This issue of EuroIntervention precedes the Congress of the European Society of Cardiology (ESC) by a few days. As you know, EuroIntervention is one of the official journals of the Society. Specifically, after the publication of the new impact factors, EuroIntervention has reached the sixth position among the 17 journals of the ESC family, a milestone that legitimately makes us proud.
The ESC Congress is a pivotal moment for enthusiasts of scientific literature, as it provides an opportunity for the presentation of new trials that are typically published simultaneously in top-tier journals. This year, the ESC Congress has attracted the submission of several studies revolving around interventional cardiology. Three studies (ILUMIEN IV, of which we published the trial design in 2021, OCTOBER and OCTIVUS) will further contribute to defining the role of optical coherence tomography as a guide for percutaneous coronary intervention (PCI). Other studies (e.g., OPT-BIRISK, STOPDAPT-3) will continue to explore the role of monotherapy with P2Y12 platelet receptor inhibitors. Furthermore, additional studies will help us better understand – or perhaps further confuse us – regarding the longstanding question of complete revascularisation in patients with acute myocardial infarction (e.g., MULTISTARS, FIRE). Specifically, two still-open questions pertain to the timing of complete revascularisation and the optimal method for identifying non-culprit lesions.
Naturally, the ESC Congress offers much more, but in general, what I want to emphasise here is that the effects of the COVID-19 pandemic on trials and their execution seem to have finally dissipated. For several years, cardiovascular research has suffered from an objectively complex situation that hindered the execution of numerous studies. The quality of submissions and trials presented at this year's Congress speaks of a significant recovery, which we hope will yield informative and impactful results for daily clinical practice.
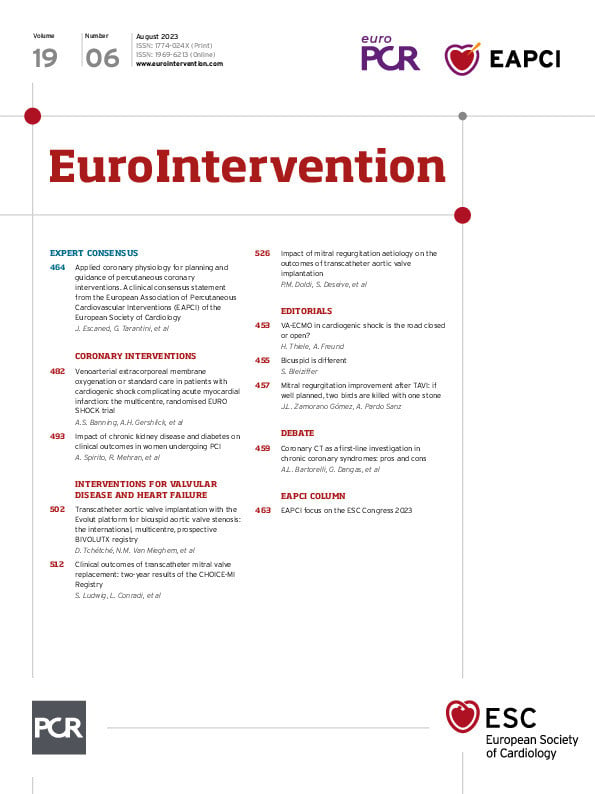
At EuroIntervention, we also strive to contribute to informing your decisions as interventional cardiologists. This issue, like others, presents a collection of articles that promises to be highly interesting.
Firstly, we offer you an interesting debate in which the invited authors tackle the question of the most effective first-line diagnostic tool for patients presenting with chronic coronary syndrome: functional testing or coronary computed tomography angiography (CCTA). Antonio L. Bartorelli and Daniele Andreini elaborate on the known advantages of CCTA, including its ability to rule out obstructive coronary artery disease (CAD) and to gauge the atherosclerosis burden. George Dangas and Gennaro Giustino concur that while CCTA is valuable in patients at low risk for CAD, given its known limitations – limited clinical evidence, lower sensitivity in detecting ischaemia, the inability to pair it with dynamic exercise testing – it should be seen as a complementary approach in patients at higher risk of CAD.
In coronary interventions, Javier Escaned, Giuseppe Tarantini and colleagues bring us a clinical consensus statement from the European Association of Percutaneous Cardiovascular Interventions on the use of applied coronary physiology for the planning and guidance of PCI. This expert consensus reviews the available physiology tools, including intracoronary pressure guidewires and functional coronary angiography tools, and their use in planning effective PCI strategies from preprocedural applications, through post-PCI optimisation.
Next, Amerjeet S. Banning, the late Anthony H. Gershlick and colleagues present the results of the EURO SHOCK trial, which aimed to determine if early use of venoarterial extracorporeal membrane oxygenation could improve outcomes in patients with persistent cardiogenic shock following PCI. Faced with limited recruitment during the pandemic, the trial was halted prematurely. In an accompanying editorial, Holger Thiele and Anne Freund call for a critical discussion on the challenges found in shock-related studies. By the way, Holger Thiele himself will present at ESC 2023 the results of another highly anticipated trial of venoarterial extracorporeal membrane oxygenation (ECLS-SHOCK).
How does the combined presence of chronic kidney disease and diabetes impact women who have received drug-eluting stents? In a pooled analysis of patient-level data of over 4,000 women receiving drug-eluting stents, Alessandro Spirito, Roxana Mehran and colleagues find that the combination of diabetes and chronic kidney disease was associated with a higher risk of all-cause death, cardiac death, myocardial infarction, stent thrombosis and target lesion revascularisation. While diabetes or chronic kidney disease alone were not predictors of myocardial infarction or stent thrombosis, their individual presence alone provides valuable information on the risk of adverse events.
Moving to interventions for valvular disease and heart failure, Didier Tchétché, Nicolas M. Van Mieghem and colleagues evaluate the clinical impact and valve performance of the Evolut PRO and R self-expanding prostheses in bicuspid aortic valve patients and explore the impact of different computed tomography sizing algorithms in the BIVOLUTX registry. With a device success rate over 90% and good clinical outcomes, the authors conclude that the Evolut bioprostheses can be used to treat selected bicuspid aortic valve patients, but that further research is needed into reducing the significant rate of conduction disorders and neurological events found in the study. This article is accompanied by an editorial by Sabine Bleiziffer.
Transcatheter mitral valve replacement (TMVR) has become an alternative therapy for selected patients at high surgical risk with mitral regurgitation (MR). Sebastian Ludwig, Lenard Conradi and colleagues share the two-year outcomes of the CHOICE-MI Registry, which assessed patients receiving TMVR with 11 different devices. Treatment with TMVR, including both transfemoral and transapical access, was associated with a durable resolution of MR, and a functional improvement at follow-up. Access site management and patient selection were the key determinants of mortality.
We conclude this issue with an analysis from Philipp M. Doldi, Simon Deseive and colleagues on the outcomes and changes in MR severity in patients with atrial functional MR (aFMR), ventricular functional MR (vMFR) and primary MR following transcatheter aortic valve implantation (TAVI). They demonstrate that aFMR patients show similar procedural and long-term outcomes compared to vFMR patients and that the presence of aFMR is associated with a lower risk of MR persistence after TAVI. In an accompanying editorial, José Luis Zamorano Gómez and Ana Pardo Sanz underline the importance of taking into account the aetiology of the mitral regurgitation as well as the valves and the patient themselves.