Have you ever been a patient yourself?
It can be a strange experience to be the recipient of care and be exposed to advice, consent, treatment decisions and even suggestions to participate in research. We are generally not used to thinking about our practice from a patient’s perspective, despite the fact that we all strive to provide the best care and achieve the “best outcomes”.
We measure and compare outcomes based on “hard” endpoints such as death, myocardial infarction and repeat intervention, mostly because they are easier to determine than subjective parameters of wellbeing and quality of life. What is it the informed patient really cares about? How can we improve patient experience and the benefits of our care towards an optimal quality of life? We must focus on the patients and start a dialogue to find out.
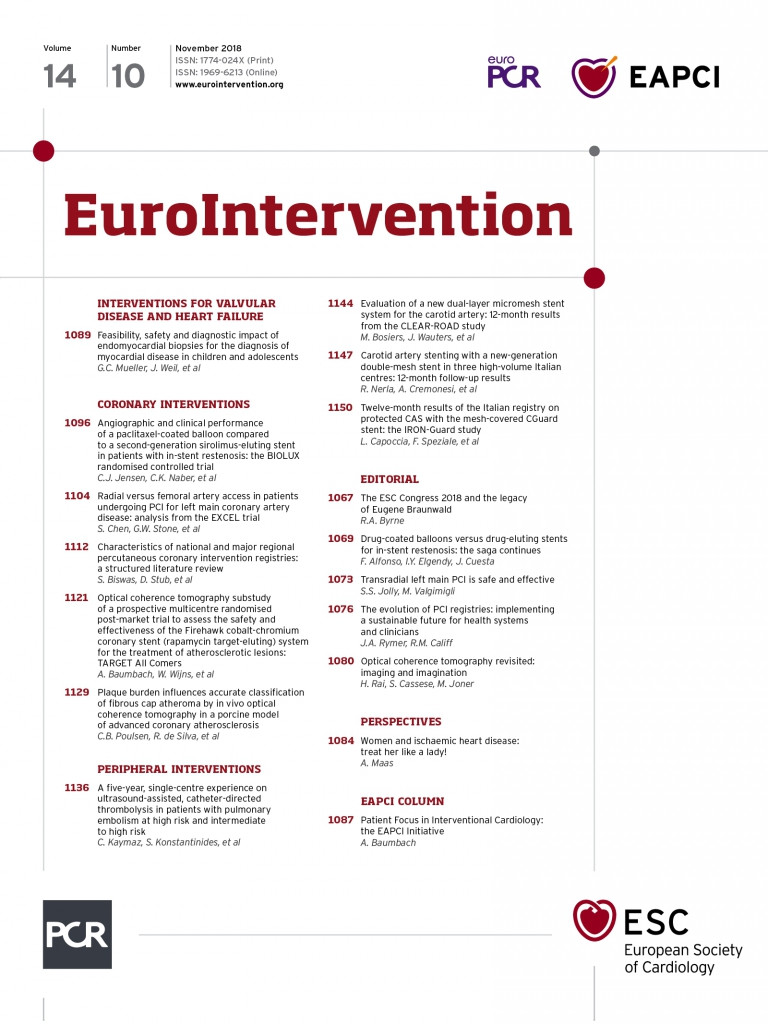
The EAPCI initiative Patient Focus in Interventional Cardiology has gained momentum this year. We have a new committee, co-chaired by Fina Mauri and Robert Byrne, from which we will see work dedicated to patient advocacy, disparity and patient engagement. This links in with the larger ESC patient initiative in cardiovascular care.
In a first meeting we brought together the leads of National Societies in Interventional Cardiology for the 2018 EAPCI Summit at the Heart House. The objectives were to find the best ways to create awareness of patient-related aspects of our care, identify barriers to optimal invasive cardiovascular treatments and to become the advocates for our patients and for best cardiovascular care… and it turned out to be not so easy.
First, whenever we think about patient-centred or focused care, each of us has rather different ideas. Some think we already provide best and extensive care (particularly in countries with seemingly unlimited resources), while others hesitate to engage with patients directly when it comes to discussions about their care, their expectations and also research. Some, on the other hand, feel we should include patients in all aspects of treatment planning, delivery, governance and research. Secondly, we find it difficult to identify pathways to engage with patients. Should we invite a dialogue? Ask them about gaps in treatment? Discuss outcomes? Invite patients to sit on trial steering committees and get involved in guidelines? Thirdly, we were mostly unaware of how other specialities and cardiac subspecialties have already initiated and embedded patient involvement in their field.
During the summit we developed an insight into existing initiatives, learned from the advanced field of oncology and what happens in subspecialties such as arrhythmia treatment and heart failure. We have now defined our first steps and, in the months to come, you will hear about patient-reported outcomes (PRO) in coronary intervention, patient-reported experience measures (PREM) following PCI, and an overhaul of the informed consent process using modern media support. More detailed proceedings of the summit will be made available soon.
The EAPCI mission is to “reduce the burden of cardiovascular disease through percutaneous cardiovascular interventions”. Engaging with the patients we treat (and might ourselves one day become) is an important step towards improving our care and will help us to fulfil our mission.