves (according to the Minnesota code) developed and either a ratio of serum creatinine kinase MB (CK-MB) isoenzyme to total cardiac enzyme was greater than 0.1 or a CK-MB value that was 5 times the upper limit of normal was present. Serum creatinine kinase levels were measured six and 12 hours after the intervention and before discharge. Beginning eight days after the procedure, either new abnormal Q-waves or enzymatic changes were sufficient for diagnosis of MI. This specific method of defining myocardial infarction was developed for ARTS I to address the difficulty of diagnosing a myocardial infarction after surgery11. A myocardial infarction was confirmed only after the relevant electrocardiograms had been analysed by the electrocardiographic core laboratory and adjusted by an independent clinical event committee. Stent thrombosis was defined according to the ARC consensus criteria16. All repeat revascularisation procedures were recorded. Events were counted from the time of the start of the initial procedure. MACCE included death, CVA, MI, repeat target vessel PCI (RPCI) and CABG.
Endpoint measurement
In ARTS I, the patients were randomised after informed consent was obtained and thereafter they entered a waiting list. In ARTS II, the patients were submitted to coronary revascularisation within 48 hours after inclusion. In order to compensate for the temporal difference since allocation between ARTS I and ARTS II, events for the present report were counted from the time of the procedure for all the patients and not from the time of allocation as previously reported12.
Statistical analysis
Demographic and procedural characteristics of female patients were compared between ARTS II and ARTS I (CABG and PCI) and a similar comparison was performed for the males. Continuous variables are expressed as mean ±standard deviation. Categorical variables are presented as counts and percentages. The F-test from a one-way analysis of variance for continuous variables and the Fisher’s exact test for categorical variables were used.
MACCE at 30 days, one-year and three years are presented as counts and percentages and were compared in terms of relative risks (ARTS II vs. both ARTS I arms) with 95% confidence intervals. For the analysis of stent thrombosis in the ARTS II population at three years follow up, the Fisher’s exact test was used. Stent thrombosis is presented as counts and percentages. Time-to-event variables are presented as Kaplan-Meier curves, and the overall incidence was tested using the log-rank test.
Results
In ARTS I, 1,205 patients (283 female and 922 male) were randomised to either percutaneous or surgical coronary revascularisation between April 1997 and June 1998 and in ARTS II 605 patients (142 female and 465 male) were enrolled between February and November 2003 at 45 participating centres.
Baseline characteristics
Table 1 and 2 present the baseline demographic and angiographic characteristics of the three treatment groups in female and male patients. Comorbidities such as hypercholesterolaemia, diabetes and hypertension include also treated patients.
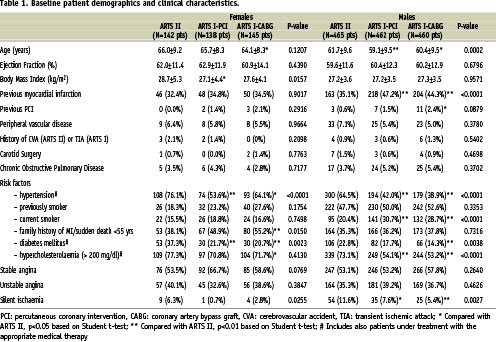
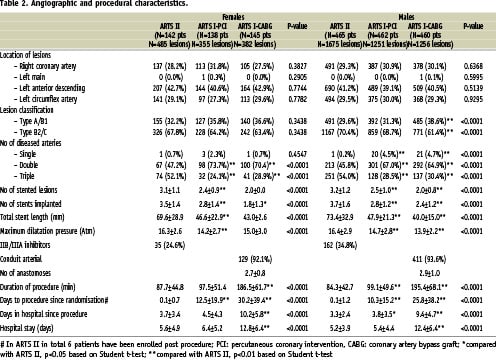
Female patients in ARTS II had a significantly higher percentage of diabetes mellitus and hypertension compared with ARTS I female patients. The percentage of three-vessel disease was 52.1% in the ARTS II female cohort vs. 24.1% in ARTS I-PCI (p<0.001) and 28.9% in ARTS I-CABG (p<0.001) female group. The mean number of significant lesions per female patient was 3.4 + 1.2 in ARTS II vs. 2.7 + 0.9 in ARTS I-PCI (p<0.001) and 2.7 + 0.9 in ARTS I-CABG (p<0.001).
The ARTS II male population had a significantly higher percentage of patients with hypertension and hypercholesterolemia compared with the respective ARTS I-PCI and ARTS I-CABG population. However, significantly fewer male patients were current smokers in ARTS II compared with ARTS I-PCI and ARTS I-CABG male patients. The percentage of three-vessel disease was 54.0% in ARTS II male patients vs. 28.5 in ARTS I-PCI (p<0.001) and 30.4% in ARTS I-CABG (p<0.001). The mean number of significant lesions per male patient was 3.6 + 1.3 in ARTS II vs. 2.8 + 1.0 in ARTS I-PCI (p<0.001) and 2.8 + 1.0 in ARTS I-CABG (p<0.001).
Female versus male patients in ARTS II
Female patients were older than male patients (66.0±9.2 years vs. 61.7±9.6 years, p<0.001), had a higher incidence of diabetes mellitus (37.3% vs. 22.8%, p=0.001), hypertension (76.1% vs. 64.5%, p=0.011) and obesity (Body Mass Index: 28.7±5.3 kg/m2 vs. 27.2±3.6 kg/m2, p<0.001). On the other hand female patients had a better ejection fraction (62.0±11.4% vs. 59.6±11.6%, p=0.049) and a lower rate of previous smoking habit (18.3% vs. 47.7%, p<0.001). The angiographic and procedural characteristics were similar for the two genders, except that more male patients were treated with IIb/IIIa inhibitors during the PCI (34.8% vs. 24.6%, p=0.024).
Short-term clinical outcome in female and male patients in ARTS I and ARTS II
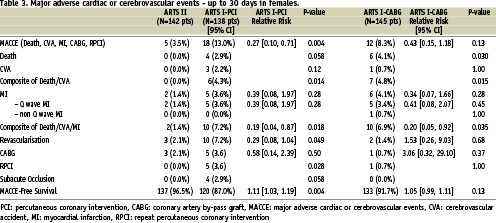
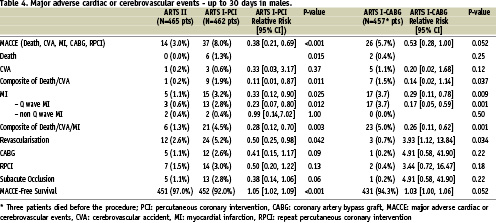
Up to 30 days, there were no deaths observed in the ARTS II female patients, whereas six deaths were reported in the female surgical cohort of ARTS I (0% vs. 4.1%, p=0.030). However the incidence of total MACCE was similar between the two groups (3.5% vs. 8.3%, p=0.13), but lower than that of the females patients enrolled in ARTS I-PCI (Table 3). Likewise, there were no differences in the incidence of MACCE between the males in ARTS II and those assigned to ARTS I-CABG (3.0% vs. 5.7%, p=0.052), although the incidence of MACCE was lower compared with the male arm of ARTS I-PCI (3.0% vs. 8.0%, p<0.001) (Table 4).
One-year and three-year clinical outcome in female and male patients in ARTS I and ARTS II
Both at one and three-year follow-up, the incidence of MACCE in the female patients of ARTS II was similar to the female population enrolled in ARTS I-CABG, but lower than the female population treated percutaneously in ARTS I (Tables 5, 6 and Figure 1). Interestingly, up to 365 days women assigned to both the surgical and interventional arm of ARTS I had a higher incidence of death compared to ARTS II (6.2% vs. 0.7%, p=0.019 and 5.8% vs. 0.7%, p=0.018, respectively). However, at three years, this difference diminished (6.9% vs. 2.8%, p=0.17 and 7.2% vs. 2.8%, p=0.11, respectively). Additionally, both at one year and three years, female patients in ARTS II had fewer repeat revascularisation procedures compared with the female population enrolled in ARTS I-PCI (6.3% vs. 20.3%, p<0.001 and 10.6% vs. 24.6%, p=0.003, respectively). Similar results were observed in the male population. In ARTS II, male patients had a similar incidence of MACCE compared to the surgical arm in ARTS I but lower compared with ARTS I-PCI (Tables 7, 8 and Figure 2). Up to 365 and 1,080 days male patients assigned to ARTS I-CABG and ARTS I-PCI had more myocardial infarctions compared with ARTS II (Tables 7 and 8). Furthermore, both at one and three years follow-up, male patients in ARTS II had fewer repeat revascularisation procedures compared with the male population of ARTS I-PCI (9.0% vs. 21.2%, p<0.001 and 15.5% vs. 26.8%, p<0.001, respectively) but more when compared to ARTS I-CABG (9.0% vs. 4.2%, p<0.003 and 15.5% vs. 6.6%, p< 0.001, respectively).
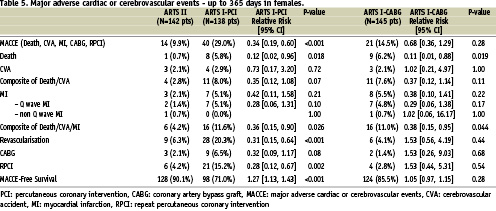
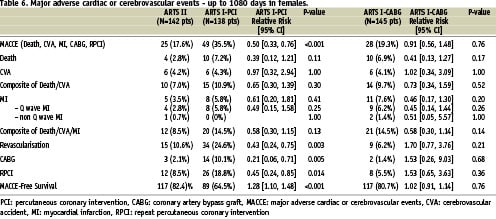
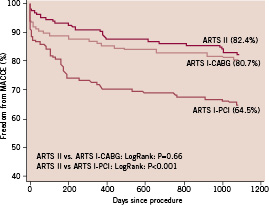
Figure 1. Kaplan-Meier curves out to three years in female patients in ARTS I and ARTS II population.
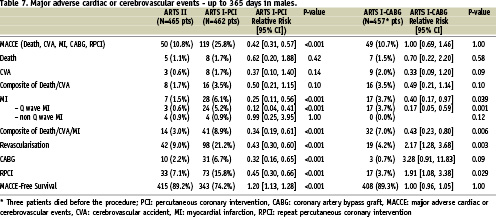
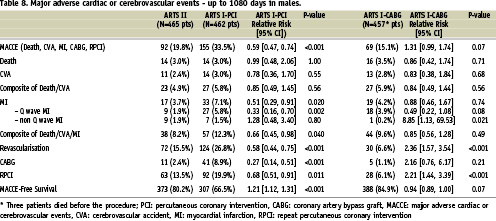
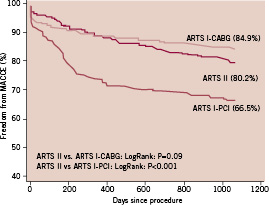
Figure 2. Kaplan-Meier curves out to three years in male patients in ARTS I and ARTS II population.
Three-year clinical outcome in ARTS II (female versus male patients)
There were no differences between the two genders in terms of in-hospital outcome. Furthermore, at 30 days, one year and three years there were no gender specific differences in the incidence of MACCE and stent thrombosis (Tables 9, 10, 11, 12 and Figure 3).
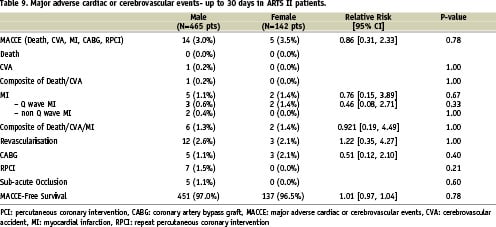
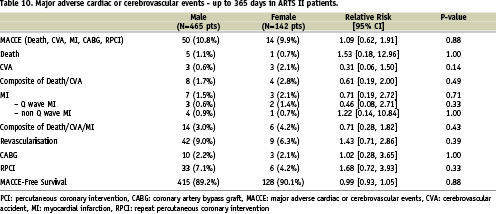
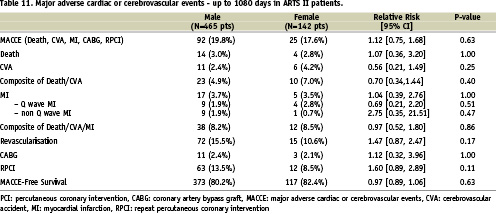
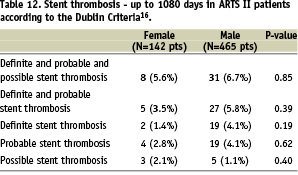
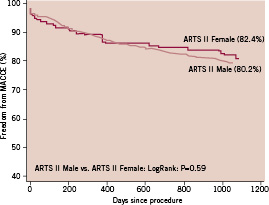
Figure 3. Kaplan-Meier curves out to three years in female and male patients in ARTS II
Discussion
Patients in ARTS II had more adverse baseline characteristics compared with those in ARTS I. However, despite this fact the following observations were made: 1) Up to 30 days, both the female and male population in ARTS II had a clinical outcome similar to the respective population in the surgical arm of ARTS I, and a better outcome than the interventional group of ARTS I; 2) These results were sustained up to three years; 3) In ARTS II, there was no difference between the two genders in terms of 30 days outcome and three year incidence of MACCE.
Gender differences
The differences between males and females with coronary artery disease treated with percutaneous or surgical revascularisation were highlighted in previous studies. Women were found to have more comorbid factors, greater functional impairment and worse anginal status17-20. Furthermore, it was observed that female patients tend to have smaller coronary vessels than male patients, rendering percutaneous or surgical revascularisation more difficult21. In accordance, the female population of ARTS II had more adverse baseline characteristics compared with males. Women were older and more likely to have diabetes mellitus, hypertension and obesity.
Gender and PCI
Despite the fact that women had more risk factors than men in ARTS II, they had a similar incidence of MACCE at thirty days, one year and three year follow-up. These findings confirm that there were no gender-specific differences in the incidence of MACCE12 in ARTS I at five-years . Improvements in the clinical outcome after PCI in women were observed in other recent studies8,22-24. The National Heart, Lung, and Blood Institute’s 1993- 1994 PTCA Registry shows that women at higher risk undergoing PCI had high clinical success and low complication rates23. An analysis of 1,908 women from a pooled data set of 6,186 patients showed that stenting can be performed in women with an excellent short- or long-term outcome comparable to that of men8. Notably, a study from Munich that included in total 1,025 women and 3,349 men treated with PCI with bare metal stents demonstrated that compared with men, women had a lower risk of restenosis in spite of a more prominent presence of diabetes and small vessel size22. The improved outcome observed in the female population may mirror increased operator experience, technology advancements, better procedural strategy or understanding of gender specific issues for revascularisation.
The impact of sirolimus-eluting stent
Despite more extensive and complex coronary artery disease in ARTS II both female and male patients had a similar mid-term MACCE-free survival compared to ARTS I-CABG and significant higher MACCE-free survival compared to ARTS I-PCI. Furthermore, women benefited as much as men in the reduction of late revascularisation with sirolimus-eluting stents in comparison with bare-metal stents, even if they started with worse clinical conditions. This is in contrast with TAXUS IV results, where women compared with men had higher one-year rates of target lesion revascularisation25.
The anti-restenotic effects of drug-eluting stents has been demonstrated in several randomised trials13,14,26. The benefits of the sirolimus-eluting stent in terms of reducing clinical and angiographic restenosis appear to be applicable to both genders26. The findings of the ARTS II gender subsets are in accordance with these results. The need for repeat revascularisation was reduced for women and men from 24.6% and 26.8% respectively in ARTS I-PCI to 10.6% and 15.5% in ARTS II. It is noteworthy that women in ARTS II had the tendency to less revascularisations at three years (10.6% versus 15.5%) than men, despite the fact that the female population had more risk factors than the respective male group. This may be due to difference in plaque composition. Interestingly, ARTS I-CABG still had the lowest need for revascularisation in men (6.6%) at three-year follow-up. Nevertheless, the 15.5% repeat revascularisation rate at three years that was reported in the ARTS II male population is lower than the rates observed in randomised historical trials, which compared either balloon angioplasty or bare metal stent implantation with CABG in patients with multivessel coronary artery disease2,27,28.
Study limitations
The current study is a sub-analysis of the main ARTS I and ARTS II trials. Thus, it has inherent limitations, such as the lack of sufficient power due to the limited number of patients in the subgroups. Therefore, definite and generalised conclusions cannot be drawn. Additionally, the study is non-randomised and a five-year interval exists between the patients enrolled in ARTS I and ARTS II. Hence the groups are not directly comparable, since interventional and surgical techniques and mortality rates have been improving during the last years.
One could postulate that a possible bias of the study lies in the fact that in ARTS II the patients were not discussed with the surgeons prior to the intervention; even though the protocol required that the lesions were also treatable by CABG. This could potentially lead to the enrolment of technically simpler two- or three-vessel disease patients than those treated in ARTS I. However, this is unlikely since the ARTS II population consisted of patients with more cardiovascular risk factors, more three-vessel disease and an increased number of significant lesions, who received more and longer stents. Furthermore, patients in ARTS II had more type C lesions.
Finally, the results of the present study are limited to three-year follow-up. Whether the favourable long-term outcome will be sustained in both genders with multivessel coronary artery disease after sirolimus-stent implantation in patients is not yet known. Recent reports on late stent thrombosis have indicated a constant stent thrombosis rate of 0.6% per year29. This may have an unfavourable impact on the long-term MACCE. However, there is no data indicating that stent thrombosis will affect more women than men.
Conclusion
Although female and male patients in ARTS II had more adverse baseline characteristics than those in ARTS I, in both groups the MACCE rate was lower than in ARTS I-PCI and similar to that of ARTS I-CABG. Furthermore, women had a higher surgical mortality at 30 days and good short and mid-term results with drug-eluting stent implantation. Additionally, the female patients enrolled in the ARTS II study were older and had more risk factors compared with the male patients. However, the MACCE rate was similar between the two groups during the 30 days, the one-year and three years follow-up period. These findings indicate that PCI with drug-eluting stents may be considered as a first choice procedure for coronary revascularisation in women.
The outcome in both genders treated with sirolimus-eluting stent implantation was significantly improved. This improvement observed in both genders may reflect the fact that sirolimus-eluting stents effectively neutralize the impact of the adverse factors that in the past hampered short- and long-term results.

