In our last two columns we spoke about the basis of our association, its history and general goals, in this article we update the situation concerning the EAPCI and its involvement in the nuts-and-bolts discussions that are laying the groundwork for subspecialty education and accreditation in Europe today.
Within Europe there are two primary boards working towards the accreditation, harmonisation and coordination of cardiology education and training. In education, it is the European Board for Accreditation in Cardiology (EBAC) which offers an “independent professional peer delivered accreditation of educational events and products” recognised by 19 national professional medical societies within Europe. In training, the EACPI is an active member of the European Board for the Specialty of Cardiology (EBSC) Coordination Task Force on Sub-specialty Accreditation. This task force was created in 2004, and is chaired by Jose Lopez-Sendon and Peter Mills, the EAPCI is represented by Carlo Di Mario. The EBSC itself was created in 1992 by the Union Européenne des Médecins Spécialistes – Cardiology Section (UEMS - CS), in cooperation with the European Society of Cardiology (ESC) in order to set the “standards of care” for European cardiology. Its role is to make recommendations for setting and maintaining the standards of training in terms of quality, content, institutions and the trainers themselves. It evaluates member states and works towards the harmonisation of EC standards in cardiology. The EBSC created the current task force in order to, “define and promote sub-specialty accreditation standards, requirements and procedures… and contribute to the overall coherence of accreditation within the specialty of Cardiology”. This task force acts in several ways: as a coordinating body for training accreditation support within associations and Working Groups in the ESC; in implementing accreditation; and working with national societies to anticipate and influence regulation. The task force becomes a point-of-reference for the varied subspecialties as they work towards devising a common curricular template, developing common assessment methods and increasing awareness of European subspecialty accreditation development.
As you are perhaps aware, in Europe today the majority of countries offer apprenticeship, but no real certification subspecialty accreditation, and very few have any formal accredited training and recognised certification programmes. Peter Mills (see figure 1) speaking at the last EuroPCR, explained that the principles of accreditation must be readily acceptable throughout the community as well as being fully integrated, with a growing need to “complement the ESC core curriculum”.
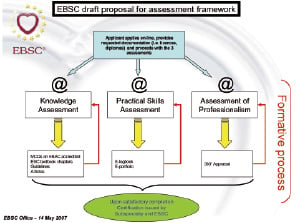
Figure 1. EBSC proposed outline for assessment framework.
A curriculum is now emerging through the experience of EAPCI members which aims to do this, assessing knowledge, skills and professionalism. Assessment methods are being debated, including the use of a European portfolio – or “e-logbook” – used to analyse the case mix that an aspiring interventionalist performs. Ideally a system will be put in place that assesses in a clear, comparable and repeatable fashion “intellectual development” with “direct observation of practical skills” that would demonstrate competence for the physician in such areas as patient selection, alternative clinical options or pre- and post- procedural care, etc.
The standardisation of accreditation in interventional medicine cannot simply apply to the curriculum itself, but touches on the role of the exam or knowledge assessment. There is a continuing discussion over “summative or formative” knowledge, taking into account that “learning should be part of assessment” and that the “most serious deficiencies in practice are not due to lack of knowledge”.
An effective training programme, training centre and trainer need to be defined. The emerging potential for simulators and virtual reality as training and assessment tools also needs to be quantified and qualified; their legitimacy depends on the development of a separate and recognised standard. To this end, an ongoing dialogue with industry has been developed, an essential cooperation allowing for “liaising with industry based programmes” and special industry sessions, requiring a neutral and accepted evaluation method to insure the independence of each programme. Four companies have already agreed to work together toward helping define these standards.
Much has been accomplished, but much more needs to be put into place before a complete European system of subspecialty accreditation exists. CME credits, professional certification with European-wide and international recognition, harmonisation of standards and quality-of-care are the ongoing goals, and the EAPCI will take the lead in this process as the details and necessary components make themselves known.
As Peter Mills concluded in his remarks, there is a “strength” in “sound educational principles” and cardiology “must play a leadership role” in a Europe that “represents authority and quality, arising from expert consensus across countries and subspecialties, e.g., ESC guidelines”. And as you all can well understand from the above, there is much more to come from your Association about this programme in the near future as it continues to evolve and take shape.

