Introduction
Percutaneous coronary intervention (PCI) in bifurcation lesions remains complex in many respects. Part of the complexity relates to the variety of situations, definitions, treatment and outcomes which are related to this anatomical configuration. In order to develop a consensual view on the many aspects of coronary bifurcation lesions, the European Bifurcation Club (EBC) was created in 2005. The first EBC meeting took place in Bordeaux and some consensus emerged1.
Briefly, the participants agreed that: a) the Medina classification should be adopted2, b) with bare metal stents, a stepwise provisional T-stent strategy is the gold standard, c) with bare metal stents, deliberate double-stenting may be an inferior technique, d) with drug-eluting stents, the optimal strategy is under development and ongoing trials (Nordic and BBC1) will help to define it, e) after complex stenting, kissing balloon inflations should be routinely performed.
Several problems were still unsolved, however. Some of the debated issues as well as the previously adopted ideas were discussed, with respect to the recent clinical and technical developments, during the second EBC meeting which was held in Rome on September 29th to 30th, 2006. This manuscript highlights the discussions, disputes and consensus which emerged from this meeting.
Definitions
A simple description of the treated lesion, stenosis quantification and PCI technique is not straightforward. Following the first and second EBC meetings, a general consensus emerged and led to the publication of a paper which describes the classification of coronary artery bifurcation lesions and treatments3. Figure 1 describe the Medina classification (lesion description) and Figures 2 and 3 the MADS classification (treatment description) which are unanimously accepted by the EBC.
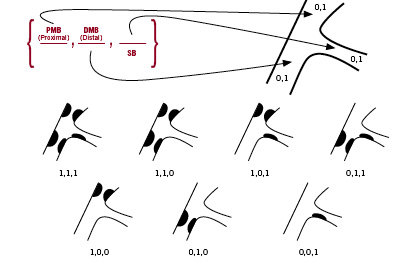
Figure 1. Description of the Medina classification of bifurcation lesions.
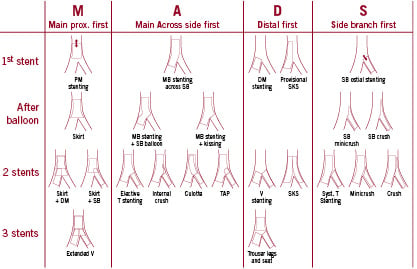
Figure 2. Description if the MADS classification of bifurcation treatment.
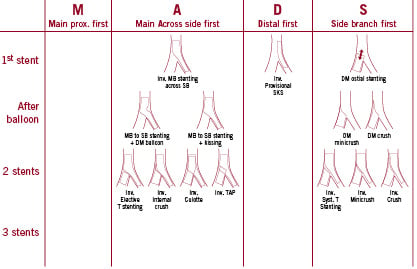
Figure 3. MADS classification of “inverted” techniques.
These classifications may need some refinements, however, and take into consideration the angle between the two branches, the lesion length, the observed/expected diameter, the TIMI flow, presence of calcification, plaque situation or eccentricity, ulceration, but all these aspects are hampered by the limitations of an accurate quantitative coronary angiography evaluation which is still operator dependent and thus subjective. Novel bifurcation software may solve some, but not all problems. A single analysis of the 3 vessels is made possible while considering the constant reference vessel diameter (RVD) relation between proximal vessel diameter (PVD), distal vessel diameter (DVD) and side branch diameter (SBD) such as PVD=0.678 x (DVD+SBD)4.
However, QCA is still limited at the level of carina which reference diameter is interpolated for the segment analysed and cannot be assessed in a single view most of the time.
Anatomopathology and physiopathology
Pathologic examination of coronary arteries reveals that the atherosclerotic plaques are located mainly along the inner side of the curved coronary arteries, close to the areas of minimum shear stress. Regions exposed to the non-uniform shear stresses develop early atherosclerotic lesions while areas exposed to uniform shear stresses are protected5-12. Consequently, atherosclerotic plaque usually develops opposite of the site branch13-16. Seen in this light, alterations in flow pattern may be critically important, not only for the comprehension of lesion geometry, but also when considering that the same mechanism favours intimal hyperplasia, and thus in-stent restenosis following stent implantation. Thus, in the setting of flow disturbances such as observed in bifurcation lesions, high restenosis rates are expected with bare metal stents, which could be offset by drug eluting stent placement.
Although there is a correlation between the stenosis severity of the side branch (SB) and its physiological significance following stent implantation in the main vessel (MV), Koo17 has shown that about 70% of ostial SB lesions following MV stenting are not functionally significant. In this very important study, no lesion with < 75% SB stenosis by QCA had a fractional flow reserve (FFR) < 0.75. Wide variations in FFRs were shown even in SB lesions with > 75% stenosis by QCA suggesting that in some cases “significant” side branch lesions after main branch stenting should not treated. On the opposite side, in this study, final kissing balloon inflation of physiologically SB stenosis (FFR < 0.75), was associated with excellent clinical outcome. Therefore, FFR assessment of SB ostial lesions after MV stenting or the use of a better angiographic cut-off value may be advocated before performing kissing balloon, and/or stenting of the SB.
Technique
One of the problem encountered in bifurcation stenting is plaque shift and carena shifting leading to SB stenosis and sometimes occlusion. There is therefore some arguments to predilate both main and side branch before stenting, at least for severely stenosed (> 95%) SB in order to minimise the potential for ischaemia and to facilitated subsequent SB dilatation and stenting. Although some believe that SB predilatation is not critical providing that a wire is already placed, there is a general consensus to predilate any ostial calcified or long SB lesion as well as when plaque burden in both branches is high with a big myocardial mass at risk. However, when the strategy is provisional SB stenting, SB predilatation can cause a SB dissection which may be associated with SB access difficulties through the stent strut. Therefore, in case of significant SB dissection after SB predilatation it could be preferable to switch to a different strategy and stent the SB first.
The systematic use of a jailed wire in the SB is also debated. Whenever possible the “Keep It Simple Swift and Safe” (KISSS) principle is recommended. However, the jailed wire technique modifies favourably the angle between both branches, is a good marker of SB and thus helps you to perform a provisional SB stenting approach. It should always be considered in the more complex anatomy.
Final kissing balloon has been recommended to optimise stent apposition, correct stent deformation or distortion and improve side branch access. However, there is no consensus to recommend final kissing balloon in all bifurcation PCI. In addition, in the current era of drug eluting stents, final kissing balloon does not seem to be an essential factor for securing late clinical success and there are no randomised studies which have addressed specifically this technical issue. Therefore, the common sense is to recommend final kissing balloon for the complex lesions (1,1,1 or 1,0,1 or 0,1,1) or procedures (2 stents or more).
In most bifurcation lesions, one stent is the treatment of choice. In a “true” bifurcation lesion (Medina classification 1,1,1; 1,0,1 or 0,1,1), the strategy of elective implantation of 2 stents may be considered, especially when the side branch lesion is longer that 2 or 3 mm18, but there are no consensus on which of the different two stent methods gives the best result on a long term basis. Even more, should we be performing complex strategy in all complex bifurcation lesions? The recent Nordic Bifurcation Study19 compared a simple stent strategy (stenting of the main vessel and optional treatment of SB) with a complex strategy (stenting both main vessel and SB). Results of this pivotal study support the simple strategy in most situations, but the overall conclusions may not be valid for specific subsets of lesions. More data are still to be collected to define which is the strategy best adapted for each of the different anatomic situations. The results of BBC 1 study which will be available this year will be very important to try to answer this very crucial question.
Stent thrombosis and restenosis rate
Stent thrombosis has emerged recently as a major drawback of DES implantation. Iakovou et al were the first to address the increased risk of late stent thrombosis following bifurcation stenting with DES20. Although it appears that bifurcation compared to non-bifurcation treatment with DES is associated with a higher stent thrombosis rate21,22, except in the recently published ARTS II sub-study23, there is no proven difference between rates of thrombosis after DES vs BMS treatment of bifurcation lesions. Nevertheless, post procedural stent thrombosis has been reported in 0 to 7.2% of cases after bifurcation stenting with DES (Figure 4).
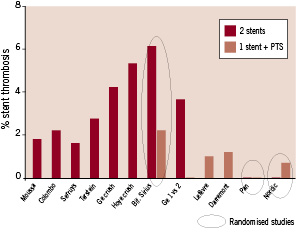
Figure 4. Occurrence of early and late (1 year) stent thrombosis in drug eluting stenting (DES) for bifurcation lesions. Data from references 19, 24-34.
If there is a trend toward a higher rate of stent thrombosis when using 2 stents, there is no clear demonstration that one stent technique is better than two stent methods, and explanations for increased thrombosis rates in bifurcation lesions are speculative. It is worth noting that treatment of bifurcation with DES is not an approved FDA indication and should therefore be considered with caution until more data are available on their long term safety. It was a consensus of this group that treatment of bifurcation with DES should be closely monitored in clinical trials or registries.
Low shear stress is associated with blood stagnation and therefore may participate in in-stent thrombosis as well as to neointimal proliferation. At least on theoretical grounds, great care should therefore be taken when designing dedicated stents for bifurcation or when performing complex two-stents techniques. Specifically, preliminary data suggests that high bifurcation angle (> 50°) has a negative impact on outcomes following crush, SKS or culotte techniques35. This may have very important consequence in left main stenting but more work is needed to decide on the clinical importance of coronary rheology.
Insights from ARTS II or REALITY studies and Research, T-search or Asian bifurcation registries support the use of DES which is associated with a low restenosis rate of one digit in the main branch and >10% only in the SB. Although outcomes appear similar with the different type of DES (sirolimus vs paclitaxel coated stent) and either using one or two-stents treatment strategies, more data are needed to confirm how might the DES matter.
Dedicated stents
The role of dedicated devices for the treatment of bifurcation lesion is still under investigation. There is a great hope that it will be the next step that will make bifurcation treatment easy for everybody especially for distal left main treatment. However, we are still waiting for the magic device. Preliminary results of the DES carena device (Devax™) assessed in the Axxess Plus study36 look promising. This dedicated stent appears safe and effective. Whether it represents an advance with respect to the current techniques needs to be evaluated.
Other DES dedicated devices are under development: The SideKick™ stent delivery system and the Stentys™ bifurcation stent are promising techniques allowing excellent SB access, the former being soon assessed in randomised study. The Capella™ sideguard ostium protection device and the Tryton™ side branch stent aim to optimise the SB coverage in combination with a stent placed in the main vessel. First-in-man trials are ongoing with the Capella™ and Tryton™ devices.
Left main
Whether distal left main stenosis has to be treated like any bifurcation lesion is debated37. Most participants would consider the same stenting PCI approach as for any bifurcation lesion, bearing in mind that there are three segments to treat, the reference diameter is large, the “SB” is significant with T shape angle and the coronary ostium should not be missed. In addition, stent thrombosis is not allowed. Accordingly, most procedures can be performed using the provisional SB T-stenting approach, with the need for additional SB stenting in 20 to 40% and final kissing balloon in all cases. Systematic use of two stents techniques may not be advocated because they are probably associated with higher risk of reintervention and stent thrombosis. Results of ongoing registries and randomised trials, such as SYNTAX are awaited to better define the strategy and indications of PCI on unprotected left main bifurcation who should be performed electively by experienced interventional operators in high volume institutions PCI and in patients not eligible for surgery.
Conclusions
Bifurcation lesions remain a challenging problem for PCI. Part of the complexity relates to the number of anatomic situations, the variety of interventional approaches, the worries over late outcomes and the limitations in anatomic as well as physiologic assessments. There are still many issues to solve and to debate. However, during this two day meeting some progress was made in the search for a standard approach.
WHAT WE ALL AGREE:
– The MEDINA classification of coronary bifurcation lesion and the MADS classification for treatment techniques should be adopted.
– QCA software needs to be standardised, with appropriate algorithms allowing multiple segment of interest analysis.
– With BMS, as well as with DES, a stepwise provisional T-stenting strategy is the best.
– Deliberate double stenting is an inferior technique.
– SB predilatation is recommended if calcified lesion or long lesion.
– Jailed wire is strongly recommended in complex lesions.
– After complex stenting (for complex lesions), kissing balloon inflations should be routinely performed.
WHAT IS STILL DEBATED:
– A validated software for QCA of bifurcations is still being waited for.
– An accurate evaluation of the functional significance of ostial SB stenosis is necessary.
– Should we do systematic kissing balloon inflation?
– Are DES really more thrombogenic? If yes, how to reduce the risk?
– What is the future of dedicated bifurcation devices?
– The optimal strategy for the treatment of distal left main bifurcation is under development, clinical trials and registries will help to define it.
– Solutions of the many problems dealing with bifurcation lesions depend on the collection of a large clinical experience. Therefore, the decision was taken at the end of this conference to create a specific e-CRF that would allow the collection of thousands of coronary bifurcation procedures and outcomes. With the use of this tool, we hope to be able to solve some of the remaining issues and to further expand our knowledge on one of the most debated issues of interventional cardiology.

