Abstract
Background: Transcatheter mitral valve implantation (TMVI) represents a novel treatment alternative for patients with severe mitral regurgitation (MR) considered ineligible for standard therapies. Data on the management of patients after TMVI screening are scarce.
Aims: We aimed to investigate outcomes of patients with severe MR undergoing TMVI evaluation treated with either TMVI, bailout-transcatheter edge-to-edge repair (bailout-TEER) or medical therapy (MT).
Methods: Between May 2016 and February 2021, 121 patients with MR considered ineligible for standard therapy were screened for TMVI. Outcomes were assessed for the subgroups of patients treated with TMVI, bailout-TEER and MT. The primary composite endpoint was all-cause death or heart failure hospitalisation after one year.
Results: The subgroups of TMVI (N=38), bailout-TEER (N=28) and MT (N=44) differed significantly with regard to MR aetiology (secondary MR: TMVI 68.4%, bailout-TEER 39.3%, MT 38.6%, p=0.014) and left ventricular ejection fraction (TMVI 37.0% [31.4-51.2], bailout-TEER 48.0% [35.3-58.3], MT 54.5% [40.8-60.0], p<0.001). At discharge and after one year, MR was reduced to ≤mild residual MR in all patients undergoing TMVI, while ≥moderate residual MR was present in 25.9% and 20.0% of patients, respectively, after bailout-TEER, and in 100.0% of patients on MT at one year. The primary endpoint occurred in 72.2% of patients remaining on MT, in 51.6% of patients undergoing TMVI and in 40.2% of those receiving bailout-TEER.
Conclusions: In MR patients considered ineligible for standard therapy, TMVI provided acceptable clinical outcomes and MR elimination in the majority of patients. In screen-failed patients, bailout-TEER represented a reasonable alternative while MT was associated with poor outcomes.
Introduction
Mitral regurgitation (MR) is the second most common valve disease in industrialised countries with an increasing incidence in the elderly population1. International guidelines recommend mitral valve surgery (i.e., mitral valve repair or replacement) or transcatheter edge-to-edge repair (TEER) in patients with severe symptomatic MR23. However, due to an advanced age profile, frailty or co-morbidities, half of affected patients are denied open-heart surgery. The majority of these patients are eligible for TEER. However, there are a considerable number of patients who remain ineligible for standard MR therapies, mainly due to anatomical reasons24. For these patients, transcatheter mitral valve implantation (TMVI), as a novel and minimally invasive treatment approach, has demonstrated promising preliminary results and might therefore evolve into a complementary treatment strategy567. Although data on TMVI are scarce, the main advantage of TMVI seems to be a more individualised and patient-tailored treatment, with different sizes and various designs of mitral valve devices resulting in predictable elimination of MR8. Nevertheless, recent studies demonstrated high screening failure rates, leaving a relevant portion of patients to medical therapy (MT) alone910. Guideline-directed MT is an important cornerstone of MR treatment and is recommended for all patients with secondary MR (SMR) according to current guidelines2. However, the mortality of patients treated with MT only, especially after TMVI screening failure, remains high1112. Therefore, despite presumed suboptimal anatomies, the option to perform TEER as a bailout therapy for these patients is frequently considered.
The present study gives a precise description of a single-centre experience with the management of patients with MR who were considered ineligible for standard therapy and consequently underwent either TMVI, bailout-TEER or remained on MT.
Methods
Study design
A total of 121 patients with severe MR were screened for at least one TMVI device from May 2016 to February 2021 and included in the Hamburg TranscathEteR Mitral Valve Replacement RegiStry (HERMES; ClinicalTrials.gov: NCT04914468). The interdisciplinary TMVI screening process has been described in detail before10. All patients undergoing TMVI evaluation were considered suboptimal TEER candidates at high or prohibitive surgical risk. TMVI devices were implanted via transapical (Tiara [Neovasc], Tendyne [Abbott Vascular], HighLife Valve [HighLife Medical]) or transseptal access (i.e., CardiAQ [Edwards Lifesciences]). If screen-failed for TMVI, patients underwent either bailout-TEER or remained on MT. Only a minority of patients underwent high-risk surgery or transcatheter annuloplasty. These patients were excluded from the study. The present study investigated the management, characteristics and outcomes of patients undergoing TMVI screening according to the treatment decision (TMVI, bailout-TEER or MT). All decisions concerning screening and treatment of patients were made by mutual consent of an interdisciplinary Heart Team.
Index dates were defined as the implantation date for the TMVI and bailout-TEER groups and the date of first device screening for the MT group. Follow-up information and survival data were collected by scheduled ambulatory follow-up visits, telephone follow-up after 12 months and yearly thereafter or by hospital records. The study was approved by the local ethics committee and was conducted in accordance with the Declaration of Helsinki.
Echocardiographic analysis
All patients underwent transthoracic and transoesophageal echocardiography for evaluation of MR aetiology and MR severity (none/trace, mild, moderate or severe MR). Assessment of the mitral valve was performed by experienced personnel according to the 2017 European Society of Cardiology (ESC) guidelines for the management of valvular heart disease2. Routinely assessed parameters included left ventricular ejection fraction (LVEF), left ventricular (LV) diameters (LV end-diastolic and end-systolic diameter [LVEDD, LVESD]) and volumes (LV end-diastolic and end-systolic volume [LVEDV, LVESV]), mean transvalvular pressure gradients and pulmonary artery systolic pressure (PASP). Right ventricular (RV) function was assessed by tricuspid annular plane systolic excursion (TAPSE).
Cardiac CT analyses
Electrocardiogram-gated full cardiac cycle multislice computed tomography (CT) was performed in every patient as part of a standardised screening protocol. A dedicated software (3mensio Structural Heart, version 9.1; Pie Medical Imaging) was used for anatomical assessment of the mitral valve annulus. In this study only systolic measurements are presented. The extent of mitral annular calcification (MAC) was documented using semiquantitative categories. The D-shaped annulus concept was utilised for examination of the mitral valve annulus.
Endpoints
In-hospital and 30-day outcomes of patients undergoing TMVI were assessed according to the predefined endpoints of the Mitral Valve Academic Research Consortium (MVARC). The functional outcome of patients was reported according to New York Heart Association (NYHA) Functional Class I to IV at baseline and one year after intervention/screening. The echocardiographic outcome was assessed as MR severity at baseline, at discharge and at one year. The primary composite endpoint was defined as all-cause death or heart failure (HF) rehospitalisation one year after intervention/screening. Singular secondary study endpoints were defined as all-cause death at one year and cardiovascular (CV) death one year after intervention/screening. Endpoints were not internally adjudicated. HF rehospitalisation was defined as the incidence of new-onset or worsening signs and symptoms of HF that required urgent therapy and resulted in hospitalisation. CV death was defined as death attributable to myocardial ischaemia and infarction, HF, cardiac arrest due to other or unknown cause, or cerebrovascular incidents.
Statistical analysis
Continuous variables are summarised by medians (interquartile ranges [IQR]) and categorial variables are displayed as counts (frequencies). The Kruskal-Wallis test was used for comparison of continuous variables and Fisher’s exact test was performed for comparison of categorial variables at baseline. To compare follow-up data to baseline, the paired Mann-Whitney U-test was performed. The Kaplan-Meier method was used for estimation of all endpoints at one year. Censoring of the outcomes at one-year follow-up was conducted by setting all events occurring after the one-year threshold to no event and all corresponding time ranges to the maximum of one year. Groups were compared using the log-rank test (two-tailed). Univariate Cox regression for a predefined subset of parameters was calculated for each subgroup. Forest plots display the respective hazard ratio (HR), 95% confidence interval (CI), and p-value (two-tailed). A p-value of less than 0.05 was considered statistically significant. Statistical analyses were performed with R statistical software, version 4.0.3 (R Foundation for Statistical Computing).
Results
Clinical and imaging baseline characteristics
A total of 110 patients were included in the present study. Of these, 38 patients underwent TMVI, 28 patients were treated with bailout-TEER and 44 patients remained on MT. A study flow chart is given in Figure 1. A detailed comparison of clinical baseline characteristics between the subgroups of TMVI, bailout-TEER and MT is given in Table 1.
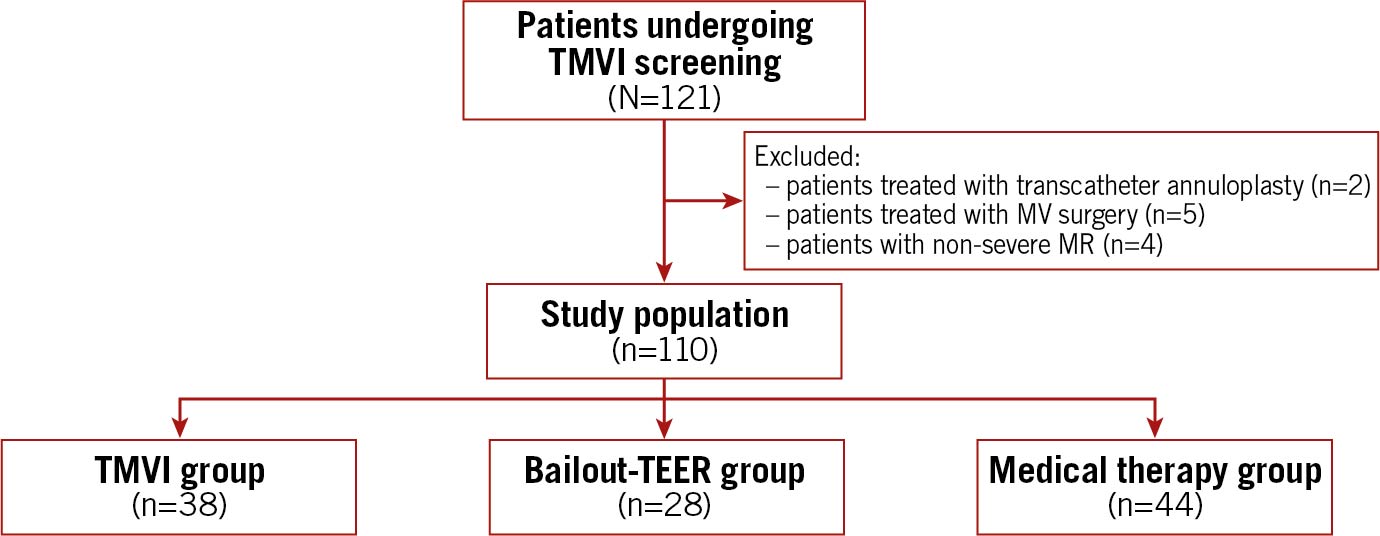
Figure 1. Study flow chart. MR: mitral regurgitation; MT: medical therapy; MV: mitral valve; TEER: transcatheter edge-to-edge repair; TMVI: transcatheter mitral valve implantation
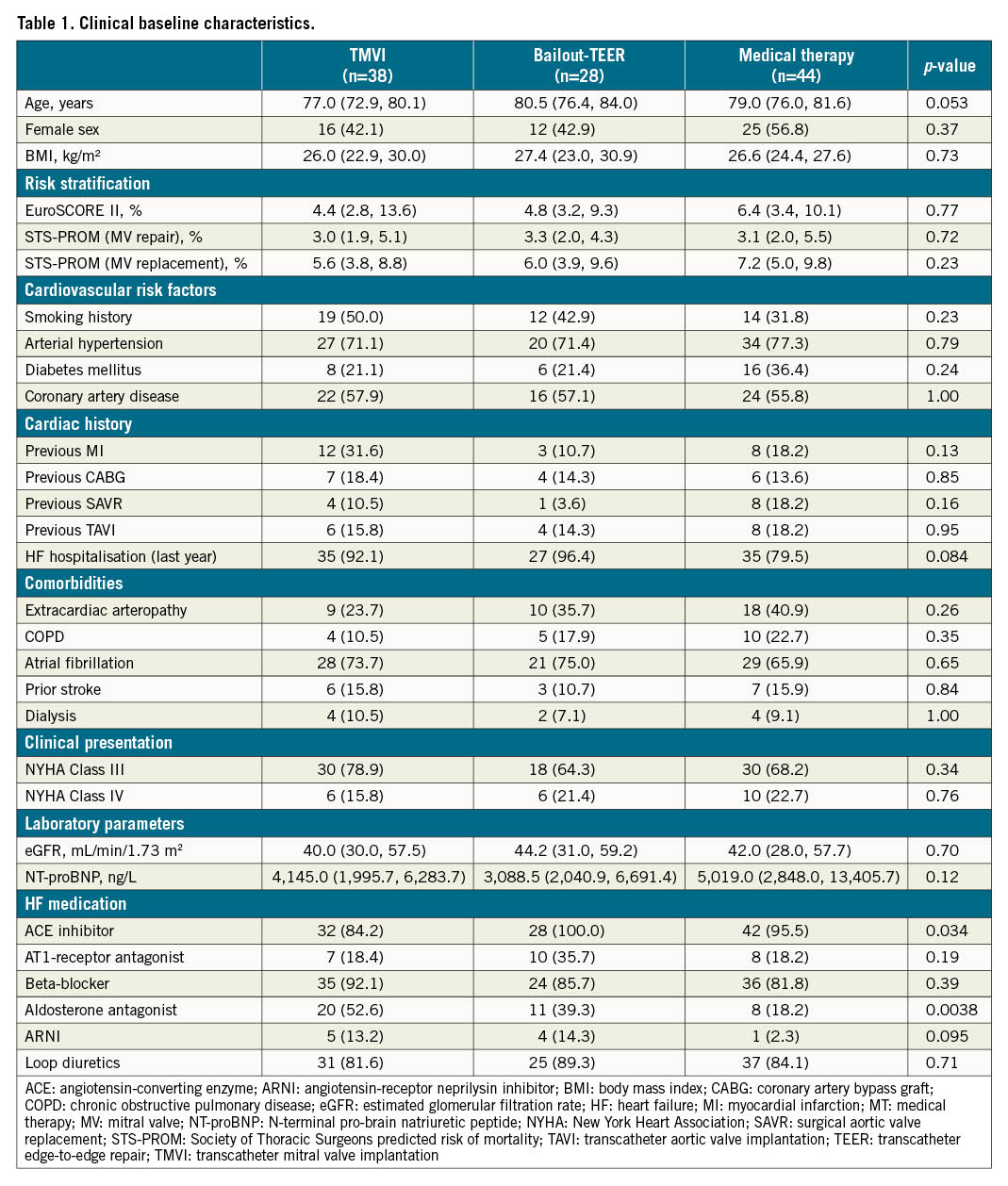
There was no difference between the subgroups regarding age (TMVI 77.0 [IQR 72.9-80.1], bailout-TEER 80.5 years [IQR 76.4-84.0], MT 79.0 years [IQR 76.0-81.6], p=0.053 or gender (female: TMVI N=16 [42.1%], bailout-TEER N=12 [42.9%], MT N=25 [56.8%], p=0.37). Estimated surgical risk among all groups was elevated according to EuroSCORE II (TMVI 4.4% [IQR 2.8-13.6], bailout-TEER 4.8% [IQR 3.2-9.3], MT 6.4% [IQR 3.4-10.1], p=0.77) as well as the Society of Thoracic Surgeons Predicted Risk of Mortality (STS PROM) for mitral valve repair (TMVI 3.0% [IQR 1.9-5.1], bailout-TEER 3.3% [IQR 2.0-4.3], MT 3.1% [IQR 2.0-5.5], p=0.72) and mitral valve replacement (TMVI 5.6% [IQR 3.8-8.8], bailout-TEER 6.0% [IQR 3.9-9.6], MT 7.2% [IQR 5.0-9.8], p=0.23). The majority of patients in all three groups were highly symptomatic according to NYHA Functional Class III or IV and there was no difference between the groups regarding rates of cardiovascular and non-cardiovascular comorbidities.
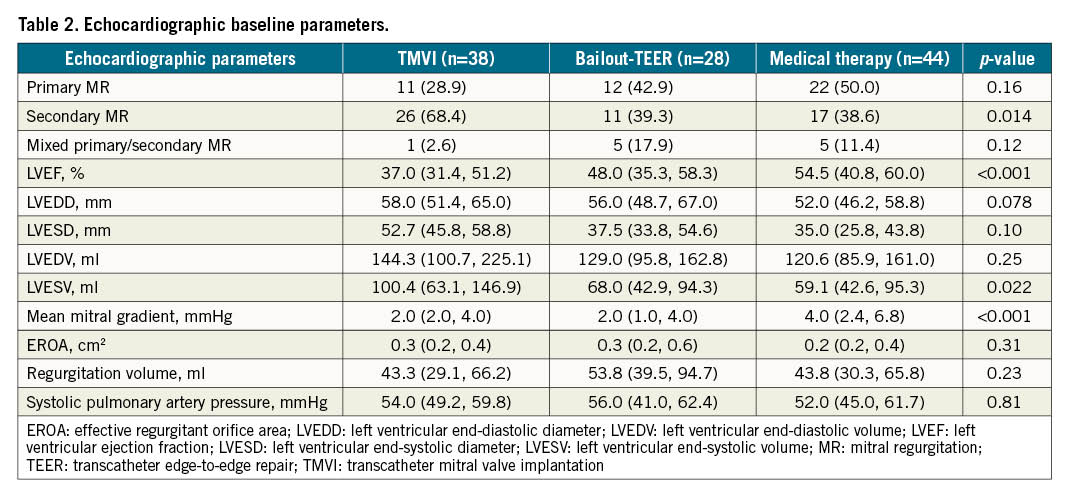
Baseline echocardiographic parameters are summarised in Table 2. Significant differences between the three groups were found regarding MR aetiology, LV dimensions and transvalvular gradients. SMR was present in the majority of patients undergoing TMVI (N=26 [68.4%]), while the predominant MR aetiology in screen-failed patients undergoing bailout-TEER or MT was primary MR (bailout-TEER N=12 [42.9%]; MT N=22 [50.0%]). In patients receiving TMVI, LV dimensions were larger (e.g., LVESV 100.4 mL [IQR 63.1-146.9]) and LVEF was lower (37.0% [IQR 31.4-51.2]) compared to patients who underwent bailout-TEER or MT (p<0.001 for LVEF, p=0.022 for LVESV). Mean mitral valve pressure gradients were highest in patients remaining on MT (4.0 mmHg [IQR 2.4-6.8]) compared to patients undergoing mitral valve interventions (TMVI 2.0 mmHg [IQR 2.0-4.0]; bailout-TEER 2.0 mmHg [IQR 1.0-4.0]; p<0.001).
CT parameters at baseline are listed in Supplementary Table 1. Circular MAC was most present in the MT group (N=14, 35.0%), while only three patients undergoing TMVI (10.0%) and no patients in the bailout-TEER group had circular MAC (p<0.001).
Reasons for TMVI screening failure
Figure 2 gives an overview of reasons for TMVI screening failure across six different devices in the bailout-TEER group and the MT group. Reasons for refusal were available in 136 out of 193 cases of device screening failure. The most common reason for TMVI screening failure in both groups was small LV size (bailout-TEER 37.9%, MT 28.2%). While mitral annular sizes outside the treatment range for TMVI were more common in the bailout-TEER group (large annulus: 27.6%, small annulus: 3.5%) compared to the MT group (large annulus: 14.1%, small annulus: 11.5%), conversely MAC was a reason for screening failure in more patients undergoing MT (25.6%) than bailout-TEER (6.9%). The risk of significant neo-LV outflow tract obstruction was a major limiting factor in both groups (bailout-TEER 24.1%, MT 20.5%).
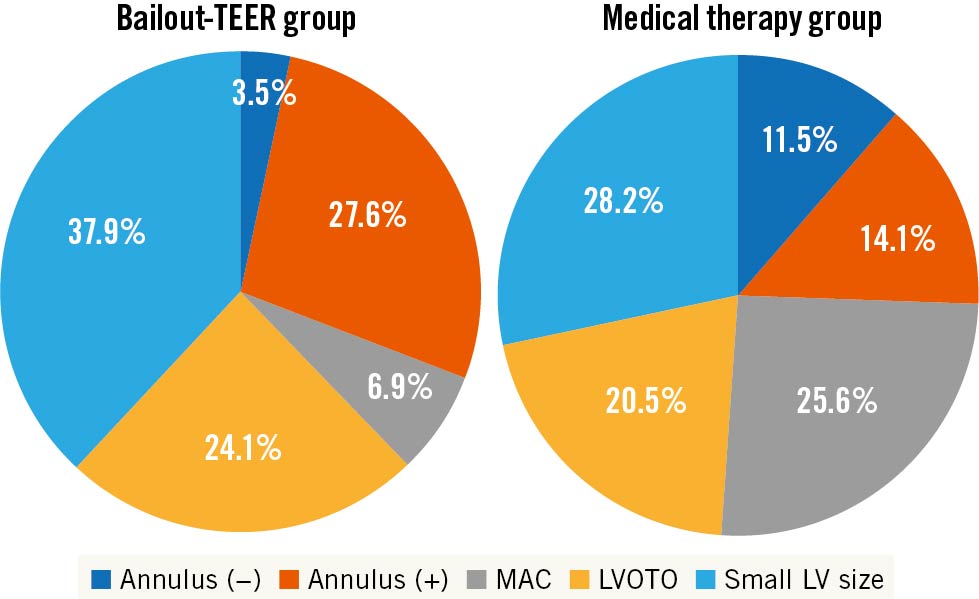
Figure 2. TMVI screening failure reasons. annulus (-): small annulus size; annulus (+): large annulus size; LV: left ventricle; LVOTO: left ventricular outflow tract obstruction; MAC: mitral annular calcification; MT: medical therapy; TEER: transcatheter edge-to-edge repair; TMVI: transcatheter mitral valve implantation
Follow-up
During a median follow-up time of 2.25 years (1.94-3.29) a total of 48 deaths occurred. Complete follow-up at one year was available in 82.7% (TMVI 76.3%, TEER 75.0%, MT 93.2%) for all-cause death and in 81.8% (TMVI 71.1%, TEER 78.6%, MT 93.2%) for the combined endpoint of all-cause death or HF rehospitalisation. Echocardiographic, functional and clinical outcomes are separately presented for each subgroup below.
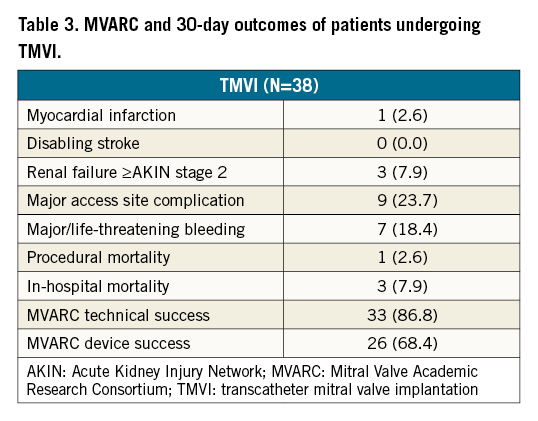
Procedural data and outcomes of patients undergoing TMVI
In-hospital and 30-day outcomes of patients undergoing TMVI according to MVARC-predefined endpoints is given in Table 3. For the vast majority of implanted devices in the TMVI group, a transapical approach was used (N=36, 94.7%). MVARC-defined technical success was achieved in 86.8% (N=33). Three patients (7.9%) had periprocedural complications: one patient suffered from an acute to chronic kidney failure and another patient showed a temporary tamponade of the left atrium. Immediately after implantation of the prosthesis in one patient, atrial migration of the prosthesis occurred, which made a conversion to surgical open-heart mitral valve replacement necessary. One patient (2.6%) died shortly after intervention from the consequences of a pericardial effusion. Rates of myocardial infarction (2.6%), disabling stroke (0.0%) and renal failure (≥acute kidney injury network stage 2, 7.9%) were low. Major access site complications and major or life-threatening bleeding occurred in 23.7% and 18.4%, respectively. In-hospital mortality was 7.9% (N=3) and MVARC-defined device success was 67.4% (N=26).
At discharge, MR was reduced to mild (24.2%) or none/trace MR (75.8%) in all patients undergoing TMVI (p<0.001) (Figure 3A). At one year, MR elimination (MR <1+) was still observed in the majority of patients (68.8%; p<0.001). At one-year follow-up, significant functional improvement was observed for the TMVI group (p<0.001) classifying 17.6% and 82.3% of patients as NYHA Functional Class III and II, respectively. Importantly, none of the patients followed-up after one year were classified as NYHA IV (Figure 3B). The primary composite endpoint of all-cause death or HF rehospitalisation at one year occurred in 51.6% of patients undergoing TMVI. All-cause death and cardiovascular death rates at one year were 34.6% and 27.2%, respectively (Figure 4).
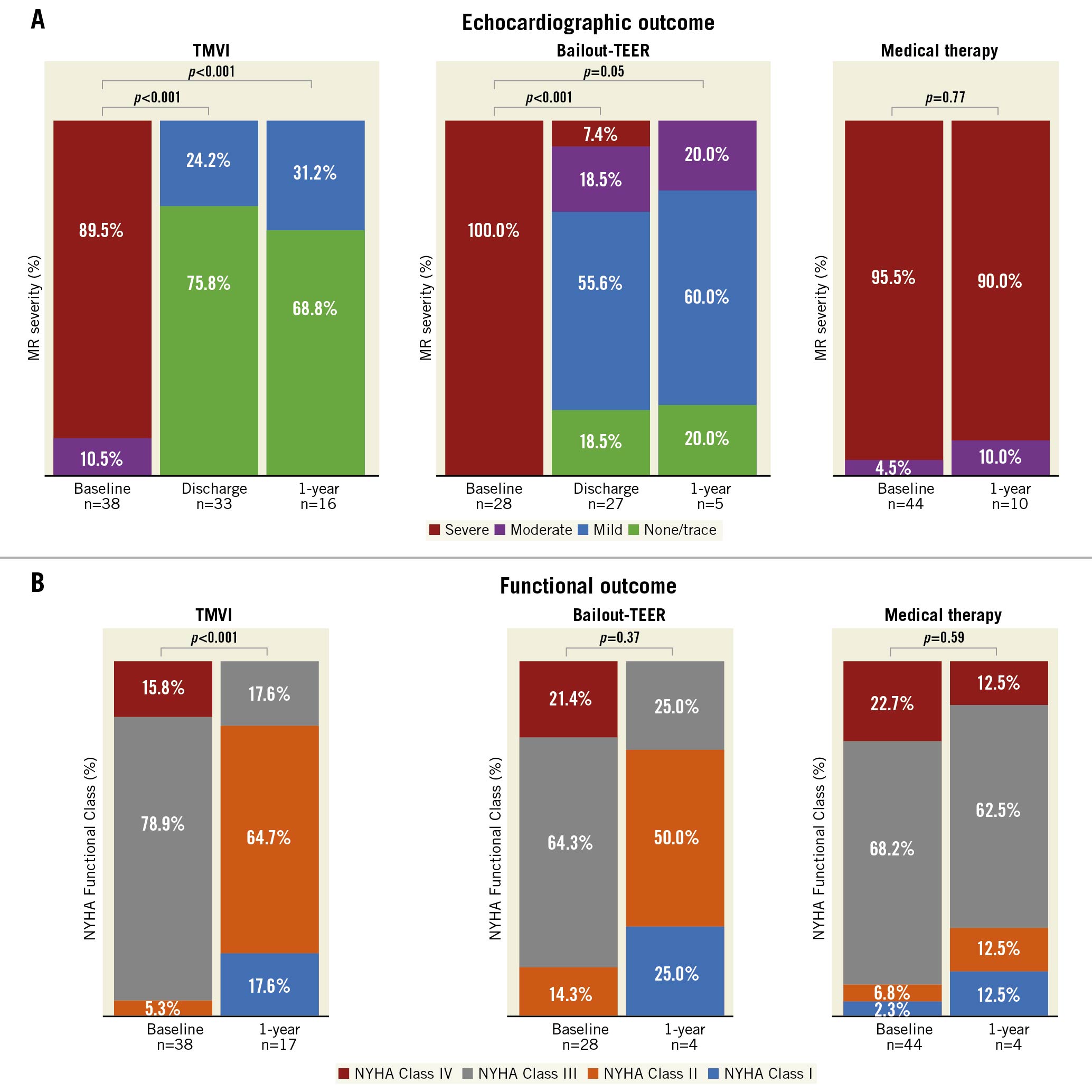
Figure 3. Echocardiographic and functional outcomes. A. Echocardiographic outcome at discharge and at one year. B. Functional outcome after one year. MR: mitral regurgitation; NYHA: New York Heart Association; TEER: transcatheter edge-to-edge repair; TMVI: transcatheter mitral valve implantation
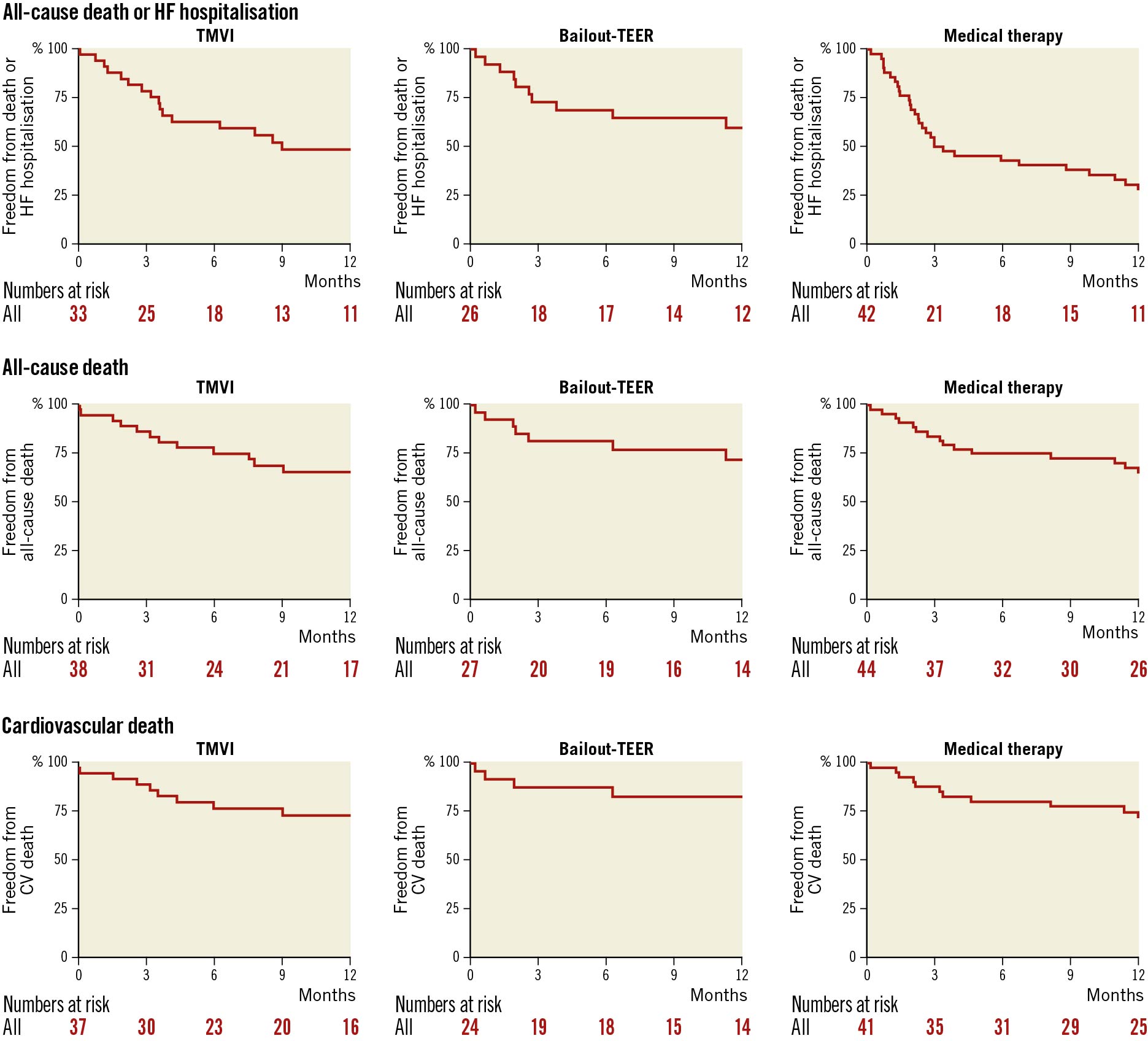
Figure 4. Kaplan-Meier analyses for the primary endpoint of all-cause death or HF rehospitalisation after one year, and the secondary endpoints of all-cause death and cardiovascular death after one year. CV: cardiovascular; HF: heart failure; MT: medical therapy; TEER: transcatheter edge-to-edge repair; TMVI: transcatheter mitral valve implantation
Outcomes of patients undergoing bailout-TEER
In patients receiving bailout-TEER, MR was reduced to mild (55.6%) or none/trace (18.5%) in the majority of patients at discharge, while in 18.5% of these patients MR was still moderate and 7.4% remained with severe MR (p<0.001) (Figure 3A). Outpatient follow-up of patients undergoing bailout-TEER was poor. In echocardiographically followed-up patients (N=5), 20.0% (N=1) presented with moderate MR (p=0.05). Of the four patients with functional follow-up, 75% (N=3) were at NYHA Functional Class I or II (p=0.37) (Figure 3B). The rate of the primary composite endpoint at one year was 40.2% in patients treated with bailout-TEER, representing the lowest rate among all three subgroups. All-cause death and cardiovascular death at one year after bailout-TEER occurred in 28.0% and 17.4% of patients, respectively (Figure 4).
Outcomes of patients on medical therapy
MR severity of screen-failed patients remaining on MT was assessed at baseline and after one year. At one-year follow-up, MR remained moderate (10.0%) or severe (90.0%) in all followed-up patients (p=0.77) (Figure 3A). Regarding functional outcome after one year, no change of NYHA Functional Class could be detected in the MT group compared to baseline functional status, with 75.0% of patients remaining in NYHA Functional Class III or IV (p=0.59) (Figure 3B). The primary composite endpoint occurred in 72.2% of patients remaining on MT at one year after screening, representing the highest rate among all subgroups. All-cause death and cardiovascular death rates after one year were 34.9% and 28.1%, respectively (Figure 4).
Predictors of outcome
Predictors of the combined endpoint of all-cause death or HF rehospitalisation after one year, assessed by univariate Cox regression analysis, are demonstrated for all subgroups in Figure 5. For the subgroup of patients undergoing TMVI, none of the investigated demographic, clinical and echocardiographic parameters were significantly associated with the combined endpoint. The strongest association with the combined endpoint was found for chronic obstructive pulmonary disease (COPD; HR 2.80, 95% CI: 0.79-9.93, p=0.11). In the bailout-TEER group, both COPD (HR 1.94, 95% CI: 1.04-3.62, p=0.037) and right ventricular (RV) dysfunction (HR 1.91, 95% CI: 1.09-3.35, p=0.023) were significantly predictive of the primary endpoint, while elevated age ≥80 years was a protective factor in univariate analysis (HR 0.52, 95% CI: 0.30-0.91, p=0.021). In patients remaining on MT, only RV dysfunction (defined as tricuspid annular plane systolic excursion <17 mm) was significantly associated with adverse outcome (HR 2.70, 95% CI: 1.23-5.90, p=0.013).
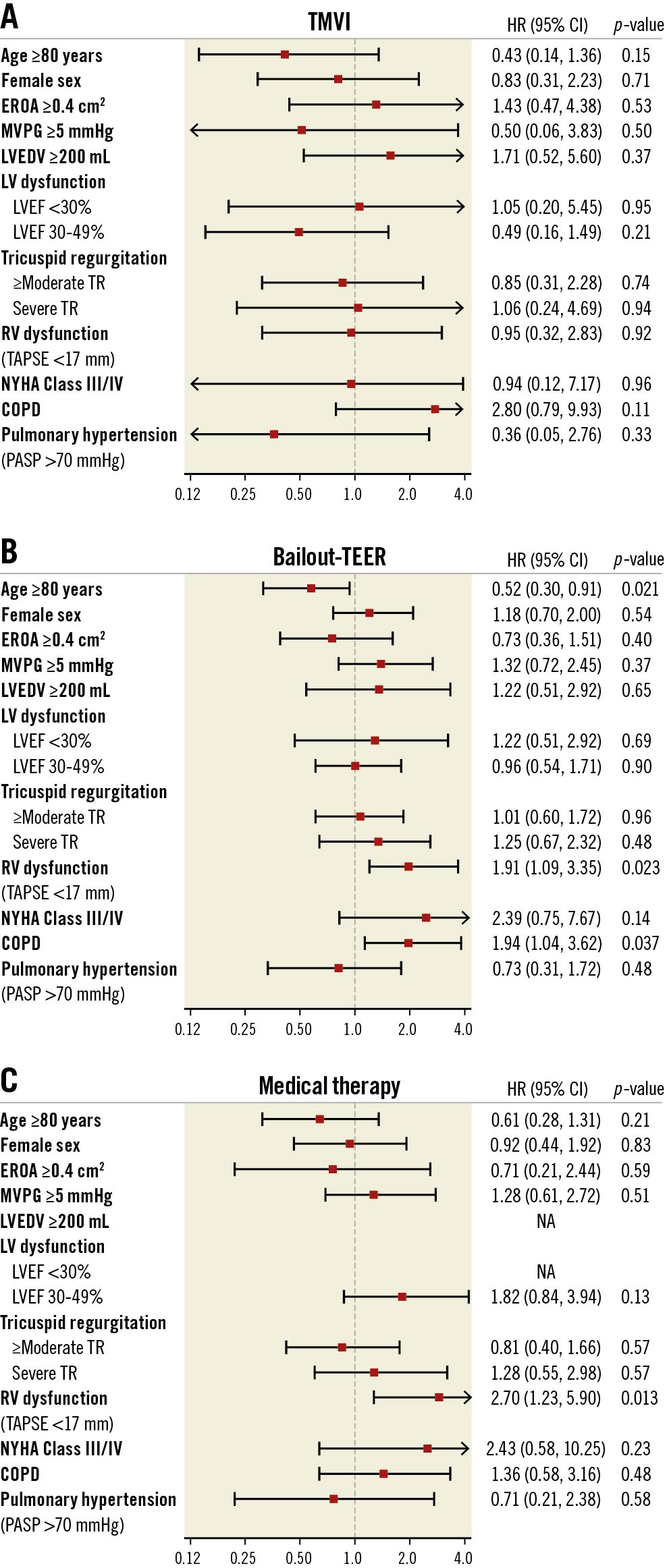
Figure 5. Univariate Cox regression analysis. Combined endpoint (all-cause death or heart failure rehospitalisation after one year). COPD: chronic obstructive pulmonary disease; EROA: effective regurgitant orifice area; LV: left ventricular; LVEDV: left ventricle end-diastolic volume; LVEF: left ventricular ejection fraction; MT: medical therapy; MVPG: mitral valve pressure gradient; NYHA: New York Heart Association; PASP: pulmonary artery systolic pressure; RV: right ventricular; TAPSE: tricuspid annular plane systolic excursion; TEER: transcatheter edge-to-edge repair; TMVI: transcatheter mitral valve implantation
Discussion
The present study gives a comprehensive overview of a single-centre experience with the management of MR patients considered ineligible for standard therapies undergoing TMVI screening (Central Illustration). If screen-failed for TMVI, patients underwent either bailout-TEER or MT. The main findings of this retrospective study can be summarised as follows:
1) The majority of patients with successful TMVI screening were diagnosed with SMR and impaired LVEF, while primary MR and preserved LVEF were more present in screen-failed patients. Small LV size was the most frequent reason for TMVI screening failure in both bailout-TEER and MT patients.
2) Technical success in the TMVI group was high (86.8%) and MR elimination to none/trace or reduction to mild MR persisted in all patients after successful treatment with TMVI up to one-year follow-up. Significant residual MR was found in a considerable portion of patients undergoing bailout-TEER and patients on MT remained with moderate or severe MR.
3) The functional status of patients treated with TMVI had significantly improved at one-year follow-up, while no statistically significant changes of NYHA Functional Class were observed in the bailout-TEER and MT groups.
4) The combined endpoint of all-cause death or HF rehospitalisation after one year occurred in 51.6% of patients undergoing TMVI. The lowest rate of the primary endpoint among all patients screened for TMVI (including those treated with TMVI) was found in patients referred to bailout-TEER (40.2%), while the highest rate occurred in patients under MT (72.2%).
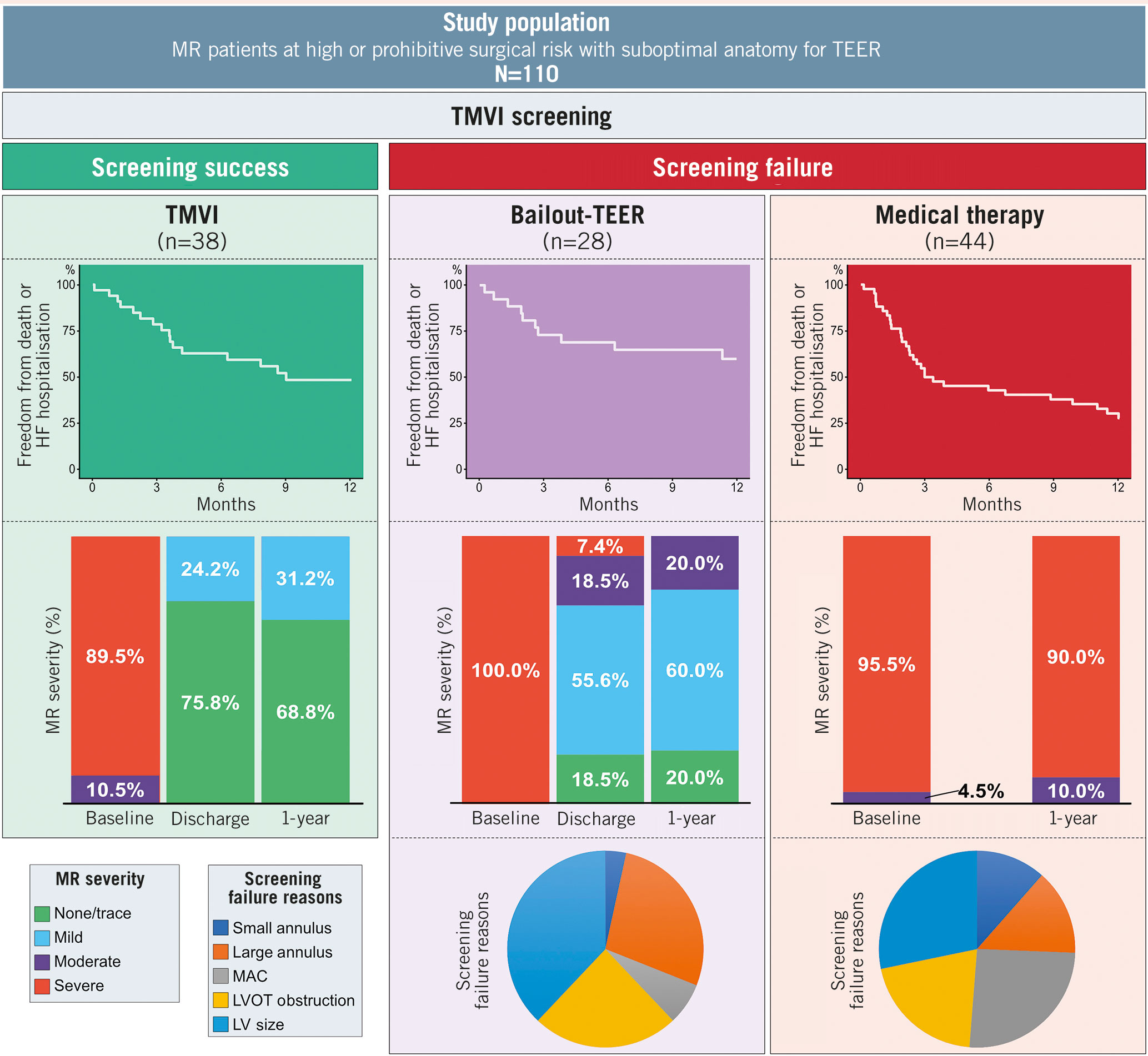
Central Illustration. Management of patients with mitral regurgitation ineligible for standard therapy undergoing TMVI screening; a single-centre experience. HF: heart failure; LV: left ventricular; LVOT: left ventricular outflow tract; MAC: mitral annular calcification; MR: mitral regurgitation; TEER: transcatheter edge-to-edge repair; TMVI: transcatheter mitral valve implantation
Residual MR is a frequent finding after TEER or surgical mitral valve repair and is associated with adverse outcome131415. TMVI is a novel therapeutic alternative for patients considered ineligible for these standard MR therapies offering predictable MR elimination. Similar to the global feasibility trial of the Tendyne mitral valve system, as the largest published TMVI study to date (including 100 subjects), complete MR elimination to none/trivial MR with persistent results after one year was also achieved in the majority of patients treated with TMVI in the present study616. In the Tendyne feasibility trial, technical success was accomplished in 96% of cases and in 86.8% in the present study. Clinical and echocardiographic improvements documented for the TMVI group in the present study largely resemble published clinical trial results with TMVI. High technical success, effective MR elimination and sustained functional improvement seem to be the cornerstones of TMVI therapy. However, the rate of all-cause death after one year was markedly higher in the present study population (34.6% [TMVI group] vs 26.0% [Tendyne global feasibility trial]). A systematic review reported an all-cause death rate of 27.6% after a mean follow-up of 10 months for patients treated with TMVI5. This higher mortality rate may reflect the fact that the present study population represents a real-world, high-risk patient cohort, considered ineligible for both open-heart surgery and TEER, undergoing treatment with different TMVI devices, and also including patients treated in a compassionate-use setting. In general, it seems fair to hypothesise that the patient cohort investigated here exhibits a markedly increased risk profile compared to patients prospectively recruited for clinical trials.
The present study allows for a differentiated statement on outcomes of patients undergoing TMVI screening treated with either TMVI, or (if screen-failed) with bailout-TEER or MT. Overall rates of all-cause death or HF rehospitalisation, and all-cause death or CV death after one year were high in all three groups. This may have been due to an overall elderly, highly symptomatic and comorbid patient population. Although comparability of the three subgroups remains limited due to profound differences regarding MR aetiology and LV anatomy, the rate of the primary endpoint at one year in patients under MT was more than 20% higher compared to those treated with TMVI, and more than 30% higher compared to those referred to bailout-TEER. This difference was mainly driven by a higher rate of HF rehospitalisations in the MT group. In summary, although TMVI did not affect one-year mortality in the current study population, functional status after one year was significantly improved and the number of HF rehospitalisations was reduced compared to patients on MT. In this regard, despite mitral valve anatomies initially considered suboptimal for a TEER procedure, bailout-TEER yielded similar functional improvement, and treated patients showed the lowest overall rates of mortality or HF rehospitalisations.
Current guidelines for the treatment of valvular heart disease recommend MT only under certain conditions and not in general for patients with primary MR23. In contrast, MT in patients with SMR is directed towards the treatment of chronic heart failure17 and has shown solid results18. In the present study, half of the MT group had primary MR but did not undergo surgery, TEER or TMVI even though evidence of MT is low for patients with primary MR19. MT was mainly implemented because no other MR treatment option could be offered to affected patients. Small LV cavity size, a high degree of MAC and elevated mitral valve pressure gradients at baseline in these patients makes them suboptimal candidates for both transcatheter replacement and repair, and since most of these patients suffered from primary MR, MT may not have had sufficient impact on the underlying disease. Niikura et al reported a one-year all-cause death rate of 14.5% in patients ineligible for TMVI who were treated medically11. In the present study, 34.9% of MT patients died after one year. A reason for this difference in outcome might be a stronger functional impairment in the present study, with a particularly high rate of patients in NYHA Functional Class III or IV of 90.9%, which is known to be associated with high mortality2021.
Interestingly, a considerable number of patients initially considered suboptimal for TEER were eventually re-evaluated after TMVI screening failure and underwent bailout-TEER instead of MT. These patients are characterised by a high rate of primary MR, but conversely, a low rate of relevant MAC. Although few patients qualified for bailout-TEER and the rate of significant residual MR was indeed high (25.9% ≥moderate residual MR at discharge), the rate of the primary endpoint was lowest in the bailout-TEER group after one year and the patients’ NYHA Functional Class improved significantly. Our results support the consideration of bailout-TEER as a reasonable treatment option for patients who screen-fail for TMVI, even in the presence of presumably unfavourable TEER-anatomy.
Limitations
This is a single-centre, retrospective study. Therefore, all drawn conclusions may only be hypothesis-generating and need to be validated by prospective studies. The small sample size of this study puts further limits on our conclusions and is mainly due to the novelty of TMVI and its currently limited uptake. Certainly, the results of the global CHOICE-MI registry (ClinicalTrials.gov: NCT04688190) will give a more detailed analysis of the outcomes of patients undergoing TMVI evaluation. However, we are convinced that this study delivers valuable insights into the strengths and limitations of TMVI and the management of patients who are ineligible for standard MR therapy. Differences in outcomes between the subgroups may have been influenced by different predominant MR aetiologies, which represents the central limitation of this study. Moreover, echocardiographic and functional follow-up was poor especially for bailout-TEER and MT patients. The number of patients ineligible for TMVI might be underestimated in our study due to a certain preselection bias of patients undergoing TMVI screening. Additionally, endpoints were not adjudicated. Despite a clear definition of endpoints, this might have had an impact, particularly on the definition of hospital admissions as HF rehospitalisations. Finally, the competing risks of congestive HF admissions and death need to be considered in the interpretation of the presented results.
Conclusions
This present study outlines a single-centre experience with the management of MR patients considered ineligible for standard therapies undergoing TMVI screening. TMVI resulted in predictable MR elimination and functional improvement over time in the majority of patients. In screen-failed patients, MT was associated with poor clinical outcomes, while bailout-TEER should be considered even in the presence of suboptimal anatomy.
Impact on daily practice
The present study gives a comprehensive overview of a single-centre experience of the management of patients with severe mitral regurgitation (MR) considered ineligible for standard therapies undergoing screening for transcatheter mitral valve implantation (TMVI). The results emphasise the strengths and limitations of TMVI as a novel and promising therapy providing predictable MR elimination in most patients. Although only feasible in a limited number of patients, transcatheter edge-to-edge repair (TEER) remains a reasonable option for patients with suboptimal TEER-anatomy. The majority of screened patients remained on medical therapy, resulting in poor clinical outcomes, which emphasises the unmet need for adequate therapy for a considerable portion of MR patients. This study may influence patient selection for TMVI in daily practice and sets the direction for future innovation.
Conflict of Interest statement
S. Ludwig reports non-financial support from Edwards Lifesciences. M. Seiffert reports non-financial support from Abbott Vascular, Biotronik, Boehringer Ingelheim, Boston Scientific, Edwards Lifesciences, Nicolai Medizintechnik, OrbusNeich Medical, personal fees from Abiomed, Amgen, AstraZeneca, Bayer Healthcare, Bristol-Myers Squibb, Boston Scientific, Medtronic, Philips and Shockwave Medical and grants from Philips. D. Westermann reports personal fees from AstraZeneca, Bayer, Berlin-Chemie and Novartis. S. Blankenberg reports grants and personal fees from Abbott Diagnostics, Bayer and Thermo Fisher, grants from Siemens and Singulex, and personal fees from Abbott, Amgen, Astra Zeneca, Medtronic, Novartis, Pfizer, Roche and Siemens Diagnostics, is a board member for DGK, and is UHZ Medical Director and a UHZ faculty member, all outside the submitted work. N. Schofer reports personal fees from Boston Scientific and non-financial support from Abbott and Edwards Lifesciences, outside the submitted work. E. Lubos received grants from Abbott and personal fees from Abbott, Abiomed, Astra Zeneca, Bayer, Edwards Lifesciences, New Valve Technology and Novartis. L. Conradi received personal fees from Edwards Lifesciences and is proctor and consultant for Abbott, Neovasc, Boston Scientific and Medtronic. D. Kalbacher reports personal fees from Abbott Vascular and Edwards Lifesciences and is a proctor for Edwards Lifesciences, receiving lecture as well as proctor fees and travel support, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.