Abstract
Aims: Acute aortic syndromes (AAS) still represent life-threatening conditions. The aim of this study was to describe our experience in the management of patients (pts) with AAS and to evaluate the safety and feasibility of endovascular treatment (EVT) in high surgical risk patients.
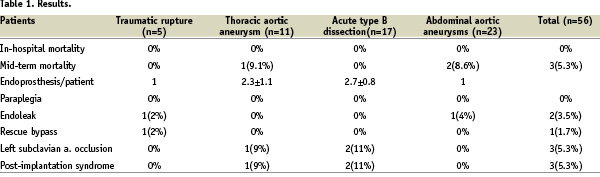
Methods and results: One hundred and four patients underwent EVT. We selected 56 pts with AAS: 17 complicated type B aortic dissections, five traumatic aortic ruptures at the isthmus, 11 thoracic aneurysms and 23 pts with large AAA with impending rupture. All these pts were at high surgical risk because of their comorbidities and/or their emergency situation. They were clinically followed during hospitalisation and they underwent a 2 mm-interval CT-scan two weeks, six and 12 months after discharge and every year after.
Death, paraplegia, open surgical conversion did not occur. Two pts underwent a successful secondary EVT for type I endoleak. One patient with thoracic aortic aneurysm died of septic shock from pneumonia 78 days after discharge and two pts with AAA suffering from a severe three-vessel coronary disease experienced sudden death at one year follow-up.
Conclusions: EVT seems to be a safe and effective therapeutic option with good short- and midterm results in patients with AAS at high surgical risk. Thus, it can be considered as a less-invasive alternative in patients considered otherwise unsuitable for conventional surgery, even though a careful, continued follow-up is still necessary to confirm the long-term safety and effectiveness of EVT in AAS.
Introduction
Acute aortic syndromes – such as large thoracic and abdominal aortic aneurysms with impending rupture, complicated acute type B dissections, traumatic rupture of thoracic aorta – still represent life-threatening conditions.
Today different therapies are available, however which one is best as well as what is the exact timing for optimal management of these pathologies remains controversial. Surgical therapy is contraindicated in several cases, because of the patient’s elderly age and the presence of serious comorbidities such as: pulmonary diseases, renal dysfunction, cerebrovascular diseases, coronary artery disease, congestive heart failure.1
Endovascular treatment (EVT) for aortic pathologies offers several advantages compared to conventional open surgery: less invasiveness, lower morbidity, less haemodynamic and metabolic stress due to aortic clamping and de-clamping, shorter hospitalisation stay.2-4 There has been great progress in endovascular treatment since its introduction. The early endografts have been modified, and new endografts have been introduced with technology designed to correct previous problems. Adjunctive devices, such as extenders and rescue techniques have been developed and device profiles have been decreased. We describe our experience in the management of pts with acute aortic syndromes and to evaluate the safety and feasibility of EVT in patients at high surgical risk.
Methods and population
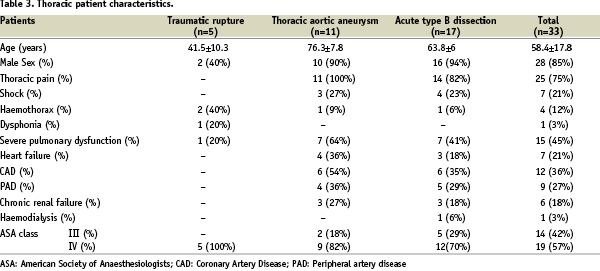
From March 2002 to December 2004, 104 patients with aortic diseases were admitted to our department. One hundred-one patients underwent EVT: 33 patients with thoracic aortic diseases, 68 patients with AAA. Three patients with AAA were not considered fit for EVT because they did not show the required anatomic criteria.5,6 Among our population treated by EVT, we selected 56 patients with acute aortic syndromes: 33 patients with thoracic aortic diseases (59%), 23 patients (41%) with large abdominal aortic aneurysms (mean maximum diameter: 76.8±11.9 mm).
We defined acute aortic syndromes as those aortic pathologies requiring an emergency or urgent treatment, such as: thoracic and abdominal aortic aneurysms with impending rupture, traumatic ruptures of thoracic aorta, acute type B dissections complicated by increasing false lumen, malperfusion and persistent pain despite an optimal medical treatment.
All patients with thoracic disease were in an emergency situation due to contained or free rupture of the thoracic aorta complicating blunt chest trauma or aneurysm, lack of response to medical treatment, pain, or increasing false lumen of acute type B dissection. They underwent endovascular treatment between six to eight hours from hospital admission.
Thoracic diseases included: 17 complicated, type B aortic dissections, five traumatic aortic ruptures at the isthmus, 11 thoracic aneurysms.
The abdominal group consisted of 23 patients with large AAA with impending rupture (mean maximum diameter: 76.8±11.9 mm; range: 65-110 mm). Three of the four patients presenting with abdominal pain at admission suffered from a para-anastomotic AAA after previous open aortic prosthetic reconstruction. In these patients the pain began between six and 12 hours before hospital admission. All patients with AAA underwent EVT within 24 hours from hospital admission.
Patients of both the thoracic and abdominal groups were considered at high surgical risk if they were in an emergency situation and/or they had one or more of the following criteria: age 80 years or more, serum creatinine level 2.5 mg/dl or more, severe pulmonary dysfunction (defined as the requirement of home oxygen, forced expiratory volume in 1 second > 20% predicted, or forced expiratory flow at 25% to 75% of vital capacity > 20% predicted); cardiac dysfunction (defined as a left ventricular ejection fraction < 30%); recurrent symptomatic congestive failure as documented by an attending cardiologist; severe coronary artery disease unsuitable for either percutaneous or surgical revascularisation; intermittent symptomatic ventricular ectopy poorly controlled with medication; or hepatic failure. These patients were classified as category III-IV by the American Society of Anaesthesiologists (ASA).
A spiral computed tomographic scan and digital subtraction angiography of the thoracic and abdominal aorta were performed for measuring and localising purposes. CT-scan was performed for the whole aorta with sagittal and coronal reconstructions and volume-rendering. Conventional angiography and/or DSA was done at time of endovascular intervention in order to evaluate aneurysmal angulation and the iliac-femoral axes to judge the anatomical suitability of the vascular access for device implantation.
The stent graft placement was performed in a dedicated catheterisation laboratory with high performance X-ray equipment, thus allowing an optimal angiographic visualisation and making easier all manoeuvres that depended on high definition fluoroscopy such as the device deployment. The dedicated cath lab is able to become a surgical theatre in case of conversion to conventional surgery. The procedures were usually performed by an experienced interventional cardiologist with the support of a cardiovascular surgeon and two dedicated nurses. Patients received general anaesthesia and mechanical ventilation during thoracic endovascular procedures and epidural anaesthesia during abdominal endovascular procedures. All procedures were performed under controlled hypotension induced by sodium nitroprusside (mean arterial pressure approximately 60 mmHg) just before the placement of the endograft. The endovascular approach was commonly transfemoral, and the implantation of the endoprosthesis was achieved through a surgical exposition and arteriotomy of common femoral arteries.
Both thoracic and abdominal endovascular procedures began by introducing a 6Fr pigtail catheter through the radial artery in order to obtain intraprocedural aortographies, direct monitoring of invasive arterial pressure and a precise localisation of the subclavian artery in the case of thoracic aortic diseases. The “telescope technique” was used to cover the descending thoracic aorta with multiple stent grafts of increasing diameters, from the proximal to the distal aorta. (Table 1).
In all cases but one (GORE Excluder) we used TALENT endoprostheses of 10 cm in length. (Figure 1 a-b).

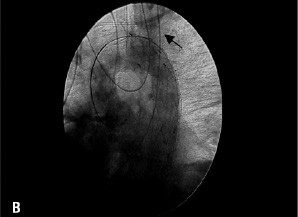
Figure 1a: Angiography showing a type B dissection of patient treated several hours after hospital admission (the arrow indicates the thoracic intimal tear). Figure 1b: Angiography showing the complete exclusion of the false lumen after deployment of three stents with the telescope technique (the arrow shows the patent left subclavian artery which has been over-stented with a free-flow proximal part of Talent endoprosthesis).
For abdominal endovascular procedures, we used a bifurcated modular endoprosthesis in 20 patients (17 TALENT, three GORE) and in three patients we implanted an aorto-uniliac endoprosthesis (TALENT) with a femoro-femoral bypass. In five out of our 23 patients with AAA we needed extensions to cover the iliac bifurcation. Proximal neck was < 1.5 cm in 18 patients. Patients with calcifications > 30% were excluded.
The endovascular criteria for a successful procedure were as follows: 1) absence of death or surgical conversion, 2) exclusion of aneurysm or false lumen, 3) occlusion of all thoracic tears in type B dissection. In type B dissections, the persistence of a double lumen in the abdominal aorta was not considered as an indication of failure if the thoracic intimal tear was covered and there was no blood in the thoracic false lumen. The time frame we considered for the assessment of absence of death or surgical conversion was 30 days.
Postoperative surveillance included basic laboratory testing, physical examination, and spiral computed tomography scans before discharge, at three, 12 months and yearly thereafter, in order to evaluate the occurrence of endoleaks in accordance to the White classification.7
Results
In hospital results
THORACIC GROUP
The mean age of patients was 58.7±17.1 (range 19-81 years).
In the group with traumatic rupture, two patients showed haemothorax and one had an increasing pseudoaneurysm with dysphonia caused by compression of the laryngeal nerve.
In the group with thoracic aortic aneurysm, three patients suffered from shock and one of them had a massive left haemothorax. The mean thoracic aneurysmal diameter was 79.8±13.3 mm. The mean procedural time for the thoracic group was 45±10 minutes.
Laceration of the right iliac artery occurred during the endovascular procedure performed on a 19-year-old woman with traumatic rupture of the aorta and multitrauma (head injury and leg fractures) requiring an emergency rescue iliac-femoral artery bypass.
Open surgical conversion was not required in any case. Two patients with traumatic ruptures required a blood transfusion.
The left subclavian artery was intentionally occluded in three patients, two with acute type B dissection, and one with thoracic aortic aneurysm, without steal phenomena. One patient with thoracic aortic aneurysm and obstruction of the aortic bifurcation required an associated aorto-bifemoral bypass to use as main vascular access.
There were no perioperative deaths and no paraplegia, despite extensive repair of the entire descending thoracic aorta in 15 patients.
Post-implantation syndrome8 (haematuria and fever without leukocytosis, refractory to antipyretics drugs) occurred in one patient with thoracic aortic aneurysm and three patients with type B aortic dissection, but they were quickly responsive to steroid therapy.
The intraoperative angiography and computed tomographic scan on discharge showed no significant endoleaks in any patient. The mean length of ICU stay and total hospitalisation was 1.3±0.5 and 7.7±5.5 days, respectively.
ABDOMINAL GROUP
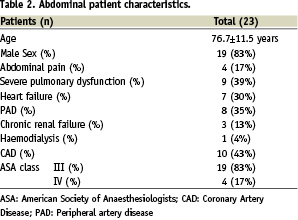
Patients with AAA were older (mean age: 76.7±11.5 years) than those in the thoracic group and showed more comorbidities (Table 2 and 3).
In two patients, we observed a distal type I endoleak at the intraoperative angiography soon after the endoprosthesis placement and an iliac extension was needed to cover it. The mean procedural time for the abdominal group was 45±10 minutes.
There were no perioperative deaths, no paraplegia and no open surgical conversion.
The intraoperative angiography and computed tomographic scan on discharge showed no significant endoleaks in any patient (Figure 2a-b).


Figure 2a: Pre-operative CT-scan showing a large para-anastomotic abdominal aortic aneurysm (maximum diameter: 110 mm) with intraluminal thrombus (arrow). Figure 2b: CT-scan of abdominal aorta after the implantation of a bifurcated endoprosthesis.
The average length of intensive care unit and hospital stay was 1.6±0.6 and 5.4±2.2 days, respectively.
Mid-term results
THORACIC GROUP
The follow-up averaged 21.6±5.7 months ranging from nine to 32 months. All patients were alive at the time of follow-up. Two patients with traumatic rupture of the aorta required orthopaedic surgery (leg and arm fractures), performed in a trauma centre five and seven days after endovascular treatment. Both patients were discharged home two weeks after the complex multi-trauma. Four older patients, who had a major comorbidity, were transferred to a rehabilitation centre 7.1±4.7 days after treatment. One of these, an 84 year-old patient with thoracic aneurysm, died of septic shock from pneumonia 78 days after endovascular surgery.
Only one type I endoleak was noted three months after the endovascular procedure in the first patient treated for traumatic rupture by implantation of a Gore-Excluder. The patient refused immediate treatment, but a CT-scan performed at 30 month follow-up there was evidence of increasing endoleak and a 2 mm migration of the endoprosthesis. Thus, he underwent a successful endovascular implantation of a further Gore endoprosthesis proximally to the previous one. (Figure 1a,2b)
ABDOMINAL GROUP
The follow-up ranged between eight and 31 months (average 20.7±6.8 months).
At one year follow-up two patients, suffering from severe three-vessel CAD, that had been judged unsuitable for either PCI or surgical revascularisation, died of myocardial infarction after admission to another hospital centre. A 67 year-old woman with AAA treated by a modular bifurcated endoprosthesis implantation showed a type I distal endoleak at the three month CT-scan. She then successfully underwent implantation of an iliac extension.
Discussion
Our data show that EVT in high surgical risk patients with acute aortic syndromes is an effective and low-risk treatment strategy.
Patients with aortic diseases are often elderly and have severe comorbidities, making them poor surgical candidates. Although long-term data are not yet available, EVT represents a more simplified approach associated with a shorter operating time, less blood loss and a shorter hospitalisation9,10, with increased quality-of-life in the perioperative period and a more rapid recovery time.11
Moreover, EVT allows a prompt treatment of associated lesions in complex multi-trauma patients in which heparinisation and extracorporeal support are not indicated and delayed treatment may be life-threatening.
Thoracic aortic endovascular treatment
Since the Stanford group reported the first large series of endovascular stent-graft of the thoracic aorta in 199412, many centres have turned their attention to the treatment of thoracic aorta diseases.13-17
The main concern in type B dissections is the determination of true and false lumen and their relationship with vital vascular branches (celiac axis, renal arteries). In our series, all vital branches were perfused by the true lumen, the graft was then placed within the true lumen at the site of the intimal tear, excluding false lumen flow.
In 15 patients (45%) of our thoracic group, we stented large portions of the descending thoracic aorta covering several intercostal arteries without having any instances of paraplegia.
In the study by Dake and al18 multiple stents were used in 33% of the patients, but this frequency may be as high as 70%.19 The sequential placement of endoprosthesis elevates both the immediate- and long-term risk because of the potential for leakage in the junctions between segments.20 The treatment of lengthy aortic segments in the region between T9-T12, during endovascular procedures, has been encouraging since the development of paraplegia seems to be less frequent than historically reported in surgical studies.4 In particular, it seems that simultaneous open abdominal and endovascular thoracic repair carries an increasing risk of paraplegia caused by insufficient collateral circulation due to the loss of lumbar and thoracic intercostal arteries21. In our series, the only patient treated by simultaneous open abdominal and endovascular thoracic repair did not show any paraplegia or paraparesis. Our results are consistent with recent studies22 that demonstrated in human cadavers an anatomic continuity among the vertebral arteries, anterior spinal artery and radicularis magna arteries. On the basis of that finding, the sacrifice of the segmental arteries emerging from the diseased aorta can be justified.23
Three patients required exclusion of the left subclavian artery to obtain adequate proximal neck length. We did not perform prophylactic left subclavian bypass in these patients. Our experience and that of others suggests that prophylactic left subclavian bypass is not routinely necessary to prevent complications related to exclusion of the left subclavian artery.24,25
Although direct comparison may not be justified because of differences in patient selection and the small number of series, our in-hospital and midterm results seem to be very encouraging. In the combined experience from EUROSTAR and UK THORACIC ENDOGRAFT registries4 the reported in-hospital mortality in emergency repair was 29% in aortic thoracic aneurysms, 12% in acute type B dissections, 6% in traumatic ruptures. In our experience, we treated high-risk patients in emergency conditions without in-hospital mortality and with only one late death in an elderly patient in whom the surgical risk was considered prohibitive.
Abdominal aortic endovascular treatment
In our abdominal series 40% of patients were older than 75 years and younger patients had almost two concomitant diseases. All patients with AAA who underwent endovascular treatment in our study were at high risk for conventional open surgical repair on the basis of number and nature of their comorbid medical conditions. Our findings showed no perioperative mortality and morbidity. However, midterm outcome was affected by previous concomitant diseases of the population.
Two open registries have been proved successful at monitoring the progress and development of endovascular treatment of AAA over the past 8 years.26,27 These registries have indicated that the 30-day mortality after endovascular treatment (EVT) could be as high as 2.9% and 3.1%28,29, but findings of other studies have estimated lower mortalities.30
Open surgical repair of abdominal aortic aneurysms (AAA) carries a 30-day mortality of 4 -12%31. Other studies have also shown that operative mortality rates after surgery increased with the age of the patient (4.6%, 5.4%, and 12% in patients aged 60-69 years, 70-79 years, and > 80 years, respectively).32
Coronary artery disease is responsible for up to 60% of perioperative deaths after open AAA surgical repair.33-35 Adverse cardiac events have been attributed to excessive stress on the myocardium caused by the combined effect of anaesthetic induction, aortic clamping and declamping, operative blood loss and associated haemodynamic and metabolic changes. It is likely that haemodynamic alterations associated with EVT are less severe. However, late outcome in high surgical risk patients will remain dominated by individual comorbid condition, even though endovascular treatment eliminates the immediate surgical risk. Reports from EVAR-2 trial showed no survival benefit for EVT in patients unfit for open repair.36 However, in our patients with large AAA (mean maximum diameter: 76.8±11.9 mm), EVT resulted in saving lives since their impending aneurysm rupture – without chance of surgical treatment – would have led to rupture and death.
Recent reports from the EUROSTAR registry37 and the Cleveland Clinic38 raised another concern: long-term results after endovascular repair appear to be worse for larger aneurysms (> 65 mm), the ones that are most in need of repair. The higher mortality rates in AAA > 65 mm has been related to several factors such as: more severe atherosclerosis and comorbidities and less favourable anatomic parameters (proximal aortic neck length, diameter and angulation) associated with larger AAA.
Our patients, all at high surgical risk with AAA > 65 mm, were able to undergo endovascular AAA repair with good EVT related morbidity and mortality rates. This was probably due to the careful evaluation before the treatment in order to establish if these patients showed the required anatomic criteria for EVT.
In our population, three patients were not anatomically suitable for EVT. Difficulties with vascular access and attachment site were predominant reasons for exclusion (two patients with conic proximal neck with a diameter > 30 mm, one patient with a proximal neck angulation > 60° and tortuous and calcified iliac arteries).
Secondary interventions after EVT of AAA is a relatively frequent event. In EUROSTAR they have been seen to be required at an approximate rate of 10% per year throughout the intermediate and late follow-up periods. Transfemoral procedures are the most frequent category of secondary interventions. In most cases these procedures consisted of aortic or iliac extension for endoleak associated with low morbidity and mortality rates.39 In our series only one type I endoleak was detected at 3-month CT-scan in a 67-year old woman, and it was treated by an iliac extension without any further complication. The time- dependent endoleak may be related to thrombus infiltration and the subsequent re-absorption as wall as to the progressive nature of atherosclerotic disease.
Our midterm follow-up was uneventful, even in those three patients suffering from a para-anastomotic AAA after previous surgical prosthetic repair. The natural history of para-anastomotic aneurysms can be complicated by rupture, thrombosis, embolism, and pressure on – or erosion into – adjacent structures. Endovascular treatment of these lesions could provide an extra advantage, since open surgical repair is associated with increased morbidity and mortality (24-70% in ruptured para-anastomotic AAA, 3-17% in elective open repair) rates.40 The increase in morbidity and mortality is thought to result from the difficulties inherent to re-operative surgery, as well as to the relative increased age of patients presenting with this condition.41 Our three patients were > 75 years old, with comorbid medical conditions, and they were successfully treated by implantation of a bifurcated endoprosthesis that was anchored proximally and distally in the native aorta.
Limitations of the study
This is a single centre and retrospective study of a selected group of high-risk patients with AAS. Our study is limited by the relatively small number of patients, even though the complexity of the patients and of their diseases support the effectiveness of a less invasive procedure such as EVT. In the present study we reported on our mid-term results with a follow-up ranging from eight to 32 months. A long-term follow-up is necessary to assess the durability and long-term effectiveness of EVT.
Conclusions
EVT seems to be a safe and effective therapeutic option with good short- and mid- term results in patients with AAS at high surgical risk. Thus, it can be considered as a less-invasive alternative in patients considered otherwise unsuitable for conventional surgery even though a careful, continued follow-up is still necessary to confirm the long-term safety and effectiveness of EVT in AAS.
Supplementary data
To read the full content of this article, please download the PDF.
Vidéo 1
Vidéo 2
Vidéo 3
Vidéo 4
Vidéo 5

