Of the many things that should fall into place once this pandemic is behind us, teaching is one of the most important. If you work in an academic centre, you’ve certainly noticed the absence – over the longest period of time – of medical students. If you don’t work in an academic centre, well, you were once a student yourself (or still are!), and so you can perfectly imagine what it’s like to be in the shoes of this generation which has lost a full year of training – at least in a traditional sense.
I am sure some of you will say “but there is remote teaching” – and that’s true. In recent months, many teachers have reinvented themselves as virtual educators, with the help of new technologies. In fact, a smartphone, earphones, and a consenting patient are enough to make each case a moment of reflection for students, with the support of medical charts and live videos and images. The flickering footage and hiccupping audio of this improvised system, if anything, gives a pioneering feel to our many attempts at normality. Incidentally, I have been impressed by the generosity with which many patients accept to be interviewed live – of course with the necessary precautions to protect their privacy – for the benefit of students watching them at home. These patients seem to know better than anyone else that the educational future of these apprentice doctors is at stake during these months.
A pre-professional internship is something that can hardly be replaced, and living in hospitals and wards is an indispensable prerequisite in training. However, it must be recognised that not all evils create a negative situation. Video interaction, in small groups, generates an unexpected level of engagement, encourages questions, and forces the educator to find creative and multimedia solutions to keep the level of attention high. Even when we return to normal, something of this experience and the advances in our ability in the way we communicate will have been useful.
In these months of disruption of traditional educational formats, we hope we have provided a sense of stability, at least with our Journal.
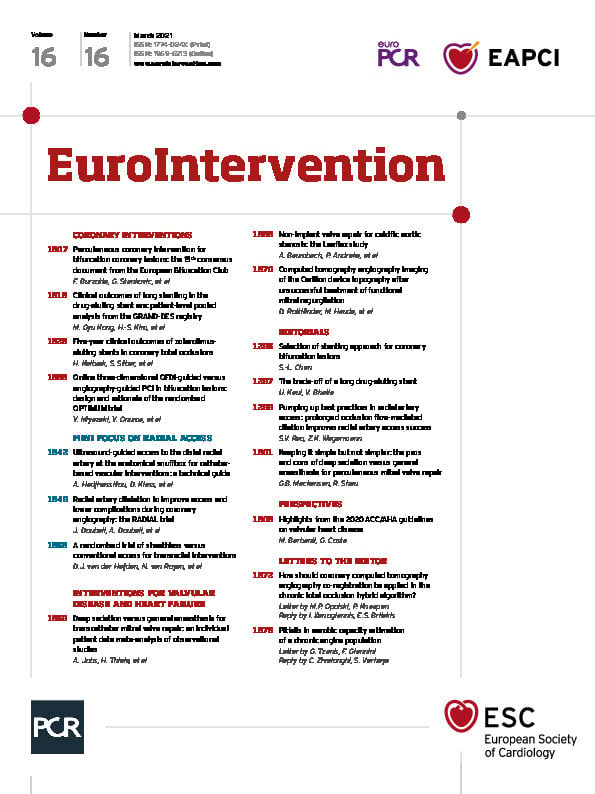
Here is what we have in store for you this month.
Our issue begins with a perspective by Marco Barbanti and Giuliano Costa focusing on the new guidelines from the American College of Cardiology and American Heart Association on valvular heart disease (VHD) which were published in late 2020. The last few years have seen a paradigm shift in the treatment of VHD led by advances in technology and clinical management. From the importance of the multidisciplinary Heart Team in evaluating individual patients, to improvements in imaging technologies and devices, the potential for the use of less invasive approaches in the treatments for VHD is expanding, as this perspective so aptly summarises.
Our clinical articles begin with a consensus document from the European Bifurcation Club on PCI for bifurcation coronary lesions presented by Francesco Burzotta, Goran Stankovic and colleagues, with an editorial by Shao-Liang Chen. The continued and rapid evolution of techniques and devices in the management of bifurcation lesions has led to a wide range of valid clinical options. Clinical challenges and the requisite experience in treating coronary bifurcation lesions and unprotected left main, including in more complex cases, are discussed. Questions such as where we stand on the optimal treatment of side branches or the clinical significance and thresholds for bail-out treatment are considered. New tools and drugs, from intracoronary imaging and bifurcation simulation programmes to drug-eluting balloons and new antiplatelet therapy regimens, are reviewed. Future devices and the necessary trials are also highlighted.
In coronary interventions, Min Gyu Kong, Hyo-Soo Kim and colleagues take a close look at the over 9,000 patients from the GRAND-DES registry who underwent stenting for a single lesion in order to elucidate the relationship of stent length and outcomes using second-generation DES. Stent lengths of longer than 40 mm demonstrated higher percentages of target lesion failure and definite or probable stent thrombosis than seen in shorter length stents, leading the authors to conclude that it is critical to take these longer stent lengths into account when planning treatment and follow-up. This article is accompanied by an editorial by Upendra Kaul and Vineet Bhatia.
Is there a difference in long-term outcomes between patients who have their occluded coronary arteries recanalised and stented as compared to those patients who have their non-occluded arteries stented? This is the subject of an article by Henning Kelbæk, Sigmund Silber and colleagues using pooled results from various trials involving the Resolute zotarolimus-eluting stent. Five-year clinical outcomes were seen to be similar regardless of whether the stents were implanted in total occlusions or not. However, it is not clear if these positive results apply to other new-generation stents.
Yosuke Miyazaki, Yoshinobu Onuma and colleagues present the protocol for the OPTIMUM trial which has been designed to determine if online three-dimensional optical frequency domain imaging-guided PCI is superior to angiography-guided PCI in bifurcation lesions. If proven true, this technique could provide images that would help operators in assessing and rewiring the optimal cell, thus resulting in lower rates of malapposition as compared with angiography-guided PCI.
Radial access in coronary interventions is the subject of this issue’s mini focus. We begin with an article by Anastasia Hadjivassiliou, Darren Klass and colleagues offering step-by-step instructions for performing distal radial access using ultrasound at the anatomical snuffbox. This technique has many potential benefits over conventional radial access by reducing symptomatic hand ischaemia as well as leading to fewer puncture-site complications and faster post-procedural haemostasis.
Continuing with the radial access mini focus, Jacques Doubell, Anton Doubell and colleagues discuss prolonged occlusion flow-mediated dilatation, a technique which can be used to dilate the radial artery prior to cannulation for coronary angiography in patients at risk for access failure – an approach which could result in fewer cannulation failures, fewer puncture attempts and a reduction in radial artery pulsation loss. This article is accompanied by an editorial by Sunil V. Rao and Zachary K. Wegermann.
We conclude our radial access mini focus with a short report by Dirk J. van der Heijden, Niels van Royen and colleagues comparing the rates of sheathless and conventional transradial access-induced vascular injury, with no advantage seen for the sheathless approach.
In interventions for valvular disease and heart failure, Alexander Jobs, Holger Thiele and colleagues compare general anaesthesia versus deep sedation in patients undergoing percutaneous edge-to-edge mitral valve repair. They conclude that either method is safe and feasible. The decision as to which one to use remains up to the preferences and experience of individual operators and centres. This article is accompanied by an editorial by G. Burkhard Mackensen and Richard Sheu.
Andreas Baumbach, Peter Andreka and colleagues look at an alternative approach to treating the calcification of the aortic valve leaflets caused by senile calcific aortic stenosis. The Leaflex device is the subject of this first-in-human study. It is an approach that could complement existing therapies but, while the device seemed feasible and could improve valve haemodynamics, these are early results and further research is needed.
And now, enough of an introduction, let’s turn the page and enter into the articles themselves.
Supplementary data
To read the full content of this article, please download the PDF.