Forty years after the first angioplasty procedure was carried out by Andreas Grüntzig and 15 years after the first TAVI performed by Alain Cribier, interventional cardiology has become a fully-fledged medical discipline and one that has undergone considerable mutations over the years.
Not only has TAVI become a major therapeutic strategy for symptomatic severe aortic stenosis, but it has also paved the way for percutaneous treatment of structural heart diseases ranging from atrial appendage closure to management of mitral and even tricuspid valvular conditions as well as obstructive hypertrophic cardiomyopathy.
In the setting of coronary artery disease, if medicine is an art, the novice interventional cardiologist should not only master his art from a technical viewpoint but he should also have a thorough knowledge of the respective indications of surgery and PCI gained through his own and his centre’s experience. He should also keep abreast of the latest enhancements in angioplasty equipment, imaging technology, antithrombotic treatment and dyslipidaemia management. Given the ever-expanding wealth of data available in the literature he should be able to take a critical look at recently published trial outcomes whilst considering any innovative concept with an open mind and be alert to how knowledge may evolve in sometimes unexpected ways.
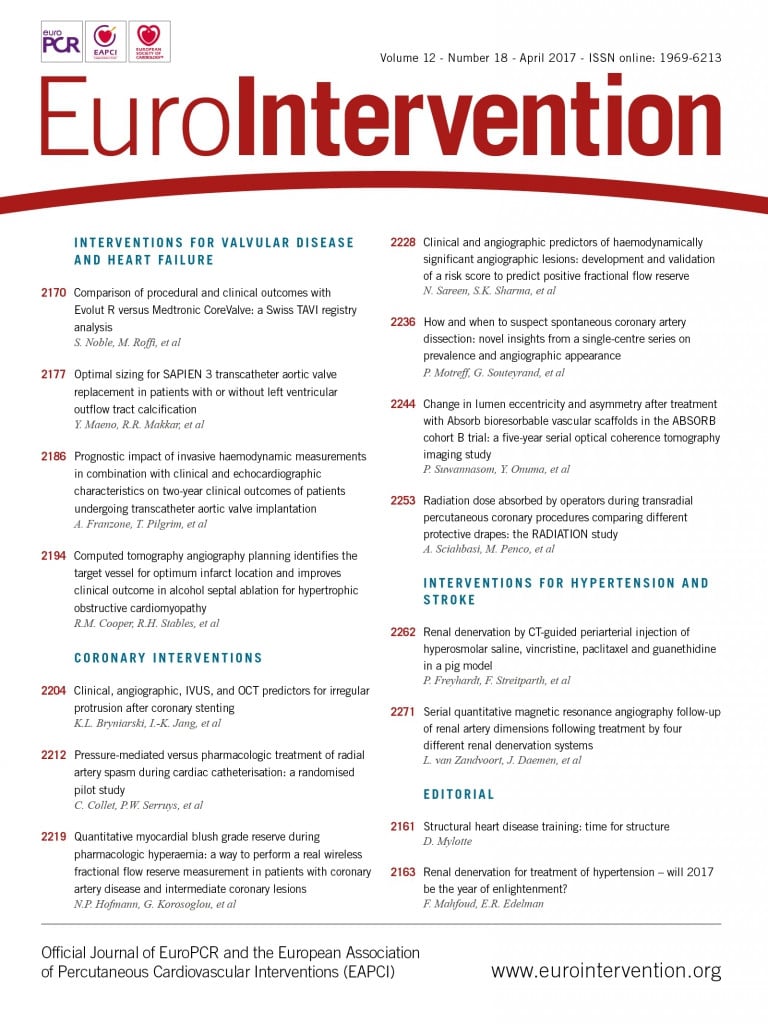
These principles are perfectly illustrated by three papers published in the coronary section of EuroIntervention’s latest issue. They are thought-provoking as well as being a source of knowledge enhancement whilst presenting practical implications and reflecting the remarkable open-mindedness of their authors.
These three articles are, namely, the study by Bryniarski et al (Clinical, angiographic, IVUS, and OCT predictors for irregular protrusion after coronary stenting)1, the study by Collet et al (Pressure-mediated versus pharmacologic treatment of radial artery spasm during cardiac catheterisation: a randomised pilot study)2, and the result of a long-term analysis by Motreff et al (How and when to suspect spontaneous coronary artery dissection: novel insights from a single-centre series on prevalence and angiographic appearance)3.
Irregular protrusions (protrusion of material with an irregular surface into the lumen of the vessel between struts identified by OCT) after coronary stenting had been shown to be associated with a higher midterm MACE, around 150%4, but predictors had yet to be identified. Bryniarski et al analysed the predictive factors in a large cohort of 786 all-comer patients undergoing PCI and OCT assessment. Irregular protrusion was observed in slightly more than half of the patients (58%). By multivariate analysis, predictors were found to be a higher rate of low-density lipoprotein (LDL) cholesterol, a higher volume of atheroma on IVUS examination, a greater lipid content, a stronger prevalence of thrombus revealed by OCT as well as the use of a longer stent. These data show that the underlying mechanism of irregular protrusion cannot be attributed to a single cause. The rate of LDL cholesterol prior to PCI seems to play a crucial role, given that it is related to the volume of atheroma. In the setting of acute coronary syndromes (ACS) with thrombotic lesions, the implementation of thrombectomy prior to stenting, or even deferred stenting in order to allow reduction of the thrombus burden, may improve acute and long-term outcomes. Finally, in patients with stable angina, stenting of long segments should be carried out according to the distal and not the proximal reference diameter in order to avoid overstretching of the distal stented segment5.
The article by Collet et al2 addresses innovation and the need for pragmatism in interventional cardiology. The authors focus on radial artery spasm, which remains an important issue given that the radial approach has become the standard route despite a non-negligible learning curve6. Although spasm can be avoided in the vast majority of cases by appropriate patient preparation in a quiet environment, accurate single puncture and effective antispastic medication using calcic inhibitors7, there is still room for improvement. Collet et al randomly compared two treatment modalities for radial spasm in patients who did not receive antispastic medication, using either a curative combination of verapamil and nitroglycerine, or an injection of saline in the introducer sheath (10 ml in 1 second, with a maximum pressure of 400 psi). The study clearly shows that pressure-mediated treatment of radial artery spasm is superior to pharmacological treatment, as evidenced by a diameter gain of 0.85±0.46 mm vs. 0.03±0.24 mm, p<0.001.
Finally, the excellent article by Motreff et al3 reinforces the message that future interventional cardiologists should keep an open mind when confronted with poorly understood or mysterious images. Indeed, at least once in our career, most of us have misdiagnosed a spontaneous coronary haematoma in the setting of ACS in a female patient with few or no risk factors and atypical angiographic lesions (1/3 of women admitted for ACS in the study by Motreff). Spontaneous coronary dissections are akin to spontaneous coronary haematoma, dissection being a resolution mode of haematoma. While dissection can be easily diagnosed on angiographic images, the presence of haematoma is not so easily detected. Therefore, Motreff et al deserve high praise for their prospective, long-term analysis evidencing the signs of haematoma by angiography with OCT guidance, namely: 1) absence of atheroma on other coronary arteries, 2) radiolucent flap(s) generating at least two lumens, 3) contrast dye staining of the arterial wall, 4) starting and/or ending of the angiographic ambiguity on a side branch, 5) long narrowing of lumen diameter: smooth and linear, or stenoses of varying severity (from mild stenosis to occlusion, often distal) mimicking a “stick insect” or “radish” aspect. Mastery of these angiographic signs is essential given that the management of spontaneous haematoma is practically the opposite of that of ACS.
Minimalistic observational treatment with single antiplatelet agents is the currently recommended strategy and PCI should only be performed as a last resort option for patients in whom medical treatment has failed8.
These three papers reflect the complexity as well as the level of technical and scientific commitment of interventional cardiologists who should build on their past experience whilst looking to the future with open-mindedness and relentless curiosity. An optimal fellowship training programme with sufficient procedural volume in the treatment of coronary artery disease is therefore warranted so that future cardiologists may acquire hands-on solo experience in transradial procedures, acute MI cases, bifurcation lesions, left main cases, imaging, rotablator and other complex PCI settings.
Conflict of interest statement
The author has no conflicts of interest to declare.