Time flies so fast, and it’s already the season to introduce a new issue dedicated to the PCR London Valves Course. In a field as young as structural interventional cardiology – or valvular interventional cardiology, as some prefer to call it – it is normal that there is something new to celebrate every year, and 2023 is no exception, marking twenty years since the first transcatheter edge-to-edge procedure. It’s evident to all that the progress of this technique hasn’t been as rapid and explosive as TAVI, which can be attributed to a variety of reasons, primarily stemming from the anatomical complexity and functional aspects of the mitral valve-left ventricle complex itself as compared to the relatively more straightforward elimination of aortic stenosis. Nevertheless, it’s a fact that the transcatheter edge-to-edge procedure has made significant strides in recent years, not only in terms of technology but also in terms of patient selection from a clinical and echocardiographic perspective.
As described by the Course Directors in their annual editorial (which follows), with international boundaries open again, this year more than ever, the Course can bring to the stage a panel capable of representing the global diversity of our speciality. As always, live cases will alternate in the main arena, this year recorded in London, Toulouse, Bordeaux, New York, and Bad Oeynhausen. These cases will include both transcatheter and surgical procedures, because the Course’s essence is to educate, not just on any single procedure, but on the treatment of valve pathologies, as defined by the Heart Team, in the way that’s best for the patient. And, this, of course, without losing sign of the diagnostics.
Once again, the usual three tracks covering the aortic, mitral, and tricuspid areas will be available. This year, there will also be a new “arena set-up” aimed at encouraging more fruitful and engaging interactions between the facilitators and active participants. In addition to these innovations, the Course will feature its classics: the simulation learning room, hands-on labs, the imaging learning centre, and the training village. And naturally, the Course Directors (with three new names added this year) have not forgotten about online participants, with numerous live-stream rooms on the Course platform and various content available on replay. There will be cases, abstract innovations, and late-breaking trials plus the second edition of the London Valves Fellows Course, where, for the first time, you can choose between the aortic or mitral pathways. In short, there’s something for everyone’s taste and discipline. And naturally, we at EuroIntervention aim to do our part by distributing a special issue of our Journal packed with content that we hope will support you in your daily practice right from the start.
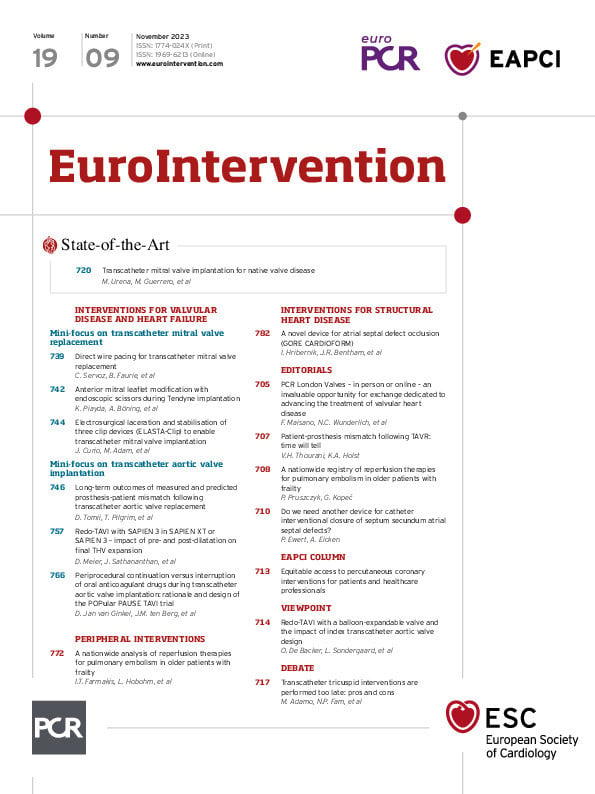
So, let’s have a peek inside this special issue, which, in keeping with the London Valves theme, brings you a wealth of articles on structural heart disease including two valve-centric mini-focuses: one on transcatheter mitral valve replacement and the second on transcatheter aortic valve implantation.
We begin with a thoughtful viewpoint on redo-TAVI with balloon-expandable valves by Ole De Backer, Lars Sondergaard and colleagues, followed by a EuroIntervention debate on the timing of transcatheter tricuspid valve interventions, which remains unresolved. To discuss this, we have brought together four practitioners who all agree that early identification of tricuspid regurgitation is essential as many patients remain asymptomatic. However, Marianna Adamo and Crina Ioana Radulescu set out their belief that there are currently no demonstrated benefits for late transcatheter tricuspid valve interventions, whereas Neil P. Fam and Shahrukh N. Bakar argue that current evidence supports close follow-up and medical management rather than immediate intervention.
We then turn to the first mini-focus with a state-of-the-art paper on transcatheter mitral valve implantation for the treatment of native valve disease. Mitral regurgitation is prevalent throughout Europe, but nearly half of symptomatic patients are ineligible for or refuse surgical treatment, and the development of transcatheter mitral valves has not kept pace with its aortic cousin. Marina Urena, Mayra Guerrero and colleagues bring us an in-depth look at the current state of transcatheter mitral valve implantation, with an anatomical review of the mitral valve, as well as indications for treatment, interventional planning and strategies, current devices and their respective trials and the future of this treatment.
We continue with a research correspondence from Clément Servoz, Benjamin Faurie and colleagues on direct wire pacing. They report on the use of direct wire pacing in a series of patients undergoing transcatheter mitral valve replacement procedures, including mitral valve-in-valve, valve-in-ring and valve-in-mitral annular calcification. The authors found direct wire pacing to be as efficient as left ventricular pacing and that it has the potential to simplify transcatheter mitral valve replacement interventions.
The transcatheter mitral valve replacement mini-focus concludes with two flashlights on anterior mitral leaflet modification and the ELASTA-Clip technique.
Our second mini-focus on TAVI starts with Daijiro Tomii, Thomas Pilgrim and colleagues examining how measured and predicted effective orifice areas (EOA) may affect estimations of the frequency and severity of patient-prosthesis mismatch (PPM). By looking at the long-term clinical outcomes of patients stratified according to PPM, the authors found that predicted EOA is more likely than measured EOA to downgrade the severity of PPM, although there was no increased risk of death in PPM patients over mid-term follow-up, regardless of the definition of EOA. Vinod H. Thourani and Kimberly A. Holst contribute an editorial on this topic.
Next, David Meier, Janarthanan Sathananthan and colleagues evaluate the impact of pre- and post-dilatation on the expansion of balloon-expandable transcatheter heart valves after redo-transcatheter aortic valve implantation. After using SAPIEN 3 and SAPIEN XTs in eight different configurations, it was only when the SAPIEN 3 was implanted in another SAPIEN 3, with the use of pre- and post-dilatation, that full expansion was achieved. The authors also elaborate on the role of computed tomography in assessing expansion.
The TAVI mini-focus concludes with an article by Dirk Jan van Ginkel, Jurrien M. ten Berg and colleagues presenting the design and rationale for the POPular PAUSE TAVI trial, in which patients undergoing transcatheter aortic valve interventions are randomised to either periprocedural continuation or interruption of oral anticoagulants, testing their hypothesis that periprocedural continuation of oral anticoagulants is safe and may decrease thromboembolic events without an increase in bleeding complications at 30 days. Recruitment started in late 2020, and the trial will assess endpoints including mortality, stroke, vascular complications, bleeding, as well as quality of life post-intervention.
Switching for a while to peripheral interventions, Ioannis T. Farmakis, Lukas Hobohm and colleagues assess the safety of reperfusion therapies in elderly and frail patients with pulmonary embolism. Use of the classical reperfusion therapies – systemic thrombolysis and surgical embolectomy – in this population is low, as they can increase the risk of bleeding and perioperative complications. Catheter-directed therapies, such as catheter-directed thrombolysis and catheter-based thrombectomy, showed lower rates of bleeding and may be a safe alternative to classical reperfusion therapies for this patient population. This article is accompanied by an editorial by Piotr Pruszczyk and Grzegorz KopeÄ.
Returning to interventions for structural heart disease, we have a report on the GORE CARDIOFORM atrial septal defect Occluder by Ines Hribernik, James R. Bentham and colleagues. The authors report on the outcomes of device implantation in 4 UK centres and compare them to the similar-sized cohort treated with the same device in the US-based ASSURED trial. The technical success rates and the rates of serious adverse events were similar between the two studies. The notable absence of aortic erosion also helped the authors to conclude that the CARDIOFORM can be used to treat a wide variety of atrial septal defect morphologies and sizes. Peter Ewert and Andreas Eicken further discuss the design of the device in an accompanying editorial.
And now, on to the papers themselves.
Editorial
DOI:
PCR London Valves edition with a state-of-the-art on transcatheter mitral valve implantation for native valve disease; debating the timing of transcatheter tricuspid valve interventions; direct wire pacing for transcatheter mitral valve replacement; predicting patient-prosthesis mismatch following TAVI; pre- and post-dilatation in redo-TAVI; the POPular PAUSE TAVI trial; reperfusion therapies for pulmonary embolism; and more
You need to subscribe to download this file
×
If you are not yet a subscriber, please subscribe to download this file.
Download citations
×
Select a format