The pandemic has brought about a significant shift in our approach to international travel, particularly for conferences and meetings for work. The widespread adoption of virtual meetings through dedicated platforms has opened our eyes to the inefficiency of spending hours travelling to events that often last only a fraction of the time it takes to reach them. While we have discussed the superiority of in-person meetings over online ones, I would like to avoid the cliché of celebrating them. Instead, I propose a reasonable compromise: to go where I enjoy going and find alternative solutions when a virtual meeting can reasonably replace a physical one.
It was the nostalgia for the days before the pandemic that prompted me to accept an invitation from the Japanese Association of Cardiovascular Intervention and Therapeutics to attend their congress, which is increasingly known for its international flavour. Before this congress, I made a trip to Thailand for some lectures in a country I had never visited before. I mention this not to emphasise the attractive and perhaps touristic aspect (clear to anyone who has visited these beautiful and fascinating places) but to highlight the newfound awareness that such exchanges are invaluable when it comes to acquiring information that is hard to find in scientific articles. These exchanges shed light on the profound differences in problems and solutions within the field of interventional cardiology. For example, during my time in Thailand, I learned about the varying thrombotic and haemorrhagic risks associated with antithrombotic therapy in Southeast Asia compared to Europe, and even compared to different regions of East Asia. In Japan, I discovered the extensive use of several cutting-edge interventional techniques that are rarely seen in Europe, and I learned that – surprisingly – the transcatheter closure approach for patent foramen ovale was only initiated a few years ago.
The differences and nuances in local practices are so vast that relying solely on general scientific literature can be misleading. Certain trips will, therefore, always be irreplaceable to gain a deeper understanding of the topics within our discipline. Understanding these themes is a challenge, even for seasoned professionals. Understanding and rendering the complexity of these geographical nuances is also a challenge for EuroIntervention, and we probably should do more in that respect.
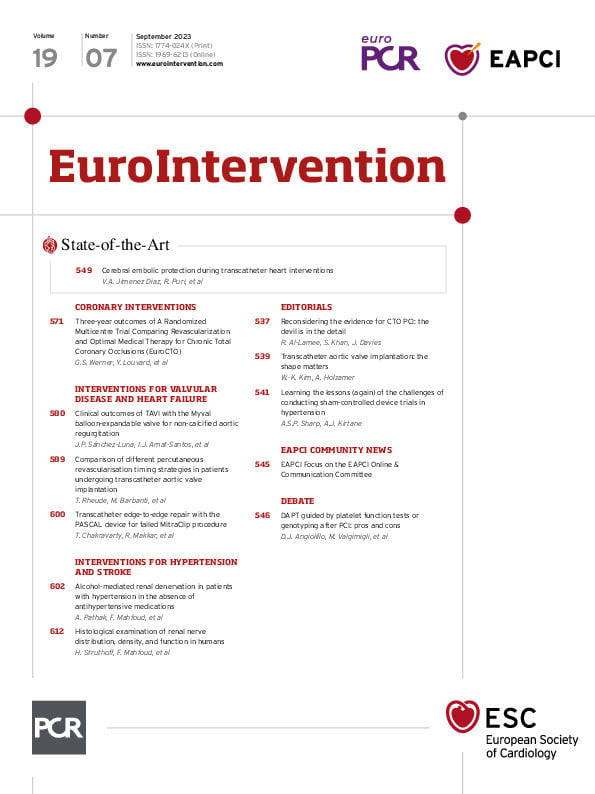
But, while we continue on this reflection, here is an introduction to the contents of this month’s edition.
We open with a debate examining the pros and cons concerning the use of tools for guiding dual antiplatelet therapy. Dominick J. Angiolillo and Mattia Galli argue that current evidence indicates platelet testing and genotyping are the best strategies for optimising the balance between safety and efficacy. While its use may be justified in the identification of clopidogrel non-responders, Marco Valgimigli and Antonio Landi see guided dual antiplatelet therapy as a costly, overly complex treatment that already belongs to the past.
Next, we bring you a State-of-the-Art on cerebral embolic protection during transcatheter heart interventions by Victor Alfonso Jimenez Diaz, Rishi Puri and colleagues. Periprocedural embolic showers of debris, ischaemic stroke and postprocedural cerebral lesions are among the obstacles that cerebral embolic protection devices can potentially mitigate in patients receiving transcatheter aortic valve implantations (TAVI). This review examines the clinical-pathological rationale for the development of the devices, the current evidence, and the expansion of their use into non-TAVI transcatheter procedures.
In coronary interventions, Gerald S. Werner, Yves Louvard and colleagues present the three-year outcomes of the EuroCTO trial comparing the long-term safety of percutaneous coronary intervention (PCI) for chronic total occlusions with optimal medical therapy (OMT). While the one-year results showed a benefit of PCI in clinical symptoms compared to OMT, the three-year follow-up demonstrated continued benefit in angina control and no increased rates of cardiovascular death or myocardial infarction, compared to OMT, provided the procedure was successful. Rasha Al-Lamee, Sarosh Khan and John Davies reflect on symptomatic assessment and indications for chronic total occlusion PCI in an accompanying editorial.
In interventions for valvular disease and heart failure, Juan Pablo Sánchez-Luna, Ignacio J. Amat-Santos and colleagues evaluate the feasibility and safety of the balloon-expandable Myval device in the treatment of non-calcified aortic regurgitation. This challenging patient subset often has large annuli, and the device offers extra-large sizes, in 30.5 mm and 32.0 mm. Procedural success was high and oversizing was demonstrated to be a valid strategy for device anchoring with no cases of annular rupture or aortic dissection. Survival at 1-year was adequate, with no cases of early prosthesis deterioration. In an accompanying editorial, Won-Keun Kim and Andreas Holzamer discuss the novel left ventricular outflow tract classification system proposed by the authors.
Does the timing of PCI influence outcomes? Tobias Rheude, Marco Barbanti and colleagues tackle this question in the REVASC-TAVI registry, a study of stable coronary artery disease patients with severe aortic stenosis who received PCI either before, after or concomitantly with TAVI. Performance of PCI after TAVI seemed to be associated with the best two-year clinical outcomes, whereas concomitant procedures had the highest mortality rates, and PCI before TAVI had the lowest rates of vascular complications and major bleeding. This registry opens the door for further trials using different transcatheter heart valve platforms.
We then move to interventions for hypertension and stroke with two articles on renal denervation (RDN). First, Atul Pathak, Felix Mahfoud and colleagues investigate the efficacy and safety of alcohol-mediated RDN in the absence of antihypertensive medication. Even though the results of this trial did not demonstrate a blood pressure difference between those randomised to the sham procedure or the alcohol-mediated RDN arm, the trial did confirm the safety of alcohol-mediated RDN and its ability to lower ambulatory and office BP in patients with severe uncontrolled hypertension. In an accompanying editorial, Andrew S.P. Sharp and Ajay J. Kirtane offer insights into the complexities of designing sham-controlled trials.
The next article reviews an effort to optimise the procedural performance of RDN with authors Helge Struthoff, Felix Mahfoud and colleagues providing us with a histological examination of the distribution of renal nerves, focusing on the post-bifurcation vessel segments. They demonstrate that the nerve density and the ratio of efferent and afferent nerves increase from proximal to distal and are numerically highest in the post-bifurcation segments. These findings can help to guide RDN, as they suggest that the number of potentially treatable nerves increases in the distal artery segments.
And now, we will turn to the articles themselves.
Editorial
DOI:
A State-of-the-Art on cerebral embolic protection during transcatheter heart interventions; a debate on guided DAPT; the 3-year outcomes of the EuroCTO trial; the Myval device in non-calcified aortic regurgitation; timing of PCI in TAVI; alcohol-mediated RDN; distribution of renal nerves; and more
You need to subscribe to download this file
×
If you are not yet a subscriber, please subscribe to download this file.
Download citations
×
Select a format