Bioprosthetic prostheses are increasingly used for surgical aortic valve replacement (SAVR) in patients with stenotic aortic valves1, due to the avoidance of oral anticoagulation therapy (OAC) – particularly in patients with an increased bleeding risk. In addition, transcatheter aortic valve implantation (TAVI) has, during the last decade, rapidly expanded as an alternative to SAVR in patients at increased surgical risk. However, bioprosthetic heart valves have limited longevity and a constant risk of structural valve deterioration (SVD), including valve thrombosis. Despite the fact that crimping of the heart valve prosthesis into a delivery system may cause damage to the leaflet tissue, symptomatic valve thrombosis with increased transvalvular gradient and symptoms is relatively rare after TAVI. It has been reported that it occurs in 0.6-2.8% of patients, and that temporary OAC may resolve both thrombosis, elevated gradient and clinical symptoms2,3.
More recently, however, four-dimensional volume-rendered computed tomography (4DCT) has revealed the presence of subclinical leaflet thrombosis as a more common finding after both TAVI and SAVR4-7. Valve leaflet thickening and reduced leaflet motion have, with reference to their CT appearance, been referred to as hypoattenuating leaflet thickening (HALT) and the more severe hypoattenuation affecting motion (HAM), respectively. Observations suggest that HALT and HAM are two stages of the same phenomenon, with leaflet thickening affecting leaflet motion at a more advanced stage. Uncontrolled data indicate that HAM may be more common after TAVR (13%) than after SAVR (4%)7, but it must be kept in mind that the two patient groups are different with regard to age, comorbidity, medical therapy, etc. Despite the fact that HAM may be associated with a small increase in transvalvular gradient, this is within the normal range in bioprosthetic aortic valves and will not permit detection of HAM on transthoracic echocardiography7.
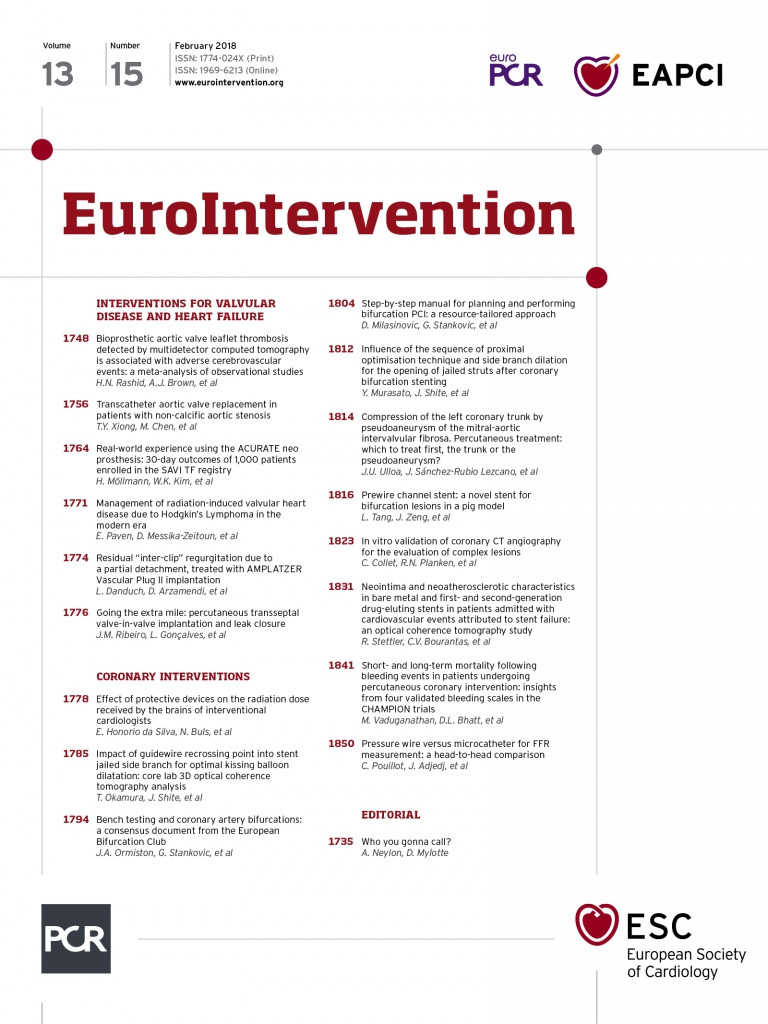
It is speculated whether subclinical leaflet thrombosis will impact on the post-procedural outcome, e.g., increase the risk of stroke/TIA, as well as lead to early SVD. In the current issue of EuroIntervention, Rashid and colleagues report the outcomes of a meta-analysis including six studies on subclinical leaflet thrombosis in bioprosthetic aortic valves in order to assess any association with stroke and TIA8.
They conclude that leaflet thrombosis is associated with a significantly increased risk of cerebrovascular events. However, these findings must be interpreted with caution. Firstly, only four of the six studies provide data on cerebrovascular events. Secondly, the largest of these studies is the publication by Chakravarty et al7, which is weighted 76% in the meta-analysis. Thirdly, a major limitation of the individual studies as well as the meta-analysis is that there is an (often very long) temporal separation between the clinical event and the CT scan. Since it has been suggested that leaflet thrombosis may resolve spontaneously9, it may be difficult to conclude that stroke, TIA or other event is caused by subclinical leaflet thrombosis detected several months later. In fact, it may potentially be a patient-specific risk for both temporary leaflet thrombosis and cerebrovascular events. Thus, prospective clinical studies are warranted in order to link subclinical leaflet thrombosis with cerebrovascular events. Similarly, there are no data for the potentially negative impact of subclinical leaflet thrombosis on the durability of bioprosthetic aortic valves. However, it has been reported that absence of anticoagulation is an independent risk factor for SVD after TAVI, but without exploring the potential impact of leaflet thrombosis10.
Although risk factors for subclinical leaflet thrombosis are not clearly identified, regional stent frame underexpansion has been associated with an increased risk of leaflet thickening, and post-dilatation of self-expanding transcatheter heart valves as well as a supra-annular valve position seemed to reduce the occurrence of this phenomenon11. Furthermore, OAC with either vitamin-K antagonist (VKA) or novel oral anticoagulants (NOAC) seems to protect against the phenomenon, whereas neither single nor dual antiplatelet therapy (APT) has the same effect7. When present, the subclinical leaflet thrombosis may be resolved by VKA or NOAC5-7. However, due to the temporal dynamic pattern of the evolution of these phenomena, where subclinical leaflet thrombosis may develop or regress early or late after valve replacement despite no change in antithrombotic regime9, short-term anticoagulation may not necessarily protect against leaflet thrombosis at a later stage. These preliminary findings complicate recommendations regarding optimal antithrombotic therapy after TAVI or SAVR, since the patient only seems to be protected against leaflet thrombosis while on anticoagulation therapy, and lifelong treatment is associated with an increased bleeding risk.
So how should the community act at the present time with regard to subclinical leaflet thrombosis? It has been suggested not to change clinical practice with regard to the choice of transcatheter or surgical bioprosthetic valve. TAVI has become an important and lifesaving treatment option for patients with aortic stenosis, and the current uncontrolled data do not justify a limitation in a potential expansion of this therapy. Similarly, there is no case for a change in antithrombotic therapy in favour of anticoagulation at the cost of a higher bleeding rate. Instead, it is recommended to await the ongoing randomised clinical trials between TAVI and SAVR, where a subset of the patients will undergo 4DCT (NCT02675114, NCT02701283), as well as the trial between different antithrombotic regimes (ARTE NCT01559298, AUREA NCT01642134, POPULAR-TAVI NCT02247128, GALILEO NCT02556203, ATLANTIS NCT02664649, AVATAR NCT02735902).
Routine 4DCT to check for subclinical leaflet thrombosis should not be performed outside clinical studies, since this will expose the patients to radiation and contrast without any evidence that a positive silent finding is an indication for anticoagulation therapy. However, patients who after TAVI or SAVR present with a new stroke/TIA or an increased transvalvular gradient may be considered for 4DCT and anticoagulation in case of a leaflet thrombosis.
Conflict of interest statement
L. Søndergaard has received consultancy fees and institutional research grants from Abbott, Boston Scientific, Edwards Lifesciences, Medtronic, and Symetis.