Abstract
Aims: Side branch (SB) occlusion is one of the major technical hurdles in the percutaneous coronary intervention (PCI) of bifurcation lesions. Our aim was to investigate whether preprocedural coronary computed tomography angiography (CCTA) could predict intraprocedural SB occlusion.
Methods and results: A total of 260 bifurcation lesions were enrolled from 246 patients who underwent CCTA before elective bifurcation PCI. Quantitative plaque analysis was performed in the main vessel (MV) and SB. Intraprocedural SB occlusion occurred in 42 lesions (16%). These lesions were characterised by SB plaque, calcified plaque in the MV, low attenuation plaque in the main proximal segment or SB, and a ratio of MV to SB ostium area >4.3, which constituted a point-based CT bifurcation score. The CT bifurcation score was cross-validated, outperforming any angiographic Medina classification or RESOLVE score (c-statistics=0.749 versus 0.631 to 0.551; p<0.05 for all). The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of the CT bifurcation score ≥1 were 90%, 42%, 23%, 96%, and 50%, respectively.
Conclusions: Comprehensive CCTA assessment was able to predict intraprocedural SB occlusion better than the current angiographic classification or scoring system. The CT bifurcation score may thus be a helpful guide for selecting the optimal bifurcation PCI strategy.
Introduction
The coronary artery tree forms a hierarchical network of branching tubes to provide efficient transport of materials. However, its branching nature causes complex local flow disturbance at a bifurcation site, which is frequently followed by localisation and progression of atheroma1. As a result, bifurcation lesions are not uncommon and are found in up to one out of every five percutaneous coronary interventions (PCI). A bifurcation lesion may suffer from side branch (SB) occlusion after dilatation of a balloon or implantation of a stent in the main vessel (MV)2. This frequently results in implantation of another stent in the SB, rewiring failure, or periprocedural myocardial infarction. If the risk of SB occlusion can be predicted before a PCI procedure, a provisional or aggressive SB treatment strategy can be selected appropriately, which may lower the risk of SB occlusion or save unnecessary SB stenting3,4.
Intracoronary imaging studies have identified that the location or extent of plaque burden, or vessel dimensions are related to SB occlusion5,6. Coronary computed tomography angiography (CCTA) enables a comprehensive non-invasive visualisation and quantitation of atherosclerotic plaque as well as luminal stenosis7,8. Therefore, we reasoned that CCTA could predict SB occlusion in a similar way to or better than coronary angiography. The present study evaluated the predictive value of CCTA for SB occlusion in bifurcation PCI.
Methods
STUDY POPULATION
We retrospectively identified patients who underwent preprocedural CCTA followed by clinically indicated PCI for a bifurcation lesion from January 2006 to March 2015. Inclusion criteria were 1) elective PCI for a bifurcation lesion with a visually estimated SB diameter ≥2.0 mm and 2) CCTA within 90 days before PCI. Exclusion criteria were 1) culprit lesion of an ST-elevation myocardial infarction, 2) haemodynamically unstable status, 3) the presence of a patent bypass graft to the target vessel, 4) elective two-stent implantation, 5) the presence of a previously implanted stent in the target lesion, and 6) inadequate CCTA quality. This study investigated anonymised imaging and used the procedural database. Informed consent was allowed to be waived and the study was approved by the Samsung Medical Center Institutional Review Board.
ACQUISITION AND INTERPRETATION OF CCTA
CCTA was performed as previously described9. In brief, a 64-slice (Aquilion 64; Toshiba Medical Systems, Otawara, Tochigi, Japan) or 128-slice scanner (SOMATOM® Definition Flash; Siemens Healthineers, Erlangen, Germany) was used. CT images were analysed by imaging specialists supervised by a radiologist using a cardiovascular workstation (iNtuition; TeraRecon, Foster City, CA, USA). We adopted the concept of in-segment restenosis of the stent to the bifurcation anatomy and set the margin of the adjacent plaque that might affect SB jailing at 5 mm10. The bifurcation lesion was divided into six segments of interest which covered the proximal and distal 5 mm segments from the bifurcation confluence (Figure 1). The proximal and distal segments were divided into branch side and contra-branch (opposite the branch) side, respectively. Plaque in the bifurcation confluence was assigned to the contra-branch ostial side segment. The SB segment was the 5 mm segment from the SB ostium. Both dichotomous and quantitative assessments were carried out in each segment. The presence of plaque was defined by a diameter stenosis (DS) of ≥50% or an area stenosis of ≥75% within the segment of interest. The vessel area and lumen area were measured at the MV proximal or distal 5 mm from the bifurcation confluence and the SB ostium. SB plaque exceeding 5 mm in length was counted separately. Quantitative plaque volume of low attenuation, fatty, fibrous, and calcified plaque (defined by radiologic attenuation of –150-29, 30-149, 150-349, and 350-1,000 Hounsfield Units [HU]) was assessed in each segment of interest. To minimise imaging bias, plaque characteristics were determined in contiguous plaque occupying at least ≥1 mm.
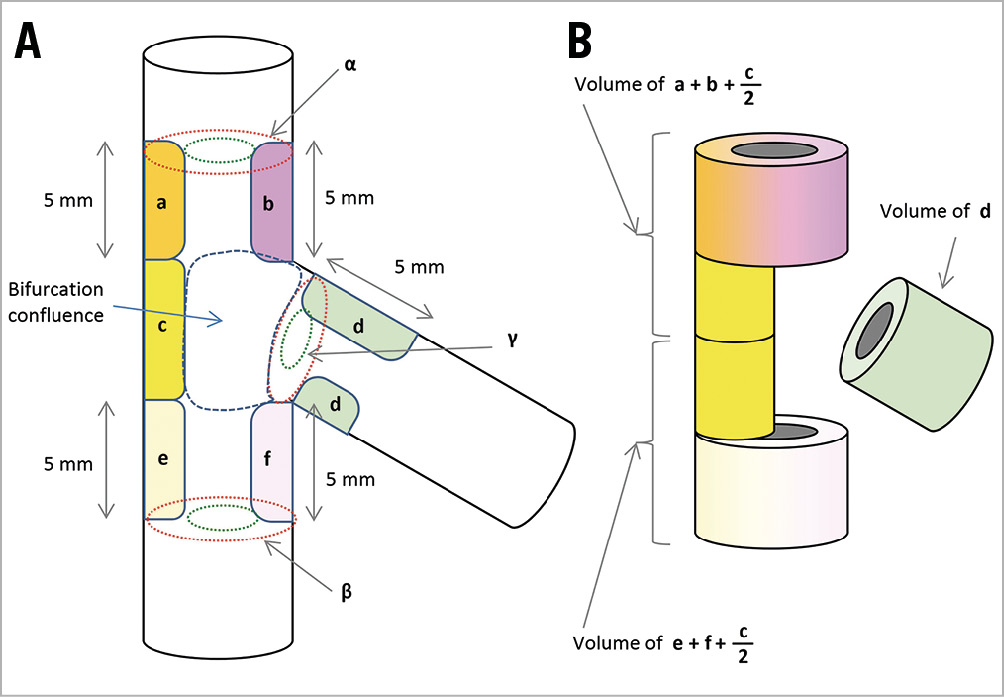
Figure 1. Schematic illustration of bifurcation plaque analysis using CCTA. A) Six segments of interest with 5 mm axial length except segment c. Segment (a) main vessel (MV) proximal contra-branch side, (b) MV proximal branch side, (c) MV contra-ostial side, (d) side branch (SB) ostium, (e) MV distal contra-branch side, (f) MV distal branch side. B) Plaque volume. α: MV proximal vessel and luminal area; β: MV distal vessel and luminal area; γ: SB ostial vessel and luminal area
CORONARY ANGIOGRAPHY AND PCI
Elective PCI was performed for patients who had significant stenosis on CCTA. The choice of treatment strategy and technique was at the discretion of the interventional cardiologist. Periprocedural myocardial infarction was defined as a tenfold increase of CK-MB compared to the upper limit of normal value (5.0 ng/ml)11. Intraprocedural SB occlusion was defined as development of SB flow with Thrombolysis In Myocardial Infarction (TIMI) flow ≤1 after ballooning or stenting in the MV.
Computer-assisted bifurcation quantitative coronary angiography (QCA) was performed by independent technicians using a dedicated system (QAngio® XA 3D; Medis, Leiden, the Netherlands). The reference diameter (RD), minimal luminal diameter (MLD), diameter stenosis (DS), and length were assessed in the proximal MV, the distal MV, the SB, and the bifurcation core segment, respectively, using the end-diastolic image. The bifurcation angle and the diameter ratio between the MV and SB were also assessed. Angiography-based bifurcations were classified using the Medina classification and the RESOLVE (Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion) score6,12. In brief, the RESOLVE score is the sum of the following parameters: plaque distribution, TIMI flow of the MV, bifurcation angle, the diameter ratio between the MV and SB, and the DS of the SB. The RESOLVE score ranges from 0 to 43. In a prior study, the RESOLVE score predicted SB occlusion risk from 0% to 19.8% according to a score of ≤2 to ≥10 and showed a c-statistic of 0.776.
STATISTICAL ANALYSIS
All analysis was performed on a per-vessel basis unless otherwise indicated. The inter-rater agreement and reproducibility of the measurement were validated in 40 randomly selected vessels using Cohen’s weighted kappa. The weighted kappa for intra-observer variability and inter-observer variability was 0.809 and 0.826, respectively. The angiographic, procedural, and plaque characteristics of the bifurcations with SB occlusion and bifurcations without SB occlusion were compared using the t-test or Mann-Whitney test. The dose-response relation among categorical and continuous parameters was assessed using the Jonckheere-Terpstra test. The optimal cut-off of continuous variables was defined by receiver operating characteristic (ROC) with Youden’s methods. In multivariate analysis, a subset of parameters predicting SB occlusion was selected based on least absolute shrinkage and selection operator (LASSO), which is a regression analysis that fits a generalised linear model via penalised maximum likelihood and select variables13. The discriminative performance was quantitated by ROC and reclassification analyses including net reclassification improvement (NRI) and integrated discrimination improvement (IDI). Scores were compared using Venkatraman’s method14. R version 3.5 (R Foundation for Statistical Computing, Vienna, Austria) was used. A two-tailed p<0.05 was considered statistically significant.
Results
CLINICAL, ANGIOGRAPHIC, AND PROCEDURAL CHARACTERISTICS
In the recruitment period, a total of 581 bifurcation PCI were performed. We identified 303 patients who underwent preprocedural CCTA before elective PCI for a bifurcation lesion. After exclusion of patients according to criteria, a total of 246 patients were enrolled (Figure 2). The median interval between CCTA and PCI was 16 days (1st-3rd quartile, 8-33 days).
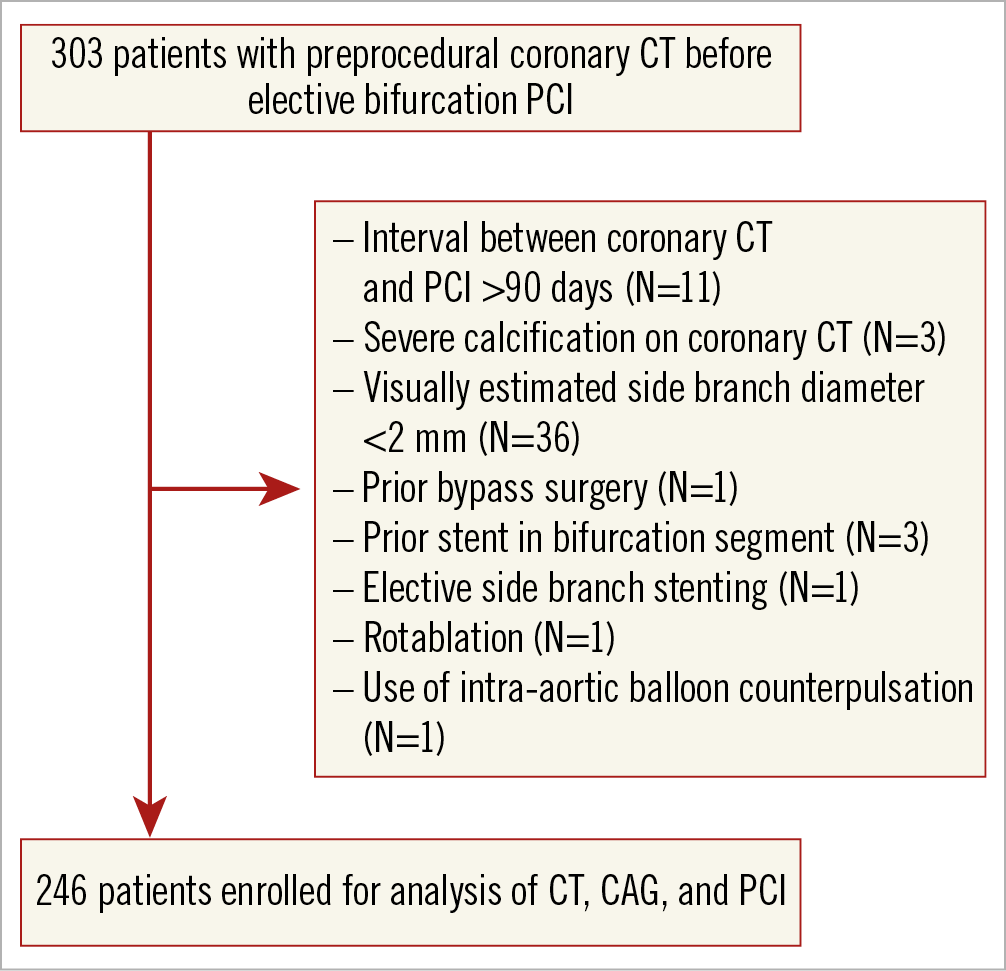
Figure 2. Patient flow chart
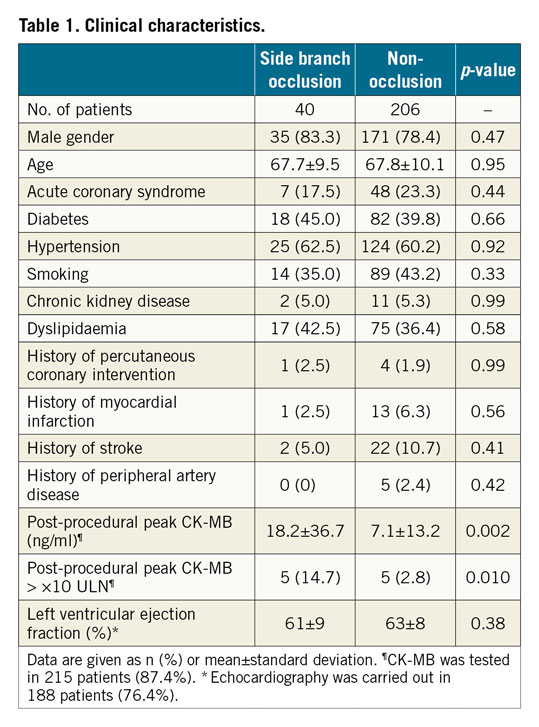
Of a total of 260 lesions from 246 patients, intraprocedural SB occlusion occurred in 42 (16%) lesions. In per-patient analysis, there were no differences in clinical characteristics between the SB occlusion and non-occlusion groups. Post-procedural CK-MB was higher in the SB occlusion group compared with the non-occlusion group (p<0.001) (Table 1). In a per-vessel analysis of angiographic characteristics, the most frequently occluded SB was a diagonal branch in the left anterior descending artery. SB occlusion risk was highest (26%) in type 1,1,1 bifurcations according to the Medina classification. Compared with the non-occlusion group, the SB occlusion group showed larger RD, smaller MLD, and higher DS in the proximal MV and SB segments (p<0.05 for all) but not in the distal MV segment (p=NS). The SB occlusion group also showed smaller MLD and higher DS in the bifurcation core segment (p<0.05 for all), and a higher RESOLVE score (10.6±5.2 versus 8.4±4.9, p=0.010) and larger stent diameter (3.39±0.64 versus 3.11±0.48 mm, p=0.006) compared with the non-occlusion group. There was no significant difference in bifurcation angle, preprocedural TIMI flow of the MV or SB, or MV plaque distribution between the two groups (Supplementary Figure 1).
CCTA CHARACTERISTICS
SB ostial plaque was more often found in the SB occlusion group compared with the non-occlusion group (64% versus 36%, p=0.001) (Supplementary Table 1). In addition, SB ostial plaque, SB ostial luminal diameter, and the ratio of MV segment to SB ostium were different between the two groups (p<0.05 for all). Calcified plaque in the proximal MV segment, small SB size (represented by an MV to SB vessel area ratio >4.3), and high SB plaque burden (represented by an SB plaque length ≥5 mm) were more common in the SB occlusion group (45% versus 19%; 38% versus 14%; 38% versus 15%, p≤0.001 for all). There was also a marked tendency towards a higher frequency of low attenuation plaque in the proximal MV or SB segment in the SB occlusion group (31% versus 17%, p=0.059). The volumetric analysis of six segments of interest also did not show any difference in plaque volume between the two groups except for a higher SB plaque burden in the SB occlusion group (0.73±0.12 versus 0.65±0.12, p<0.001) (Supplementary Table 2).
DEVELOPMENT OF CT BIFURCATION SCORE
For multivariate analysis, a LASSO analysis was carried out to select the CT parameters to be included in the final model, which were plaque in the SB, calcified plaque in the MV proximal segment, necrotic plaque in the MV proximal or SB segment, and an MV to SB vessel area ratio >4.3 (Supplementary Table 3). Each parameter was assigned one point to create the CT bifurcation score which ranges from 0 to 4 (Figure 3). The prediction model was tested by exhaustive leave-one-out cross-validation which showed similar accuracy of the model (0.84) and cross-validation (0.83). Representative cases are shown in Figure 4.
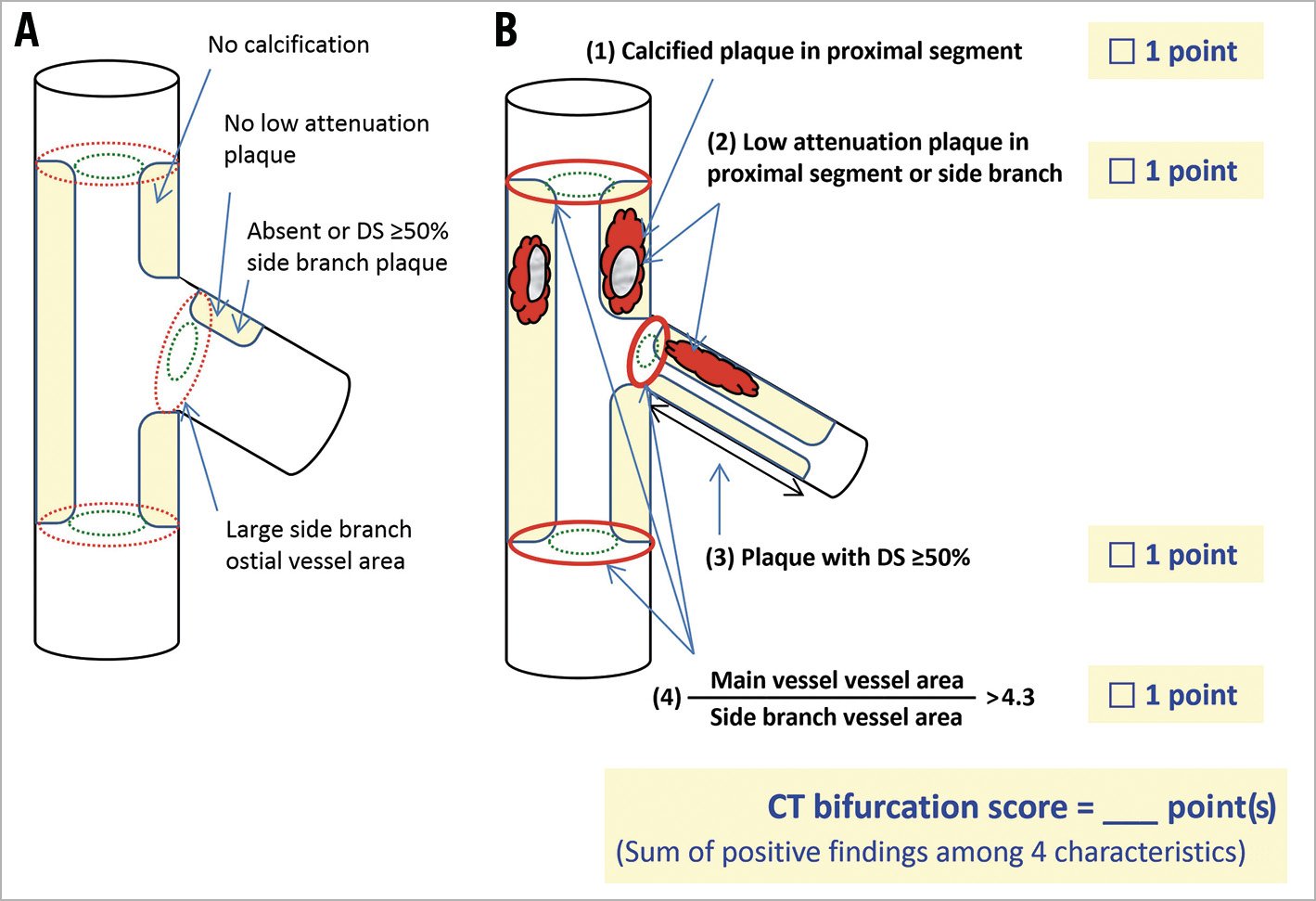
Figure 3. CT bifurcation score. A) Bifurcation with a low risk of intraprocedural SB occlusion. B) Bifurcation with a high risk of intraprocedural SB occlusion and calculation of CT bifurcation score.
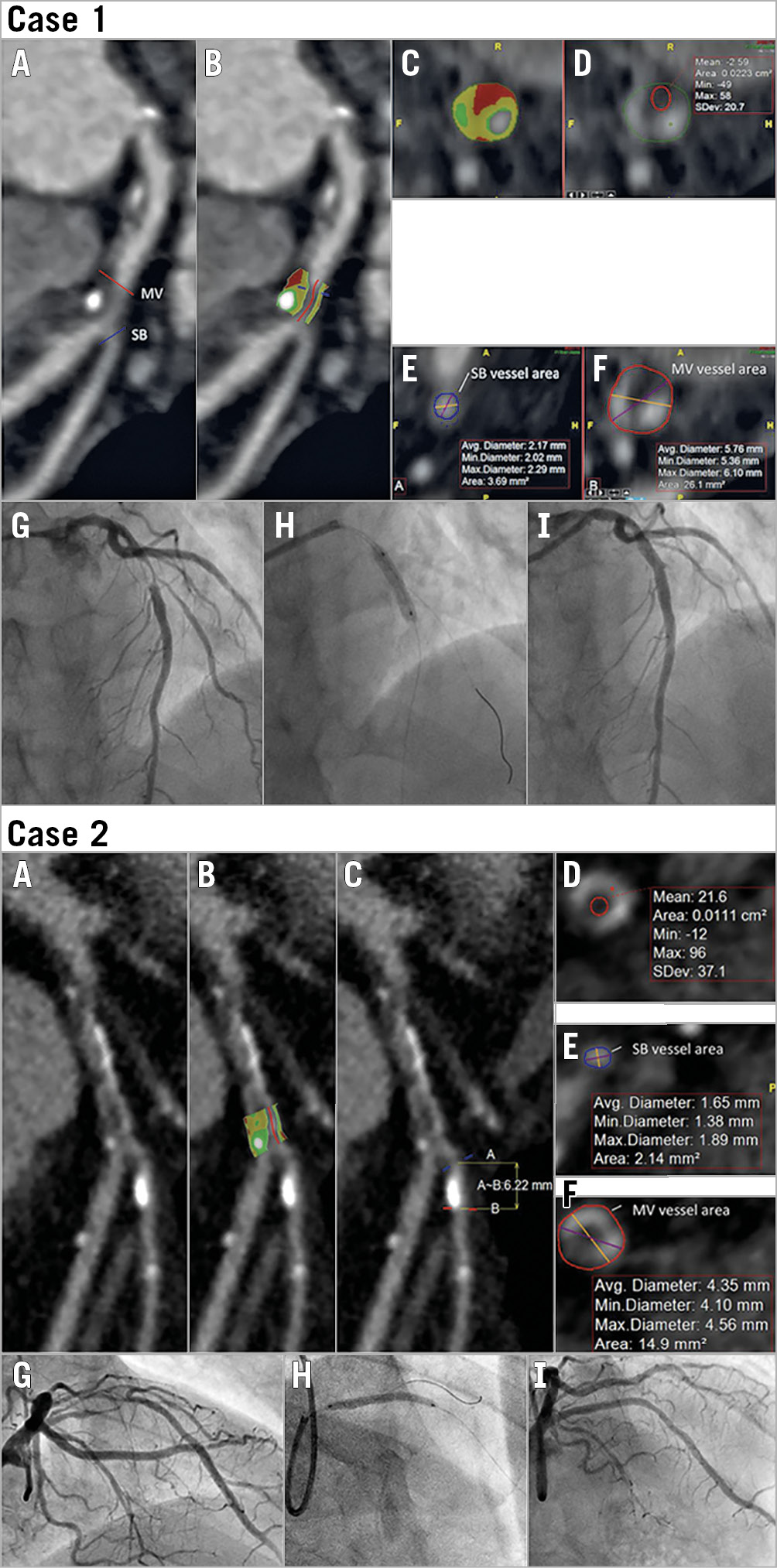
Figure 4. Representative cases of intraprocedural side branch occlusion. Case 1. The plaque characteristics in the MV are shown using different colours. Red, low attenuation (–150-29 HU); yellow, fatty (30-149); green, fibrous (150-349); white, calcified (350-1,000). A) & B) Curved multiplanar reconstruction image of CCTA. C) - E) Notice the calcified and low attenuation plaque in the proximal MV segment, and the large MV/SB vessel area ratio. The CT bifurcation score was 3. G) - I) Angiographic basal, stenting, and final images. Diagonal flow became TIMI=0 after MV stenting. Case 2. A) - F) The CT bifurcation score was 3. G) - I) Diagonal flow became TIMI=0 after MV stenting.
CT BIFURCATION SCORE VERSUS ANGIOGRAPHIC CLASSIFICATIONS
The risk of SB occlusion increased proportionally from 4.2% to 64.7% according to a CT bifurcation score of 0 to ≥3 (Figure 5A), whereas it increased moderately from 8.6% to 22.9% according to RESOLVE score quartiles (Figure 5B), and from 0% to 26.4% according to Medina classification (Figure 5C). By pairwise comparison, the CT bifurcation score showed higher predictive performance for SB occlusion (c-statistic=0.749) compared with the RESOLVE score (c-statistic=0.627) or Medina classification (c-statistic=0.631 to 0.551) (p<0.05 for all) (Figure 5D). The CT bifurcation score also consistently improved reclassification of prediction by the RESOLVE score or Medina classification (categorical NRI=0.23, continuous NRI=0.65-0.71, IDI=0.11-0.14, p<0.01 for all) (Supplementary Table 4). The optimal cut-off of the CT bifurcation score was ≥1, which showed sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of 90%, 42%, 23%, 96%, and 50%, respectively (Supplementary Table 5).
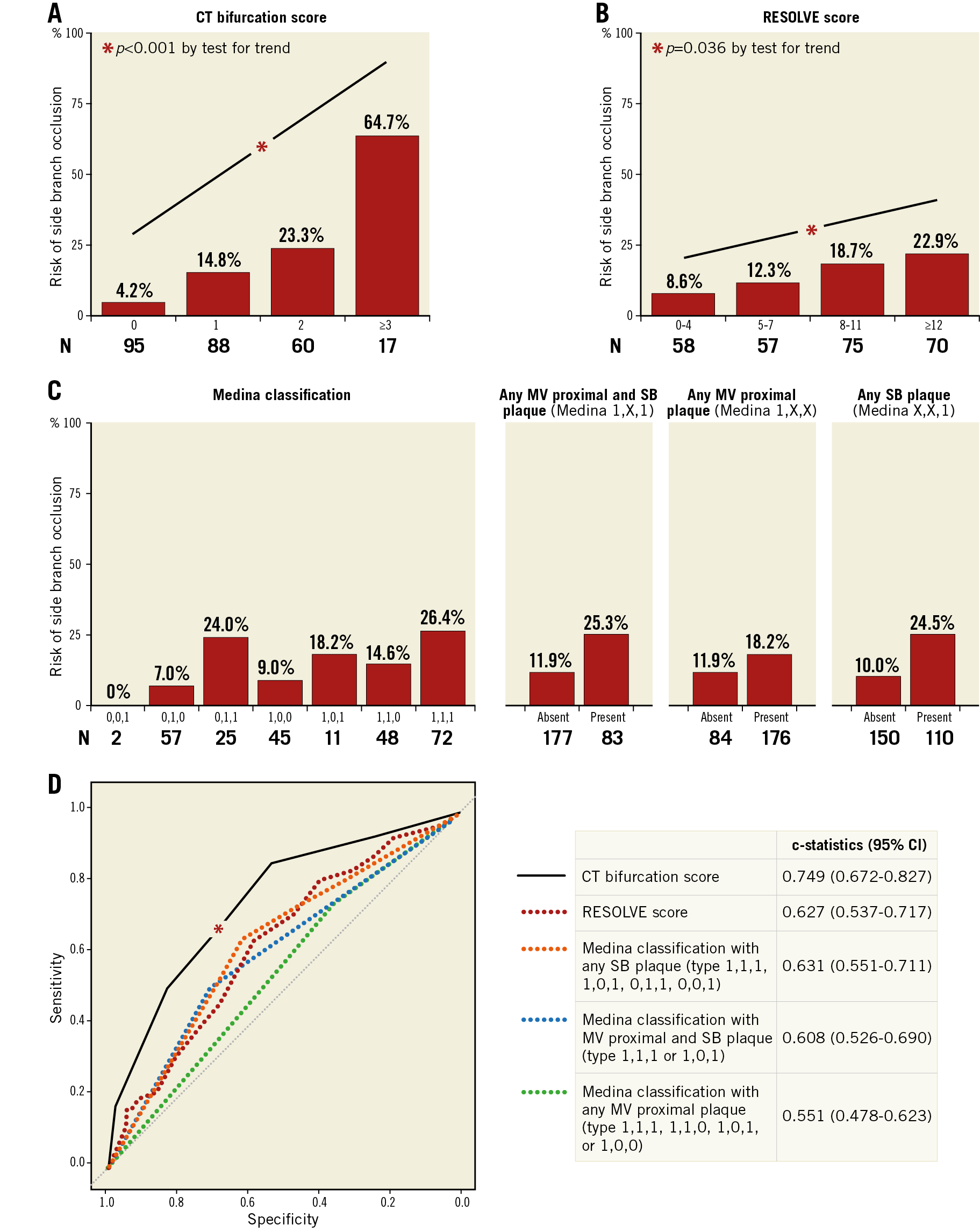
Figure 5. Risk of side branch occlusion according to the CT bifurcation score or angiographic classification. The risk of SB occlusion increased proportionally according to the CT bifurcation score (A) or RESOLVE score (B). Among Medina classifications, the risk of SB occlusion was highest in type 1,1,1 (26.4%). X stands for 0 or 1 (C). *CT bifurcation score versus RESOLVE score (p=0.017), versus Medina classifications (p<0.01 for all) (D).
Discussion
In this study, plaque characteristics imaged by CCTA were able to predict intraprocedural SB occlusion. A novel and simple point scoring system based on four CT parameters, the CT bifurcation score, was cross-validated and showed better performance compared with angiographic Medina classification or the RESOLVE score. Intriguingly, the nature of plaque (represented by calcified or low attenuation plaque) contributed much more to SB occlusion than anatomical plaque burden in the segment of interest.
IMPACT OF PLAQUE CHARACTERISTICS ON SB OCCLUSION
No bifurcation classification, including the Medina classification, was designed to predict SB occlusion. In the COBIS registry, only plaque burden in the proximal MV and SB was an anatomic predictor of SB occlusion15. The recently reported RESOLVE score showed a fair predictability of SB occlusion; however, it needs a meticulous measurement of QCA, which makes it challenging for clinical application6. Interestingly, bifurcation angle is one of the major parameters in the RESOLVE score but was controversial in COBIS and other studies16.
The key mechanism of SB occlusion has been postulated to be carina or plaque shift, but there is emerging evidence about the role of plaque characteristics in SB occlusion. Intravascular ultrasound (IVUS) and optical coherence tomography (OCT) studies have shown that the presence of calcification, attenuated plaque, or lipid pool in the bifurcation was related to the development of intraprocedural SB occlusion or stenosis17,18,19. The addition of our results to previous IVUS or OCT studies suggests the following consequence as a hitherto unknown mechanism of SB occlusion. Disruption of calcification or low attenuation plaque by ballooning or stenting might trigger emboli-induced local thrombus formation or vasospasm. A combination of this dynamic thromboembolic milieu with inherent complicated flow disturbance in bifurcated vessels might result in intraprocedural SB occlusion. This hypothetical mechanism could explain the late spontaneous SB flow restoration of 14% in the COBIS registry15. Our result suggests that SB occlusion may share a common pathophysiology of vulner-able or high-risk plaque. As high-risk plaque characteristics such as thin-cap fibroatheroma, large lipid-rich plaque, or microcalcification are more important than anatomical plaque volume or area stenosis in vulnerable plaque, high-risk SB plaque characteristics (including low attenuation plaque or calcification) might be more predictive than anatomical SB stenosis or bifurcation angle in bifurcation PCI.
CCTA ANALYSIS OF A BIFURCATION
Our result is the first of its kind to show a link between plaque characteristics and SB occlusion using a non-invasive modality. The CT bifurcation score consists of four parameters that can be easily assessed in clinical practice. The score was proportional to the risk of SB occlusion and could predict it better than any angiographic Medina classification or the RESOLVE score. Any characteristic among the four CCTA findings showed high sensitivity (86%) for the development of intraprocedural SB occlusion. Evaluating the CT bifurcation score before the procedure may guide the interventional strategy by reducing stent implantation in the SB vessel or reducing unexpected intraprocedural SB occlusion by preventive wiring or balloon dilatation, which may lead to better clinical outcome for patients with bifurcation disease. Discordance between anatomical stenosis and the physiological severity of stenosis is not uncommon in both the MV and SB20. Our result suggests that the link between plaque characteristics and ischaemia demonstrated by recent CT studies might be consistent in bifurcated vessels21.
COMPARISON WITH PRIOR PREDICTORS
The burden of SB plaque was a major predictor of SB occlusion in most studies, and this was reproduced in this study7,15. Our study showed that not only the anatomic dimensions of the plaque but also the nature of the plaque may have a significant role in the development of SB occlusion. Park et al reported that the quantitative thickness or the luminal dimensions of the SB were predictors of SB occlusion7. Our study did not replicate all of their findings, which can be explained by the limited spatial resolution of CCTA in sub-millimetre measurement of plaque dimensions. The angio-graphy-based RESOLVE score could predict SB occlusion but was inferior to the CT bifurcation score6. This might be partially explained by the complicated scoring system and controversial factors such as bifurcation angle. A well-validated multicentre-based angiographic scoring system would be warranted for comparison of CCTA with angiography-based prediction. The incidence of SB occlusion was much higher than that reported in previous studies in which SB occlusion was defined by decreased flow of the SB after MV stenting (8.4% in COBIS, 7.4% in RESOLVE). In this study, SB occlusion was defined by decreased TIMI flow of the SB after MV ballooning as well as stenting.
The CT bifurcation score showed high sensitivity and low specificity for prediction of SB occlusion. Therefore, the appropriate usage of the CT bifurcation score would rule out rather than rule in the risk of SB occlusion. A protective guidewire or a provisional two-stent technique would not be required in case of a score of 0, and might be suggested in the case of a score ≥1.
Limitations
The result was derived from single-centre data. The treatment strategy and technique were not pre-specified. The use of a dedicated bifurcation QCA or CCTA workstation system is still not free from inter- and intra-observer variation22. Plaque characteristics were defined by HU, which can be affected by intraluminal opacification or adjacent radiopacity. The model of the CT bifurcation score was cross-validated but might be different in a larger data set. Further validation of the CT bifurcation score with a larger data set might be required before extrapolation of the CT bifurcation score to other studies and before using the CT bifurcation score for, and as a comparator between, multifarious clinical bifurcation research analytics. The improvement in devices, techniques, and operator experience in the study period was not reflected. This score will require an appropriate update as techniques and equipment are evolving rapidly.
Conclusions
Comprehensive CCTA assessment could predict intraprocedural SB occlusion. The CT bifurcation score, a novel and simple points scoring system based on four CCTA parameters, outperformed current angiographic classification or scoring systems for prediction of SB occlusion. The CT bifurcation score may thus be a helpful guide for selecting the optimal bifurcation PCI strategy.
|
Impact on daily practice The CT bifurcation score predicted side branch occlusion with high sensitivity and moderate specificity. The CT bifurcation score may be helpful in ruling out the risk of side branch occlusion. |
Funding
This study was supported by a Korean Society of Interventional Cardiology grant (#2014-1), the Korean Circulation Society Research Fund (#201301-01), the National Research Foundation of Korea (#2017R1A2B310918), a Samsung Biomedical Research Institute grant (#GL1B33211), and the Heart Vascular and Stroke Institute of the Samsung Medical Center.
Conflict of interest statement
The authors have no conflicts of interest to declare.