Abstract
Aims: The incidence of obesity is increasing continuously in industrial countries. Vascular complications after the transfemoral approach (TF) for either coronary angiography (CA) or angioplasty (PCI) are more frequent in this population. The transradial approach may decrease the risk of such complications.
Methods and results: We undertook a prospective, multicentre, European registry of overweight patients (BMI ≥35), undergoing CA and/or PCI in centres with broad experience in the transradial approach (TR). The vascular approach was left to the operator’s discretion. The primary end point was the occurrence of access related complications resulting in delayed hospital discharge 555 patients, (age 60.8±10.9 years; males 57.3%; BMI: 38.5±3.6 kg/m2) were included in the study. Of these, 157 underwent the transfemoral approach and 398 the transradial. Total procedure time was significantly shorter for the transradial approach in these morbidly obese patients (TR: 35.5±25.8 min versus TF: 52.4±25.2 min, p=0.0001), and hospital stay after CA or PCI was significantly shorter in the transradial group (TR: 1.8±2.3 days versus TF: 2.5±4.3 days, p=0.04). Vascular complications delaying hospital discharge occurred in 0.8% of TR patients vs 5.1% TF patients. p=0.0009).
Conclusions: The rate of vascular complications in overweight patients after CA or PCI can be significantly decreased by the use of the transradial approach in centres with a large experience.
Abbreviations list
MI = Myocardial Infarction
ACS = Acute Coronary Syndrome
PCI = Percutaneous Coronary Intervention
CA = Coronary Angiogram
CABG = Coronary Artery Bypass Graft surgery
CVA = CerebroVascular Accident
Introduction
Recent reports from the American National Centre for Health Statistics show that the numbers of overweight and obese people are extremely high in the United States, reaching epidemic proportions1. Other publications have also shown an increasing rate of obesity in the European population and in other countries throughout the world. It is estimated that there are up to 200 million obese citizens in the recently expanded European Union2.
In obese patients, difficulty gaining femoral arterial access and achieving post-procedural haemostasis leads to an increased risk for vascular complications. It has been reported that the risk of vascular complications for cardiac catheterisation is greater in obese patients3,4.
The purpose of this study is to determine whether the transradial (TR) approach for CA and/or PCI can be safely and easily used in very overweight patients (BMI ≥35) and to compare the TR, and transfemoral (TF) approaches in these patients for efficacy (including crossover, procedural success rate, duration, X-ray exposure, vascular complication and hospital stay).
Methods
In this prospective multicentre European registry (14 centres), we included all patients with a BMI ≥35 kg/m2 presenting for coronary angiography (CA) or percutaneous coronary intervention (PCI) (January 2004 to December 2005). All clinical presentations were permissible (including ST-elevation acute myocardial infarction). There were no exclusion criteria.
In each centre, there was at least one operator with a wide experience in the TR approach for CA and PCI with a rate of TR approach superior to 80% in daily practice and a learning curve of more than 1,200 TR procedures. The vascular approach was chosen by the operator.
Overweight and obesity criteria
According to baseline body-mass index (BMI), subjects are categorised into underweight (BMI < 18,5 kg/m2), normal (BMI 18,5-24,9 kg/m2), overweight (BMI 25,0-29,9 kg/m2), obese (BMI 30-34,9 kg/m2) and very obese (BMI > 35 kg/m2)2.
Endpoints
The primary endpoint was a composite vascular endpoint, comprising one or more of the following: vascular complications requiring surgical intervention; blood transfusion; reduction in haemoglobin by ≥3 g/dl or haematocrit by 10%; acute arm or leg ischaemia; forearm compartment syndrome; or other vascular complication resulting in delayed patient discharge from hospital (including false aneurysm and haematoma clinically assessed to be > 3 cm). Important haematoma was defined as resulting in delayed patient discharge from hospital.
Secondary endpoints were:
a) Vascular complications included in the combined endpoint, with clinical haematoma assessed to be > 3 cm, plus cholesterol embolisation, cerebrovascular accident (CVA) or post-procedure occlusion of the radial artery (clinical diagnosis before discharge confirmed by echo-doppler);
b) Procedural efficacy according to approach. For CA this was judged by: percentage crossover to the other approach; selective intubation of the coronary arteries; bypass grafts and left ventricle; number of catheter used; total procedure duration (from first puncture attempt to withdrawal of the last catheter); X-ray exposure time and volume of contrast medium used. For PCI this was judged by: percentage crossover to the other approach; primary success (all lesions successfully treated without complications); angioplasty-related cardiac complications; number of catheter used; procedure duration (from first puncture attempt to withdrawal of the last catheter or from guiding catheter insertion to guiding catheter removal in ad hoc procedures); X-ray exposure time and volume of contrast medium used.
Coronary angiography
Approach selection (radial or femoral: left or right) was at the operator’s discretion according to the context (pulse, presence of unilateral vascular occlusion, left radial route in the presence of an in situ left mammary graft). Selection of the puncture and catheterisation equipment was also left to the operator’s preference.
Percutaneous coronary intervention
The decision to perform coronary angioplasty immediately after angiography (ad hoc PCI), or later with the arterial sheath left in place, was at the discretion of the operator as was the choice of guide-catheter shapes and all PCI equipment. Femoral closure devices could also be freely used according to operator preference. (Perclose, Abbott Vascular Devices, Redwood City, CA 94063, USA or Angioseal, St Jude Medical, Diag Division, Minnetonka, MN 55345, USA).
Statistical analysis
Data were collected for each procedure attempted (i.e., for coronary angiography, coronary angiography plus PCI, or PCI alone). If a patient underwent two procedures during the study period, (e.g., for angiography, then later for angioplasty) they were included on both occasions. Continuous data are expressed as mean±SD, and categorised data as proportions. Continuous data are compared by t-test and categorised by chi square (χ2). A p value <0.05 is considered significant. Results were analysed by intention-to-treat. Due to the crossover rate, a per protocol analysis was also scheduled.
Results
Centres
Patients were included from the following centres:
Hôpital Européen de Paris la Roseraie (n=83), Hôpital Bichat (n=18), Institut Jacques Cartier, Massy (n=87), Meixoeiro University Hospital (n=53), Bergamo (n=50), Sussex Cardiac Center Brighton and Sussex (n=45), Hôpital Claude Galien (n=45), Riga (n=48), Centre Universitaire de la Côte de Nacre (n=32), Szeged (n=24), Barcelona (n=17), Hôpital du Val-de-Grâce (n=19), Valle de Hebron (n=18) and Santa Cruz (n=16).
Patient population
For the total studied population, mean age was 60.8±10.9 years (29-85 years), mean weight 106.9±14.8 Kg (78-160 Kg), mean height 1.67±0.10 m (1.4-1.9 m) and mean BMI (38.5±3.6 Kg/m2 (33.6-56.7 Kg/m2). In the studied population there were 318 males (57.3%). The numbers of patients with cardiovascular risk factors were respectively: hypertension 404 (72.8%); hypercholesterolaemia 365 (65.8%); family history of cardiovascular disease 132 (23.8%); diabetes mellitus 189 (34.1%); current or previous smoker 207 (37.3%). In this population there was a history of previous myocardial infarction in 92 patients (16.6%), previous CABG in 33 patients (5.9%), previous PCI in 89 patients (16%), previous stroke in four patients (2,3%) and peripheral vascular disease in nine patients (5.1%). CA represented 64.3% of the cases, PCI 11.6%, and CA with PCI 24.1%.
CA was indicated for the exploration of a valvulopathy in 6.1%, cardiac insufficiency in 4.7% and for ischaemic reasons in 89.2%. Clinical indications were stable angina in 51%, acute coronary syndrome with ST elevation in 10%, acute coronary syndrome without ST elevation in 17%, silent ischaemia in 12% and for non-ischaemic reasons in 10%. Ischaemia was documented in 60.5% of cases: ECG in 33.9%; nuclear medicine tomography in 18.1%; stress test 6.6% and other in 1.9%.
Results for coronary disease extent in the overall population were: no significant lesion in 22.9%; one vessel disease in 40.7%; two vessels disease in 21.9%; three vessels disease in 14.5% and significant left main lesion in 4.1% of the cases.
The size of vascular access site was respectively: 4 Fr in 7%; 5 Fr in 59.4%; 6 Fr in 31.2%; 7 Fr in 2.2% and 8 Fr in 0.2%.
The rate of TR approach by intention to treat was 398/555 (71.7%) and after crossover was 391/346 (70.5%). Transradial access was chosen for the following reasons: physician choice (n=524, 94.4%); dialysis or fistula (n=4, 0.7%); need for 7 Fr catheters (n=5, 1.0%); abnormal Allen test (n=3, 0.5%); CABG (n=6, 1.1%); none, or too small radial (n=7, 1.3%); vascular disease (n=3, 0.5%); failed punction (n=2, 0,4%); other reasons (n=1, 0.1%). The rate of crossover was 25/555 (4.5%): radial to femoral for 12 patients (2.2%); radial to radial for 5 (0.9%); femoral to radial for seven (1.3%); and radial to ulnar for 1 (0.2%).
The rate of success and difficulties in the radial group (n=398) were: success without difficulty for 336 patients (84.4%); failure for 14 patients (3.5%); catheterisation difficulties for 16 patients (4%); spasm for 12 patients (3%); loops for 15 patients (3.8%); and other difficulties for 3 patients (0.8%). Overall difficulties were present in 60 patients (15.1%).
Baseline patient clinical characteristics are listed in Table 1 for both groups; femoral group (n=157 patients) and radial group (n=398 patients).
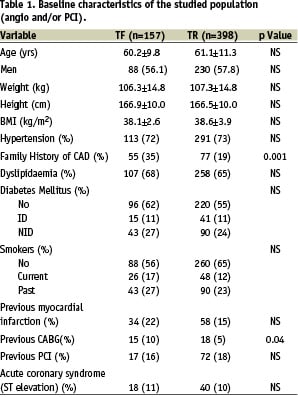
Clinical characteristics were similar in both groups, we only found a significantly higher rate of family history of coronary artery disease in the radial group (35% versus 19%, p=0.04) and a higher rate of previous CABG (10% versus 5%, p=0.001) in the femoral group (Table 1).
The proportion of CA and PCI was in the TR group: CA 67.1%, PCI 9% and CA with PCI 23.9%. TF group CA 57.3%, PCI 17.8% and CA with PCI 24.9%. CA represented 64.3% of the cases, PCI 11.6%, and CA with PCI 24.1% (p <.01).
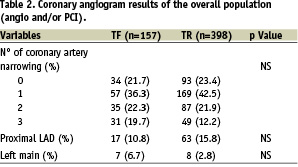
Coronary disease extension and the rate of left main disease were similar in both groups (Table 2).
The antiplatelet and anticoagulant therapy at the time of catheterisation was similar in both groups: aspirin (TR: 342 patients [85.9%] versus TF: 157 patients [86.6%], NS); clopidogrel (TR: 139 patients [34.9%] versus TF: 56 patients [35.7%], NS); heparin (TR: 258 patients [64.8%] versus TF: 99 patients [63.0%], NS); glycoprotein IIb/IIIa receptor blockers (TR: 28 patients [7.0%] versus TF: six patients [5.7%], NS). Only four patients received thrombolytic therapy all in the TR group.
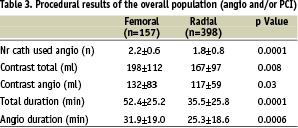
Procedure results are listed Table 3.
For the PCI group (n=198 patients), TR access was achieved in 123 patients (62%) and TF access in 75 patients (38%), PCI success (per vessel) was reached in 260/269 (97%), clinical total success in 190 patients (96%), QMI in four patients (2.1%), MACE in two patients (1%), emergency CABG in 0 (0%) and death, 0 (0%). Only one patient had a CVA in the TF group (0.6%), none in TR group (NS). Two patients (0.5%) in the TR group had a documented radial artery occlusion without any clinical consequence. No patient in either group had cholesterol embolisation.
Results for hospital stay duration and vascular complications are listed Table 4 and were respectively: hospital stay duration (TR: 3.6±3.9 d versus TF:4.2±4 d, NS); hospital stay duration after CA or PCI (TR: 1.8±2.3 d versus TF 2.5±4.3 d, p=.04); the rate of important haematoma was three patients (0.8%) in TR group versus four patients (2.5%) in TF group, p=0.09; vascular complication delaying hospital discharge and/or transfusion in three patients (0.8%) in TR group versus eight patients (5.1%) in TF group, p=0.0009; clinical haematoma seven patients (1.8%) in TR group versus 16 patients (10.2%) in TF group p=0.0001, combined endpoint (vascular complication, transfusion, CVA, radial occlusion and cholesterol embolisation) in nine patients (5.7%) in TF group versus four patients (1%) in TR group p=0.003 (see figure 1).
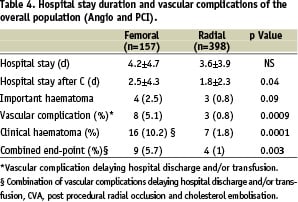
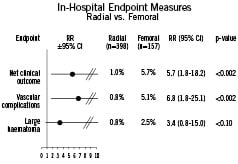
Figure 1. In-hospital endpoints.
Radial occlusion occurred in four patients (1%).
Closure devices were used in 13 patients (8.3% of TF group). We also observed a significant difference for the occurrence of primary endpoint in the PCI group with or without CA: TR (n=131) two patients (1.5%) versus TF (n=67) five patients (7.5%), p < 0.05. Similar results were found in the coronary angiogram group: TR (n=267) two patients (0.8%) versus TF (n=90) four patients (4.4%), p< 0.05.
Discussion
Obesity is associated with an increased long-term risk of cardiovascular death and hospital admission due to a wide range of cardiovascular problems in addition to coronary heart disease in both men and women2. Body weight has implications for mortality2,5. A direct or indirect relationship has been established between obesity and insulin resistance, type II diabetes, dyslipidaemia, inflammation, thrombosis, hypertension, atherosclerosis, and stroke6,7. It is known that obesity is a strong risk factor for the development of coronary artery disease (CAD).
Several reports have found extremes of BMI to be associated with worse outcomes. Ellis et al found patients with BMI of ≤ 25 kg/m2 and ≥ 35 kg/m2 to have an increased mortality after PCI, with higher rates of in-hospital mortality4. Powell et al found a similar relationship between mortality and BMI after PCI, with an increased risk at the very extremes of BMI8.
In obese patients, difficulty gaining femoral arterial access and achieving post-procedural haemostasis, as well as delay in the recognition of poor haemostasis, leads to an increased risk for vascular complications. Frequently in obese patients, the puncture is done very deeply in the inguinal pleat with secondary problems of haemostasis. It has been reported that the risk of vascular complications for cardiac catheterisation is greater in obese patients3,4. In a multivariate analysis of 18,137 PCI patients in northern New England (1997-1999), the rate of vascular complications was 2.98% and one of the variables associated with increased risk was the body surface area <1.6 m (OR 1.9) related to body weight9. For Ammann, vascular complications were also significantly increased in overweight patients undergoing diagnostic coronary angiogram10. On the other hand, several recent studies have suggested a paradoxical protective effect of obesity11. In the study reported by Cox et al, obese patients had less vascular complications than non-obese patients12. He found a U-shaped relationship between weight and the rate of vascular complications, with peaks of risk at the lowest BMI and highest BMI subgroups. He also found a significantly reduced rate of vascular complications in obese patients with transradial approach (80% reduction, 0.7% versus 4.0% in patients with femoral access, p=0.04), and non-obese patients (60% reduction, 2.1% versus 5.3% in patients with femoral access, p=0.05). In this retrospective study, the rate of using closure devices for femoral access was high, 71.7% in the total population and 80.3% in the obese patients group. In this study, logistic regression identified the non-use of radial access, the performance of PCI, female gender, older age and the use of glycoprotein IIb/IIIa antagonists as independent risk factors for vascular complications. Radial artery use was the most powerful independent predictor for a reduction in the risk of vascular complications in obese patients. The transradial approach reduces the rate of vascular complications in all patients13, although this reduction might be enhanced in a high risk group such as obese patients. Vascular complications worsen the prognosis of patients and increase the hospital stay with financial consequences. The transradial approach for CA and for PCI decreases the risk of vascular events, and decreases the length of post-procedural in hospital stay. Not much data for the transradial approach in obese populations is available. This prospective registry compared the femoral to the radial approach for CA and/or PCI, in very overweight patients (BMI ≥ 35 kg/m2), in centres with a wide experience of transradial approach, demonstrating that the rate of haematoma was significantly higher in the transfemoral group, 10.2% versus 1.8% in transradial group (p<0.0001); the rate of vascular complications in the transfemoral group, 5.1% versus 0.8% in transradial group (p<0.0009). In the TROP registry, the proportion of PCI was significantly higher in the TF group. However, the primary endpoint was significantly more frequent in the TR group in patients with PCI, with or without CA, and in patients with CA alone. The post procedural in-hospital stay was significantly longer in the transfemoral group (2.5±4.3 days versus 1.8±2.2 days in transradial group, p=0.04). This study also showed the feasibility of the transradial approach in very overweight patients, with a success rate of 96% and no difficulty observed in 84.4% of the cases. The mean number of catheters used for each procedure was significantly less in the transradial group (1.8±0.8 versus 2.2±0.6 in the transfemoral group, p=0.005) and the procedural duration for CA and PCI were significantly shorter in the transradial group. But, CABG patients were preferably studied transfemorally. Therefore, there was no greater difficulty for the transradial approach compared to the transfemoral group in very overweight patients for a well trained physicians. In this registry, physicians were highly experienced in the transradial approach, with a rate superior to 80% of transradial approach in daily practice and a learning curve of more than 1,200 procedures. The rate of crossover was 4.5%, radial to femoral in 2.2% of cases and femoral to radial in 1.3%. For the TR approach, the rate of catheterisation difficulties, spasm and loops were low respectively 4%, 3% and 3.8%. In a study reported by Cha et al, BMI, age and hypertension were independent predictors of tortuous right subclavian arteries increasing the difficulty of the right radial approach14. In this study the rate of crossover to left radial or femoral was 4%14. Another difficulty in the TR approach must be described: radial artery calcification, more frequent in diabetes mellitus, a common cardiovascular risk factor in obese patients15.
The main limitation of this study was the non-randomised design. In addition, the use of closure devices was low in the TF group.
Conclusions
Obesity is a risk factor for coronary artery disease, and also for mortality and morbidity with percutaneous coronary intervention. The risk of vascular complications through the transfemoral approach for coronary diagnostic procedures or interventions is higher in obese patients. The transradial approach in very obese patients, performed by skilled operators, potentially reduces the rate of access-related vascular complications.
Appendix
Participating centres and patients recruited: Hôpital Européen de Paris la Roseraie, Aubervilliers, France (H. Benamer, C. Gaultier) (n=83), Hôpital Bichat, Paris, France (H. Benamer) (n=18), Institut Jacques Cartier, Massy, France (P. Dumas, T. Lefèvre, Y. Louvard, M.-C. Morice) (n=87) Meixoeiro, Spain (M. Sanmartin, Mantilla, Baz, Ocaranza, Goicolea) (n=53), Ospedali Riuniti Bergamo, Italy (O. Valsecchi, A. Vassileva, G. Guagliumi, G. Musumeci) (n=50), Sussex Cardiac Center Brighton and Sussex, United Kingdom (D. Hildick-Smith) (n=45), Hôpital Claude Galien, Quincy-sous-Sénart, France (Ph. Garot, O. Tavolaro) (n=45), Riga, Latvia (I. Narbute, Dombrovskis, Latkouskis, Kalnins, Trusinskis, Lismanis, Apinis) (n=48), Centre Hospitalier Universitaire de la Côte de Nacre, Caen, France (G. Grollier, R. Sabatier, M. Hamon) (n=32), University of Szeged, Hungary (I. Ungi) (n=24), Barcelona, Spain (RJ. Ruiz-Salmeron) (n=17), Hôpital du Val-de-Grâce, Paris, France (J. Monségu, P. Schiano) (n=19), Valle de Hebron (n=18), and Santa Cruz (n=16), San Pablo, Spain (Martin, Pijuan, Domingo, Garcia, Guiteras).

