When we thought of these introductory pages two years ago, with the intention of briefly introducing the contents of EuroIntervention before diving into the more in-depth reading of the individual articles, we also thought of starting with a short Editor’s note commenting on the salient facts of the month in interventional cardiology. If I look back, I have to admit that I probably found myself talking more about the effects of the pandemic on our work than about the topics that I would have imagined at the beginning of 2020.
A few months ago, for example, I commented with some relief on the effects of mass vaccination on the resumption of normal conference activities with physical participation. Today, again, I am writing during a steep and ascending phase of the contagion curve, with a much more transmissible variant around. During the first wave, at least in my country, I remember that much of the media aimed at raising people’s awareness by explaining the meaning of logarithmic growth. Many gave the example of grains of rice that double in the squares of a chessboard: one in the first square, two in the second, four in the third, eight in the fourth, etc. At the time, this example seemed to many an interesting but abstract mathematical concept. With the omicron variant raging all over the world, the meaning of that concept is, if possible, even more evident today.
And while the virus spreads, thankfully contained by available vaccines, our knowledge must be just as quick to adapt to the mutations of the pandemic. If I reread many of the articles that the field of cardiology has produced in the course of the first waves of this virus, I also feel that they should be frequently updated in light of the changed circumstances. For example, we initially hospitalised many patients with COVID-19 complicated by acute coronary syndrome, now we also hospitalise many patients with acute coronary syndromes and, incidentally, a positive swab: but are they the same? Is the current literature on COVID-19 up-to-date, or struggling to keep up with the pace of such a changing virus?
To put it mildly, we live in interesting times, but we must not lose the drive to do what we have always done in treating our patients: update our knowledge to always serve them best. Many authors contribute to this educational aim and their work can be found, as always, in the following pages.
Let’s now see what we have in store for you in this issue.
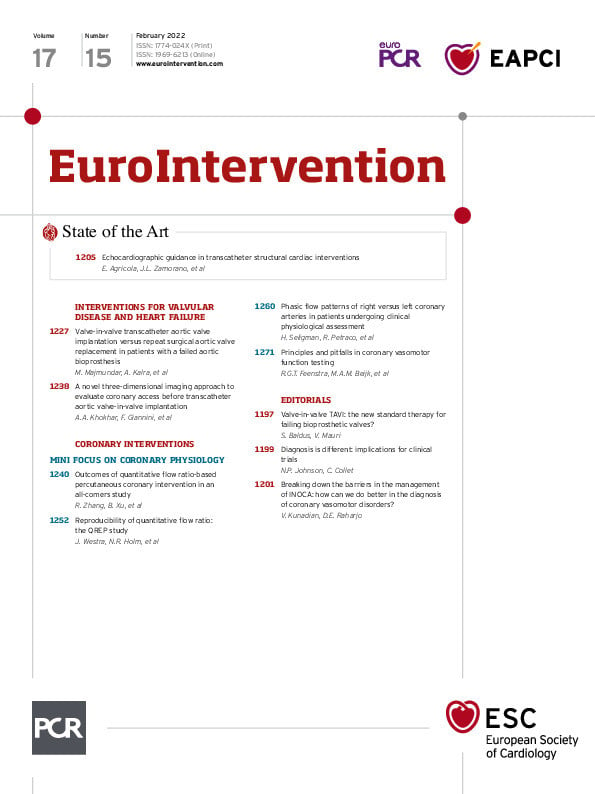
The evolution in imaging has been one of the critical elements in advancing catheter-based treatments of structural heart diseases. In this issue of EuroIntervention, Eustachio Agricola, José Luis Zamorano and colleagues present a State of the Art on echocardiography techniques in use today. The authors provide tips and tricks for a wide range of catheter-based interventions, from guiding transseptal crossing, to left atrial appendage closure, transcatheter mitral or tricuspid valve repair or replacement, percutaneous closure of patent foramen ovale and atrial defects, percutaneous closure of paravalvular leaks, and more. They consider current challenges as well: radiation exposure; optimisation of intraprocedural and post-procedural evaluation; and the necessary training in these essential techniques which are in constant evolution.
Could transcatheter aortic valve implantation (TAVI) be a feasible option for treating bicuspid aortic valve stenosis? What conditions would be optimal for choosing TAVI over surgical aortic valve replacement (SAVR) in treating this condition? These are the questions posed by Monil Majmundar, Ankur Kalra and colleagues as they evaluate the available clinical data exploring the complexities of bicuspid aortic valve stenosis and these two procedures. They conclude that under certain clinical and anatomical circumstances –in patients who do not require concurrent aortic root repair– TAVI could be a feasible choice, though more studies are needed. This article is accompanied by an editorial by Stephan Baldus and Victor Mauri.
This issue’s mini focus is on coronary physiology. Authors Rui Zhang, Bo Xu and colleagues use angiographic data from the PANDA III trial in a retrospective analysis to see whether angiography-based quantitative flow ratio (QFR)-consistent treatment is associated with prognosis in patients undergoing percutaneous coronary intervention (PCI). They conclude that QFR-consistent treatment had a lower risk of two-year major adverse cardiac events supporting the use of physiology-guided decisions in the cath lab. This article is accompanied by an editorial by Nils P. Johnson and Carlos Collet.
Continuing with our mini focus, Jelmer Westra, Niels Ramsing Holm and colleagues assessed the reproducibility of QFR measurements from different international centres. The reproducibility of QFR was seen to be dependent on the observer, angiographic quality, and the coronary artery stenosis severity as assessed with fractional flow reserve, underlining for the authors the importance of strict adherence to standard operating procedures for QFR analysis.
Does clinical interpretation of coronary physiological data differ between the left and the right coronary systems? The next article in our mini focus answers this question by studying the phasic patterns of coronary flow in the left versus right coronary arteries of patients undergoing invasive physiological assessment. Authors Henry Seligman, Ricardo Petraco and colleagues conclude that diastolic flow predominance is seen in both the left and right coronary arteries and thus the clinical interpretation of coronary physiological data should therefore not differ between the two systems and was not affected by the underlying degree of stenosis or microvascular disease severity.
Our mini focus concludes with an article by Rutger Feenstra, Marcel A. Beijk and colleagues on the “unmet need” that prevents the widespread use of coronary vasomotor function testing for diagnosing coronary vasomotor dysfunction. While coronary vasomotor function testing can be used to diagnose patients with angina in the presence of non-obstructive coronary artery disease, no consensus exists on a standardised study testing protocol. This is seen to have an impact on clinical acceptance of the concepts of coronary vasomotor dysfunction and the widespread adoption of such testing protocols in current clinical practice. This article is accompanied by an editorial by Vijay Kunadian and Daniell Edward Raharjo.
Ready? So, let’s begin.
Supplementary data
To read the full content of this article, please download the PDF.