Introduction
Stenosis of the aortic valve is the most common valvular lesion affecting the adult population. Its incidence increases, as the population grows older1,2. Asymptomatic patients have an excellent prognosis. Yet, in case of symptoms such as angina pectoris, dyspnoea or dizziness the prognosis is poor. This is especially true when surgical treatment cannot be performed. In such instances, the annual mortality amounts to approximately 25%3. To meet this problem, percutaneous balloon valvuloplasty has been introduced in the mid-1980s but abandoned because of lack of efficacy and risks4. Less invasive surgical procedures are being explored and recently percutaneous valve replacement has entered the clinical field4-7. The technique, treatment and experience are still in its infancy but hold firm promise for a vast number of patients who are not referred, or cannot undergo, surgery. In accordance with earlier data from the European Heart Survey on valvular heart disease, it is estimated that the latter is true for approximately 30% of the patients with aortic stenosis1,8.
The present report describes the medical history and treatment of an elderly patient with severe aortic stenosis and heart failure who was declined for surgery in two institutions. She successfully underwent a percutaneous implantation of a porcine valve mounted in a self-expandable nitinol stent.
Report
A 77-year-old woman was referred to the outpatient clinic because of a severe aortic stenosis for which she was declined surgical valve replacement because of severe calcification of the ascending aorta and aortic arch. She had no previous medical history or co-morbid conditions. Coronary angiogram performed elsewhere, revealed absence of significant coronary artery disease.
When she was first seen at the outpatient clinic, there were symptoms of shortness of breath at rest. Clinically she was in overt left and right heart failure with rales and lower limb and sacral oedema. The blood pressure was 110/80 mmHg. At variance with a previous ECG, the current ECG revealed atrial fibrillation with a ventricular response of approximately 70 beats/minute.
She was admitted and unfractionated heparin and furosemide by means of a continuous infusion were initiated with the objective to perform valve dilatation and eventually percutaneous valve replacement in case of sufficient recovery. The administration of furosemide resulted in a weight loss of 17kg (form 88 to 71 kg) in a time span of 4 weeks. The dose of furosemide was regularly adjusted because of transient increases in serum creatinine.
Echocardiography revealed a normal sized left ventricle but with an impaired systolic function, calcified aortic stenosis (peak gradient 112 mmHg) in combination with mild to moderate aortic and mitral regurgitation. On MRI, the diameter of the aortic annulus was 23 mm. Also, thrombus in the left atrium and appendage was suspected.
On the basis of these findings balloon valvuloplasty with a 23 mm balloon was performed (Figure 1).
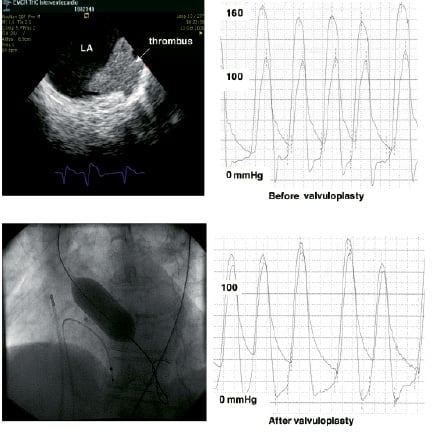
Figure 1. Pressure recordings before and after balloon valvuloplasty, balloon dilatation and coronary thrombus in left atrium (LA) and appendage visualised by intracardiac echo.
After three inflations the peak-to-peak gradient was reduced from 43 to 7 mmHg. The procedure was performed under the guidance of intracardiac echo (Acunav, Siemens, Germany), which confirmed the presence of thrombus in the appendage of the left atrium that extended along its wall (Figure 1). After valvuloplasty, there was a significant symptomatic and clinical improvement despite the presence of severe aortic insufficiency on echo.
Percutaneous aortic valve replacement with a 23 mm CoreValve (Figure 2) using femoro-femoral cardiac assistance was planned.

Figure 2. The CoreValve stented valve consists of a self-expandable nitinol stent in which a trileaflet valve is mounted. The nitinol frame has a diamond cell design with different strut lengths and widths to accommodate expansion to a non-uniform cylindrical shape. The lower or most distal part has a high radial force to push aside the native aortic leaflets and preventing recoil. The middle part is constrained to avoid interference with flow through the coronary ostia and hosts the tissue valve. The upper or proximal part implants itself on the ascending aorta, assuring anchoring and alignment of the implant. The valve is made of single layer of porcine pericardium constructed in a tri-leaflet configuration, which are attached to a scalloped skirt (also made of a single layer of porcine pericardium) using PTFE sutures. The valve is sutured to the nitinol frame with 5.0 PTFE sutures. The stented valve is crimped onto a 21.0 Fr delivery catheter covered by a protective sheath holding the prosthesis in a collapsed position.
Since it concerns an investigational treatment for which there was no clinical protocol yet, permission for compassionate use was asked and granted by the medical ethical committee of our institution and the Inspection of Health Care, The Hague, The Netherlands.
The implantation was performed under general anaesthesia. A 4 Fr pigtail was advanced via the left radial artery into the ascending aorta to allow pressure recordings and angiography for proper valve positioning and assessment of the final result.
This was followed by surgical cut down of both femoral arteries and veins for femoro-femoral cardiac and circulatory support on one side and insertion of the intracardiac echography and implantation of the stented valve through the other. After crossing the aortic valve and placement of an extra support guide wire, the stented valve was advanced through the aortic arch up to the ascending aorta. Extracorporal circulation was then started to allow precise positioning and expansion of the prosthesis at the aortic annulus (Figure 3).
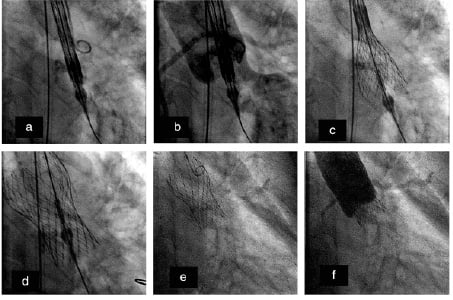
Figure 3 a & b. Positioning and deployment of the stented valve. The stented valve is carefully positioned in order to assure coronary flow and mitral function (a-b). The protective sheath is subsequently retracted allowing the full expansion of the stent and valve (c-d). The delivery catheter is then retrieved (e). Aortography directly after implantation of the stented valve. There is no aortic regurgitation and the coronary arteries can be discerned revealing unimpeded flow through the ostia (f).
This was performed under fluoroscopic control, angiography and intracardiac echo. After expansion, aortography was repeated which revealed absence of aortic regurgitation –confirmed by echography– and both coronary arteries were visible indicating unimpeded antegrade flow. All catheters were removed and protamine was administered.
After implantation, she was treated with unfractionated heparin that was replaced by acenocoumarol in combination with acetyl salicylic acid and clopidogrel for 6 months. Except for a delayed wound healing, that prolonged the hospital stay, the further course was uneventful. The patient felt well and there were no symptoms or signs suggestive of heart failure. Echocardiography only disclosed a minimal aortic insufficiency, which was most likely due to a small paravalvular leak.
Discussion
A percutaneous replacement of an aortic valve in a patient who could not undergo surgical valve replacement is reported. This is the first patient who is treated as such in the Netherlands. It concerns an investigational treatment that can only be performed in the framework of a scientific protocol. Since no protocol was submitted, permission for compassionate use was asked and granted by the authorities.
A strategy of percutaneous valve replacement was adopted since correction of the pressure load on the left ventricle in the absence of other co-morbid conditions and option for open-heart surgery was the only way to beneficially affect her prognosis. Balloon valvuloplasty has a temporary symptomatic effect and a strategy of repeated valvuloplasty suggested by some was not considered an attractive alternative. Notwithstanding the astonishing biomedical engineering aspects of this novel technology and treatment, it is at this moment not an alternative for open-heart surgery for patients at high risk of perioperative complications. To achieve this, carefully conducted prospective registries must obtain sufficient and solid clinical data on safety and efficacy9.
With respect to safety, at the time of the treatment decision in this patient, only fourteen patients worldwide had been treated with the present stented valve. Four of these patients died in the perioperative period. One death was related to prolonged lower limb ischaemia, one due to a left ventricular perforation due to the guide-wire and two died as a result of multi-organ failure in relation with prolonged thrombocytopenia in the postoperative period. The exact cause of the latter has not been elucidated, yet it may be related to platelet consumption induced either by the femoral-femoral support or the stented valve. This was no longer observed after the iniation of acetyl salicylic acid in combination with cloplidogrel prior to the implantation.
Obviously, death may also be patient related since so far only patients who could not be operated or were considered too high a risk for surgery were treated. At the time of this writing, 22 patients have been treated worldwide with this stented valve. No patient has died other than the four patients mentioned above. Of note, the design of the stent frame is such that after implantation flow through the ostia of the coronary arteries is not impeded and the space between the stent struts is large enough to allow selective catheterisation of the coronaries.
With respect to efficacy, valve function and durability of the stented valve have extensively been tested in a mock circulatory system under pulsatile flow. Yet, stented valves implanted in humans are subjected to different mechanical forces and environment that cannot be mimicked by in-vitro tests. With respect to the first, hypertension should be considered, but also the alignment of the valve in the ascending aorta. It is conceivable that the distribution of the mechanical forces differs between a valve that is perfectly aligned with the axis of the ascending aorta and one that is not. With respect to environment, surgically implanted homografts fare less well in patients with glucose, calcium and renal disorders.
Technology will evolve. Among others, the size of the delivery catheter will reduce. The original size was 25 Fr and currently is 21 Fr and an 18 Fr system is being developed. Hopefully further miniaturisation will occur reducing the surgical trauma and enhancing safety and feasibility. A truly percutaneous approach is foreseen that allows more patients to benefit from this treatment. It is also conceivable that further reduction in size of materials may obviate the need for cardiac and circulatory assistance. As long this is not a reality, one may consider the use of cardiac assist systems obviating the need of surgical cut down for placement of the cannulae such as the Tandem Heart. This was not possible in the present patient due to the presence of thrombus in the left atrium. The Tandem Heart is based upon the use of oxygenated blood that is drained from the left atrium via a cannula that is inserted via the right atrium and reinjected into the arterial system via the iliac artery. It has been used in high risk angioplasty and was used during the implantation of a CoreValve stented valve in a porcine model, which was part of an extensive preparation programme prior to the treatment of the present patient10. Also, advances in bio- and tissue engineering may lead to changes in stent and valve design and composition leading to further down sizing.
Optimal function and durability requires optimal attachment of the valve into the stent, preservation of the function of the valve and stent after compression and re-expansion9. Biological valves appear to be the most suited for this purpose but synthetic polymer-based material may provide an alternative provided haemo- and biocompatibility is guaranteed. Tissue engineered valves are being examined. They may consist of biodegradable scaffolds configured to the shape of the valve and seeded with cells proliferating and producing cellular and extracellular matrix9,11,12. Concern has been raised that coronary flow may be blocked by the native aortic leaflets that are immobilised by the stented valve against the coronary ostia. Techniques that captures and shelters the native valve leaflets or cut them away at the time of implantation are being examined13,14.
Similar to coronary balloon angioplasty, there is no doubt that we enter a new era of innovation that most likely will prove to be a sweeping and a far-reaching change in interventional cardiology that will benefit the patient. As we shape the future and think of expanding the envelope, we have to bear in mind and consider the history and results of the surgical repair of aortic stenosis and use them as a reference to define the standards for percutaneous valve repair and clinical studies.

