In this issue of EuroIntervention, a comparison of the outcomes of transcatheter aortic valve implantation (TAVI) performed by a “minimalist” versus a “complete Heart Team” is being published1.
The authors, Droppa et al, describe their consecutive experience and outcomes using two completely different team set-ups. All procedures were performed under local anaesthesia, patients were treated between February 2014 and May 2017, and the analysis was performed retrospectively. The change in practice occurred due to a newly established German regulation which defined the Heart Team in accordance with guideline recommendations. The authors mention that they were “forced” to establish a true Heart Team. When looking at the patient numbers included in this analysis, 292 patients were treated during the 18-month period from February 2014 to July 2015 by the “minimalist team” (=16 patients per month), whereas, later on, 238 patients were treated in the 22-month period from August 2015 to May 2017 by the full Heart Team (=11 patients per month). This decrease in the monthly number of patients is in complete contrast to the countrywide trend of increasing numbers of TAVI procedures and several questions therefore arise. Was there any difference in screening when the true Heart Team was in place? Was there any selection of patients who were included in this analysis?
The overall outcomes of TAVI procedures are very good with low mortality and morbidity, as is also shown in this manuscript. However, a residual risk of severe complications remains during every procedure and there are no predictors indicating when a complication may occur2. Therefore, a routine Heart Team should be prepared to provide optimal care for all patients. Withholding potential therapy, especially complete Heart Team care which is indicated in the guidelines, may raise some ethical questions. The current guidelines clearly underline that “Aortic valve interventions should only be performed in centres with both departments of cardiology and cardiac surgery on-site and with structured collaboration between the two, including a Heart Team (heart valve centres)”3. With the suggested set-up in the present manuscript, a structured collaboration between cardiologists and cardiac surgeons cannot be reached. It would be interesting to know whether patients were aware of the situation, i.e., that full support by anaesthesiologists and cardiac surgeons was not present. Most interestingly, such suggestions are being raised only in Germany, whereas in all other countries there is no discussion about performing TAVI by a Heart Team.
The presented set-up is called a “minimalist Heart Team”, but is it a Heart Team at all? Honestly, we believe it is not. Imagine an aircraft where the flight captain is being called to the cockpit for an emergency. He will be back to his seat within seconds. He will be able to perform all the required tasks immediately, because he is highly involved in the flight, he was definitively present at the previous team briefings, he was present during the starting of the aircraft, etc. The suggested “minimalist Heart Team” is completely different: important parts of the team, cardiac surgery and anaesthesiology, are not involved. They are just to be called on when there is an emergency, without being involved in the case, assuming that there was no briefing, no joint start of the procedure, no presence during the procedure, etc. The expectation that such a set-up leads to comparable outcomes is not realistic. In a small series of selected patients, as in the present manuscript, this may be comparable, but in an overall all-comers setting it will not be. A true Heart Team consists of different specialities, namely cardiologists, cardiac surgeons and cardiac anaesthesiologists.
The simple suggestion of a structured minimalist Heart Team would be the best way forward: two physicians perform the procedures, one cardiologist and one cardiac surgeon, instead of two cardiologists. One anaesthesiologist should be present who takes care of the echo instead of one echo cardiologist. Two nurses should be present, one catheterisation lab nurse and one operating room (OR) nurse instead of two catheterisation lab nurses only. The overall number of physicians and nurses of such a structured minimalist Heart Team is the same as suggested by the authors, but guidelines and regulations are being followed and the patient can expect maximal safety (Table 1, column C).
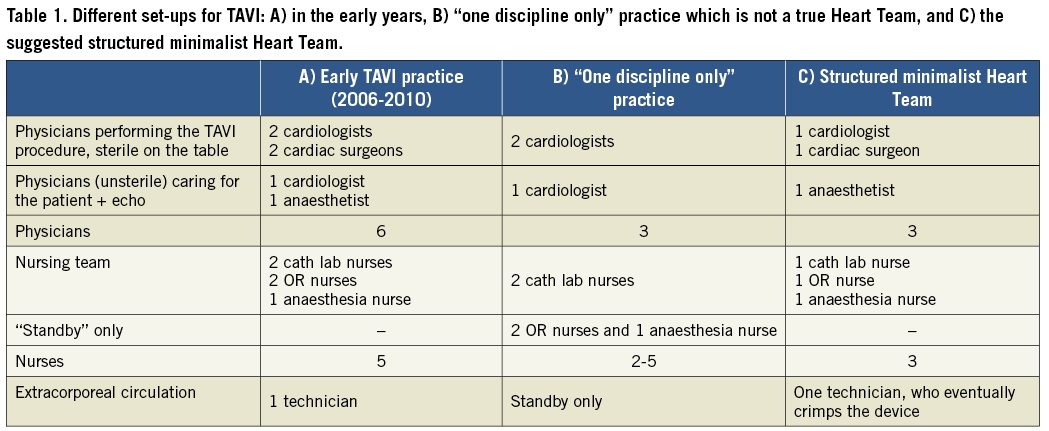
The suggested structured minimalist Heart Team (Table 1, column C) offers multiple advantages:
– full team integration;
– adherence to current guidelines;
– optimal safety and optimised therapy;
– TAVI performance independent of individual (personal) interests;
– future collaboration.
Such a structured minimalist Heart Team, consisting of the joint team work of one cardiologist, one cardiac surgeon and one anaesthesiologist, requires dedicated team members. Cardiac surgeons and anaesthesiologists should be highly interested in collaboration and in performing TAVIs together. It requires communication, training and willingness to work together. In the end, such cooperation will be fruitful for all partners, it will be of maximal benefit for the patient, and it will be a true Heart Team. We should all bear in mind that TAVI procedures are in-hospital procedures and anything physicians do in a hospital should be team work.
Once established, a structured minimalist Heart Team will be quite rewarding. It paves the way for an even broader cooperation in all of the different fields of medical practice treating heart disease. For the future, a joint “physician interventionalist” who has received basic training in either cardiology or cardiac surgery and then in addition follows a curriculum in structural heart interventions should be established. This joint effort will be of maximal benefit for patients who require TAVI, during preprocedural screening, when performing the procedures, and during postoperative care. The structured minimalist Heart Team with guideline-directed cooperation between cardiologists and cardiac surgeons will be the future.
Conflict of interest statement
The authors have no conflicts of interest to declare.