Abstract
Aims: Very few women become interventional cardiologists, although a substantial proportion of cardiologists and the majority of medical students are women. In accordance with the EAPCI Women Committee mission of attaining gender equality at the professional level, a worldwide survey was recently conducted aiming to understand better the motivations and the barriers for women in selecting interventional cardiology (IC) as a career path.
Methods and results: A total of 1,787 individuals (60.7% women) responded to the survey. Women compared to men were less frequently married (women vs. men, 57.0% vs. 79.8%, p<0.001) and more frequently childless (46.6% vs. 20.5%, p<0.002). The most prevalent reason for choosing IC was passion (83.3% vs. 76.1%, p=0.12), while those for not choosing were, sequentially, lack of opportunity (29.0% vs. 45.7%), radiation concerns (19.9% vs. 11.6%) and preference (16.2% vs. 29.5%), p<0.001. According to 652 men replying to why, in their opinion, women do not choose IC, on-calls and long working hours were the most frequent reasons (35.3%).
Conclusions: Several barriers preclude women from choosing IC, including lack of opportunity, concerns regarding radiation exposure and the prejudices of their male colleagues. This highlights the need to develop new strategies for future training, education, and support of women in order to choose IC.
Introduction
In the last three decades, a drastic decline in cardiac mortality and considerable improvements in quality of life for cardiac patients have been observed. This is substantially attributed to the increasing use of percutaneous coronary and structural interventions, as well as advanced contemporary pharmacotherapy. Due to an increasing ageing population, a growing proportion of individuals with obesity and diabetes mellitus, the expansion of the interventional cardiology field towards structural heart disease as well as to the rapid improvement in novel technologies, there is an incremental need for interventional cardiologists. Approximately 90% of interventional cardiologists are men. The small number of female interventional cardiologists contradicts the fact that throughout Europe the majority of medical students (nearly 60%) are women1,2. These observations and disparities have set the rationale for the establishment of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Women Committee with the aim of identifying determinants of the current gender-related disparities at the medical school-to-work transition, and of developing strategies for education, professional advancement and research in the field of interventional cardiology (IC). The Women Committee is a community of female interventional cardiologists within the EAPCI with the following objectives: to encourage female physicians to choose an IC career; to help women to achieve equal career opportunities to men; to increase awareness in the interventional and research community about gender-related disparities in diagnosis and treatment of cardiac patients; to support the systematic enrolment of women in clinical trials; to ensure the consideration of women in all aspects of scientific literature; to develop educational programmes on gender-based issues in interventional cardiology.
In accordance with the EAPCI Women Committee mission of attaining gender equality at the professional level, a survey was recently conducted by the EAPCI Women Committee with the aim of understanding better the motivations and the barriers for women in choosing IC as their subspecialty. The results of this survey are presented here.
Methods
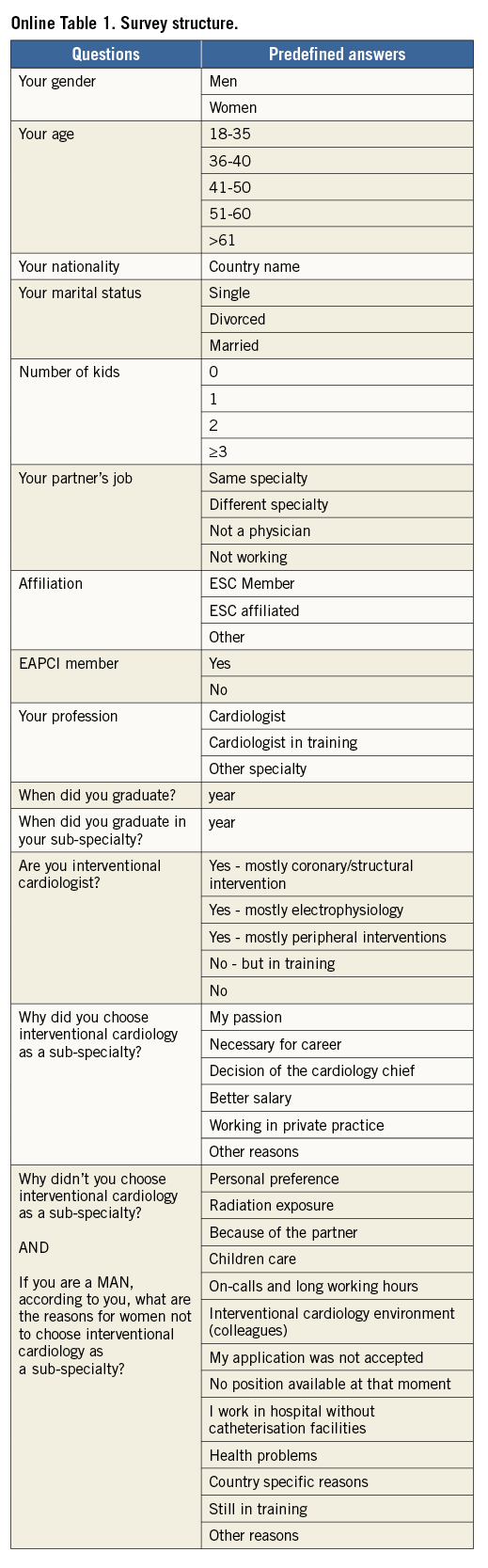
The European Society of Cardiology database comprises 293,932 individuals, with 48,443 who had expressed an interest in IC. The EAPCI Women survey was sent to those individuals with an interest in IC in March 2014. Questions were proposed by the EAPCI Women Committee and approved by the EAPCI president and the president-elect. The survey included multiple-choice questions (Online Table 1), as well as open replies. It was not mandatory to reply to the entire questionnaire. Six percent (58 individuals) of respondents chose “several reasons” as an option by listing a combination of the predefined answers in a different order of relevance. P. Capranzano and J. Mehilli went through the comments and re-classified them by selecting the first reason deemed as the most important in the list provided by each responder. Considering the very modest number of selections for some of the predefined answers and to simplify the statistics, the following categories were built: lack of opportunity (lack of position available, working in hospital without catheterisation facilities, application not accepted), family reasons (child care and because of partner) and financial reasons (working in private clinic, better salary).
Statistical analysis
The results are reported as counts or proportions (%) for categorical data and median (25th-75th percentiles) for continuous data. For individual level data, differences between women and men as well as between individuals working or non-working in a coronary/structural invasive subspecialty were checked for significance using the chi-squared or Fisher’s exact test where the expected cell value was <5 (categorical variables) or Wilcoxon rank-sum test (continuous variables). Gender-related analysis for the primary objective was performed considering all respondents, considering only individuals who were stated to be cardiologists and finally considering only EAPCI members. A two-sided p-value of <0.05 was considered to indicate statistical significance. Statistical software R version 3.0.2 was used for analysis.
Results
DESCRIPTION OF THE RESPONDENTS
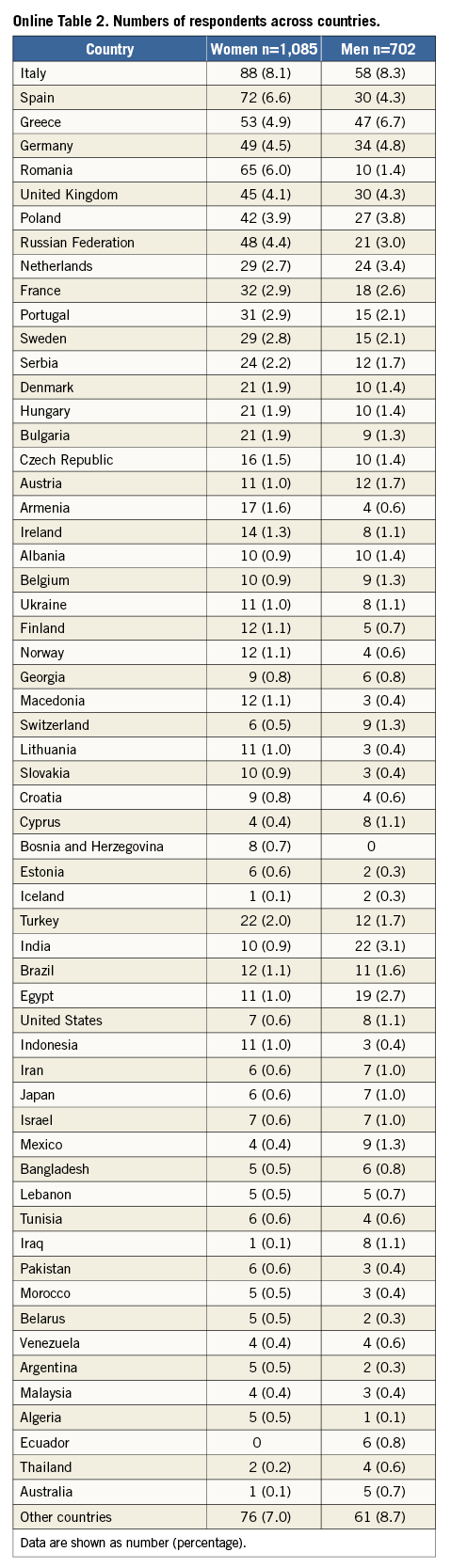
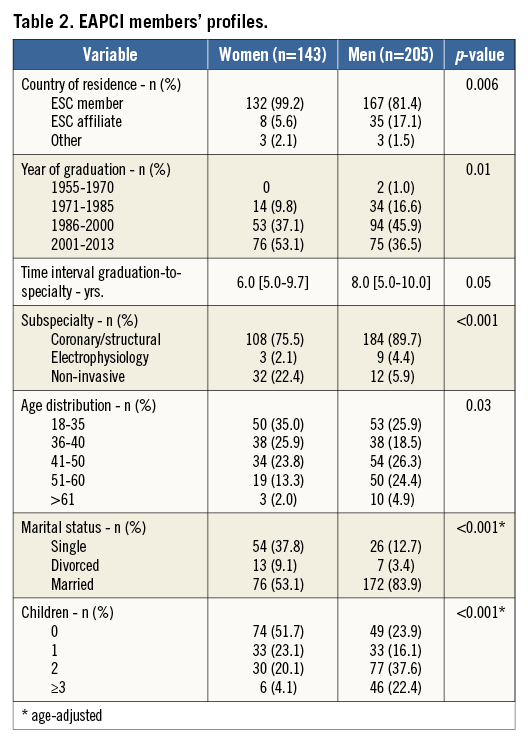
A total of 1,787 individuals (1,085 [60.7%] women and 702 [39.3%] men) responded to the survey. Of these, 348 (19.5%) were EAPCI members and 1,513 (84.5%) were from ESC countries. Numbers of respondents according to gender across countries are listed in Online Table 2. There were significant differences between the proportions of female and male respondents regarding their professional and social profiles (Table 1). Compared to men, women came more frequently from ESC member countries, were younger, nearly half of them had graduated after year 2000, they were less frequently married (57.0% vs. 79.8%, p<0.001) and more frequently childless (46.6% vs. 20.5%, p<0.002) (Figure 1). The proportion of women and men working invasively in a coronary/structural and electrophysiology subspecialty was 30.0% and 10.1%, respectively, p<0.001. In total, 67.5% (143/212) of women and 62.3% (205/326) of men respondents specialising in coronary/structural intervention were members of the EAPCI community (p=0.32). We performed the gender-related analysis on the subgroup of EAPCI members: the same significant differences in the respondents’ profiles were observed (Table 2). Furthermore, we performed a profile analysis of respondents according to their subspecialty. Among men, compared to individuals working in a non-invasive subspecialty, individuals working in a coronary/structural invasive subspecialty were more frequently married (88.3% vs. 80.8%, p=0.006), more frequently had ≥2 children (66.0% vs. 54.1%, p=0.002) and had more frequently graduated between 1986 and 2000 (44.6% vs. 32.1%, p=0.009). Among women, no differences in the social profile between individuals working and not working in a coronary/structural invasive subspecialty were observed regarding marital status (64.2% vs. 64.9%, p=0.8), proportion of women with ≥2 children (31.6% vs. 34.0%, p=0.84) and time frame of graduation (p=0.12). Among invasive-working physicians in the coronary/structural subspecialty, women were less frequently married (p<0.001), less frequently had ≥2 children (p<0.001), and were more frequently younger than 40 years of age (50.6% vs. 37.6%, p<0.001).
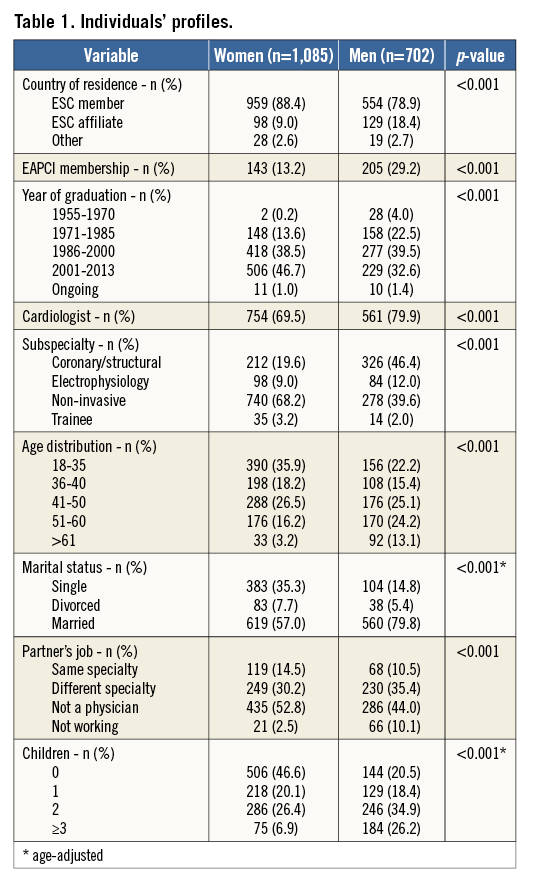
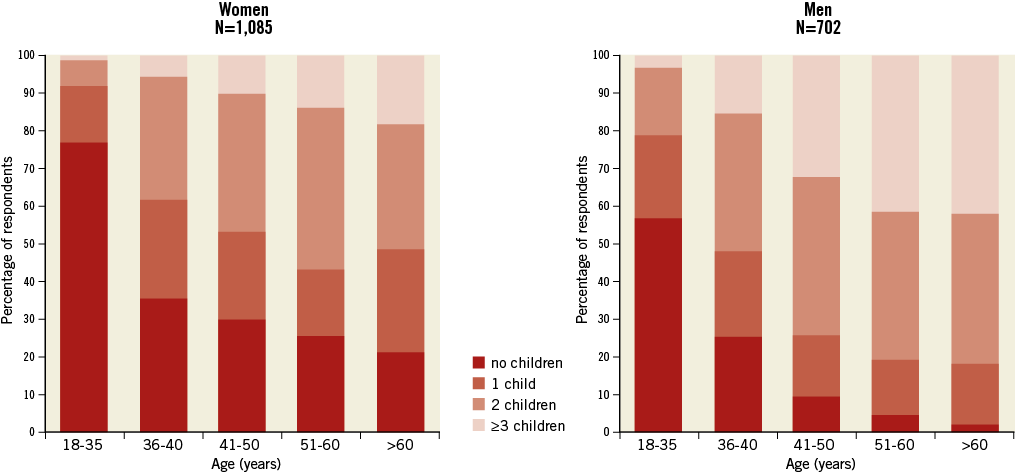
Figure 1. Percentage of respondents with or without children stratified by age.
REASONS FOR CHOOSING INTERVENTIONAL CARDIOLOGY
There were 317 women and 418 men who responded to the question “Why did you choose interventional cardiology?”. The most prevalent answer was “this is/was my passion” (83.3% and 76.1%, respectively). A detailed gender-related description of the answers for all respondents, for cardiologists only as well as for EAPCI members is shown in Table 3.
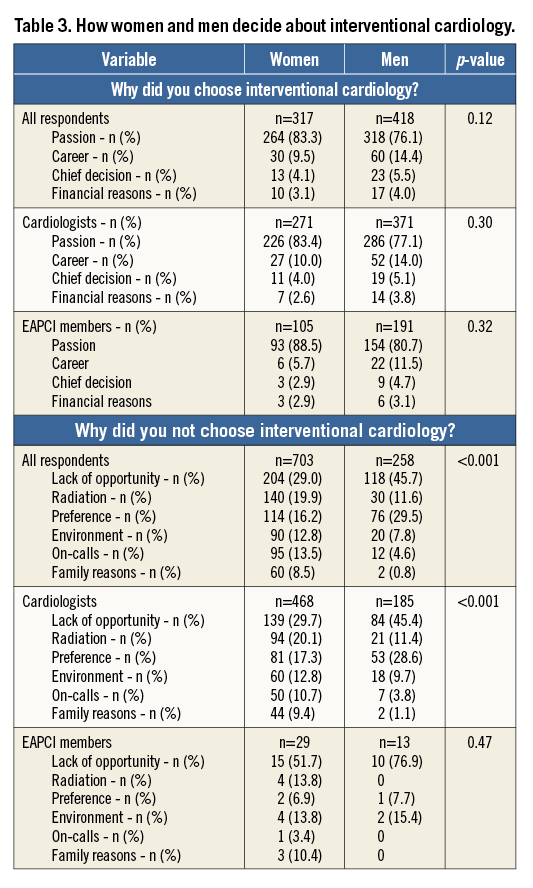
REASONS FOR NOT CHOOSING INTERVENTIONAL CARDIOLOGY
Overall, 703 females and 258 males responded to the question “Why did you not choose interventional cardiology?”. The most frequent reason in both genders for not choosing IC as a subspecialty was lack of opportunity (women vs. men, 29.0% vs. 45.7%), including mostly no position or facilities available (96% vs. 98%), followed by concerns regarding radiation exposure (19.9% vs. 11.6%) and personal preference (16.2% vs. 29.5%). A detailed gender-related description of the answers for all respondents, for cardiologists only as well as for EAPCI members is shown in Table 3.
The prevalence of reasons for individuals not choosing IC as a subspecialty in subgroups stratified by age (less or more than 40 years) is shown in Figure 2 for women and Figure 3 for men. Twice as many women aged <40 years reported that the main reason for not choosing IC was due to concerns regarding radiation exposure compared to women aged >40 years.
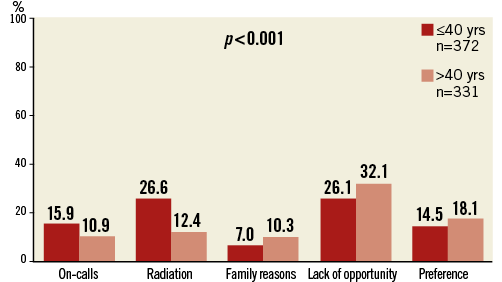
Figure 2. Reasons for women not choosing interventional cardiology stratified by age.
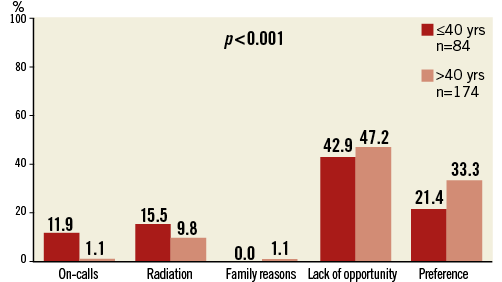
Figure 3. Reasons for men not choosing interventional cardiology stratified by age.
REASONS FOR WOMEN NOT CHOOSING INTERVENTIONAL CARDIOLOGY ACCORDING TO MEN
According to the 652 men responding to this question, on-calls and long working hours were the most frequent reasons (35.3%) for women not choosing IC (Figure 4). There were 58 open replies to the question about why women do not choose IC according to men. The latter open answers are as follows: work conditions considered too challenging, stressful, demanding and not suitable for women (39.6%); male-dominated environment (32.8%); issues related to pregnancy and family care (22.4%); no/other interests (3.4%); and lack of a positive female model (1.7%). Some examples of open replies from men are as follows: “it is a misogynistic environment, probably due to the “tough” mind-set needed to deal with all the emergencies encountered in IC”; “women do not have good hand working under stress conditions”; “it needs more adrenaline and testosterone”; “there is a proven tendency of better orientation and coordinate hand orientation in men than women”.
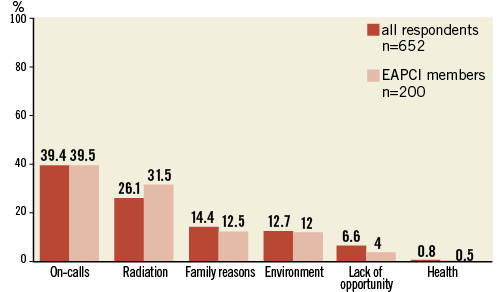
Figure 4. Reasons for women not choosing interventional cardiology according to men.
Discussion
This survey was undertaken by the EAPCI Women Committee to understand factors affecting women’s choice of IC as a subspecialty, in order to plan and implement effective strategies to impact positively on their career decisions. The main findings of the present survey include: i) nearly half of women respondents graduated after the year 2000, probably in accordance with current trends showing an increasing number of female students in medicine; ii) women were less likely to be married and to have children compared with men; iii) although two thirds of women respondents worked in non-invasive subspecialties, a relatively small proportion of them (16.2%) were not interested in IC, which was almost half the proportion of men (29.5%); furthermore, while for three quarters of men respondents the lack of opportunity due to system-related limitations was the reason not to choose IC, for more than half of women concerns particularly related to radiation exposure among younger ones were the most frequent reasons; iv) according to men, women do not choose IC predominantly due to issues related to the pattern and load of the required work, considered it too challenging, demanding or incompatible for women.
CONCERNS REGARDING RADIATION EXPOSURE FOR WOMEN AND DURING PREGNANCY
In the field of IC, a major issue is the perception of concerns regarding radiation exposure, which either prevents women from pursuing such a career (~25% of young women as shown in the present survey) or forces them to alter training and career plans in cardiology to a field with minimal exposure to radiation. In the ACC Committee survey on Women in Cardiology, ~24% of women chose a career/training track with minimal radiation exposure3.
Professional radiation exposure is associated with a non-negligible lifetime attributable risk of developing malignancy4; however, the prevalence of cancer amongst interventional cardiologists has not been elucidated. The 615 respondents to a survey conducted under the “Women in Innovation” (WIN) Group and distributed through the EAPCI to all catheterisation laboratory staff reported a 2% cancer diagnosis (women: 4.4% and men: 1.8%, p=0.067), with the overwhelming diagnosis among women being breast cancer5. Although biologically plausible, considering the fact that the observed breast cancer incidence among WIN survey respondents is equal to the cumulative breast cancer risk in the overall female population of 4%6, a direct correlation between daily low-dose radiation exposure over several years and cancer cannot be demonstrated.
Nevertheless, radiation protection measures leading to an overall reduction in the effective dose must be adequately used7. In particular, considering the potential higher radiation-related risk for women, the implementation of dedicated protection measures is advisable. The use of a lead apron with sleeves, which ensures full coverage of the axillary area, in addition to a dedicated breast shield, should become mandatory for women. Moreover, in order to overcome the fact that lack of awareness of the radiation-related hazards among women turns into fear which can preclude the choice of IC as a subspecialty, formal education and training must be implemented for women, especially during pregnancy, to understand the actual magnitude of the radiation-related risk and strategies to limit the operator effective dose. The recent reports about the lack of knowledge of radiation safety among medical residents emphasises the immediate need for dedicated educational activities8.
A further unique issue related to radiation exposure is about pregnant women working in a catheterisation laboratory. There is great disparity in the approach to pregnant radiation-exposed workers across countries, with about 20% of pregnant females continuing to work in the cardiac catheterisation laboratory4. In Italy, the national law requires women working with radiation to communicate their pregnancy as soon as known, and thereafter entry to an exposed area is absolutely forbidden throughout pregnancy. In other European countries, the law states that the environment must guarantee that the foetus will not receive more than 1 mSv throughout the pregnancy. Indeed, based on the available evidence, heritable or developmental risks to the foetus of pregnant interventional cardiology staff are extremely low, similar to those of the general population, provided that dose limits are respected5,9. However, careful and frequent monitoring of the under lead radiation, appropriate fit and thickness of lead aprons, radiation shielding, adherence to radiation safety protocols, and work restrictions, are warranted to minimise radiation exposure during pregnancy and should be part of the guidelines9.
FAMILY LIFE AND INTERVENTIONAL CARDIOLOGY
The reasons why fewer professional women are married or have a family were not explicitly asked for in our survey, but it has been suggested that the burden of the family responsibilities falls disproportionately to the woman, thus potentially impeding her career choices and advancement by both personal preference and external indirect discrimination2,10,11. Thus, it seems that women, much more than men, have to choose between having a career or a family. Indeed, in our survey, family issues were reasons for precluding the choice of IC in about 10% of women and in less than 1% of men.
In order to reconcile working and family life for women, strategies aiming to promote a balanced participation of women and men in family and working life are needed. According to EU directives, some of these latter strategies include: granting working men rights likely to allow them to provide major support for family life; developing support services for families; granting, where appropriate, specific protection to single-parent families; developing incentives and support measures for non-governmental organisations committed to promoting equal opportunities12. Besides sharing of parental responsibilities, more liberal leave and increased flexibility in work hours may allow more professional females to have children and families, and both sexes to achieve a healthier work/life balance.
MISCONCEPTIONS REGARDING WOMEN’S ROLE AS INTERVENTIONAL CARDIOLOGISTS
An intriguing finding of our survey is that men, including both cardiologists and EAPCI members, considered the pattern and load of catheterisation laboratory work to be a barrier for women in choosing IC. This reveals a stereotype of a woman being fragile, unsuitable to the demanding work and unable to handle challenging and stressful situations that often occur in the cardiac catheterisation laboratory. This specific stereotype determines the “self-fulfilling prophecy”, according to which preconceptions, along with actual organisational barriers, lead to exclusion of women from an IC career, further nourishing the false idea that women are unsuited to the catheterisation laboratory lifestyle13. These prejudices set the basis for an unreasonable preclusion of women from training and for inducing a male-dominated interventional environment with about 90% of workers being men, which is a reason for about 13% of women for not pursuing a career in the field of IC.
The underrepresentation of women has, to a similar extent, been observed in the non-medical field, as shown in a European Commission survey about gender equality in the boardrooms of companies listed on stock exchanges in the 27 member states. On average, only 13.7% of board members are women, despite the suggested evidence of the benefits of gender diversity for company performance14. Similarly, despite the fact that having more women in the catheterisation laboratory may contribute to a more efficient and innovative working environment, mainly due to a more cooperative mindset, which incorporates a wider range of perspectives and therefore reaches more balanced decisions, the female gender is still unreasonably underrepresented in IC.
Despite measures to ensure both genders have equal opportunities, including taking up leadership positions, the road to effective gender professional equality remains long and full of obstacles, particularly in the field of IC15. Indeed, in recent years, tangible progress in gender equality, especially in senior and leadership positions, is the exception and not the rule. As noted in non-medical fields, progress is only visible in countries where legal quotas were adopted16. It is hoped that, in the IC environment, quotas will never be necessary. The latter might be considered a defeat of the intelligence distinctive of our environment with the intention that our sustained efforts will even gender disparity in the field of IC.
Limitations
The main limitation of our study is that of sampling bias, due to the voluntary nature of the survey, and consequently the sample may not necessarily be reflective of the whole cardiology and IC community. The higher proportion of female respondents in this survey may be a consequence of this being an initiative for them and thus men may have been less interested in this topic. It may also be possible that women with positive experience in the IC field have not been interested in this survey. However, for the first time within EAPCI, this survey represents a systematic approach to shedding light on potential obstacles for women entering the IC field in the contemporary era.
The survey did not allow for multiple responses to the multiple-choice questions, forcing the respondent to choose one answer, which is not so clear-cut in the real world and may have resulted in an underestimation of concerns. However, there was a box stating “several reasons” and there was the possibility of adding open replies and comments at the discretion of respondents.
Conclusions
The present EAPCI Women Committee survey demonstrates that several barriers precluding women from choosing interventional cardiology as a subspecialty persist. This highlights the need to develop new strategies for future training, education, and support of women interventional cardiologists, which is a main goal of the EAPCI Women Committee. The main mission of this committee is supported by the European Treaties, which will enable the adoption of measures to ensure equal treatment in matters of employment, occupation, promotion and training opportunities for women.
| Impact on daily practice Although the number of women cardiologists continues to increase, very few of them become interventional cardiologists. Against the widespread opinion among male physicians that invasive specialties are too challenging and demanding for women, concerns about the radiation exposure and lack of flexibility in working hours, as well as insufficient support services for family, are the most frequent reasons impeding particularly young women from selecting the interventional cardiology career path. These findings of the EAPCI Women Survey urge development of new strategies of training, education and support for women working in invasive specialities, particularly with regard to the current reality of a greater proportion of women among medical students. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data