Abstract
Informed consent is indispensable in contemporary medicine, especially in cases where the risks are high or there is true clinical equipoise, as in much invasive cardiology and cardiothoracic surgery practice. In this article we illustrate the principle of informed consent and describe how consent requirements have become more exacting in response to the rise of autonomy as the dominant principle in biomedical ethics. We outline some criticisms of informed consent, discuss why current requirements may never be achievable, and describe some of the vast literature aimed at “solving” the problem. We argue that respect for autonomy is just one of the principles of biomedical ethics and that the implementation of this principle must be weighed in the clinical context against the other principles, namely beneficence, non-maleficence and justice. The way we implement informed consent should be based on an ethical assessment of the clinical situation, including the invasiveness of the procedure, equipoise and the importance of patient values, and not on practical issues. We conclude that focusing on the whole decision-making process, effective communication, and a proportionate and individualised approach to consent could go some way to improve the experience of many patients in cardiology.
Introduction
The giving of consent to physical examination or treatment is fundamental to medical practice. It is among the most widely discussed issues in contemporary biomedical ethics, and is increasingly prominent in the cardiology literature. Informed consent requirements have become increasingly rigorous in parallel to the rise of autonomy as a dominant principle in biomedical ethics, and an array of legislation and guidance now demands informed consent that is ever more specific and explicit1. However, there are numerous obstacles to meeting these obligations. For example, they may be unachievable in emergency scenarios such as primary percutaneous coronary intervention (PCI), where cognitive impairment is commonplace. Indeed, given the complexity and rapidly progressive nature of best practice, even fully competent patients might have difficulty giving truly informed consent1. In this article we describe the principle of informed consent in everyday clinical practice, rehearse the criticisms of informed consent as it is currently understood, and present an assortment of novel attempts that have been proposed to improve the process. However, it is argued that the gap between the requirement that consent is fully specific and fully explicit and what is realistically achievable persists. It should be acknowledged that to bridge this gap requires revision of existing legislation and guidelines. Nonetheless, the cardiology and cardiothoracic surgical community could improve the situation by focusing on effective communication, and a proportionate and individualised approach to consent, especially where true equipoise exists.
The principle of informed consent
The growing prominence of informed consent has mirrored the rise of autonomy as the most important of Beauchamp and Childress’ four principles of biomedical ethics2, such that it has served as bedrock to numerous developments in medicine and the law. Informed consent requirements now permeate through statute, common law and guidelines. Requirements for valid consent are that the patient should have sufficient understanding, that sufficient information be given about the proposed treatment, and that any decision should be made free from duress (Figure 1)3.
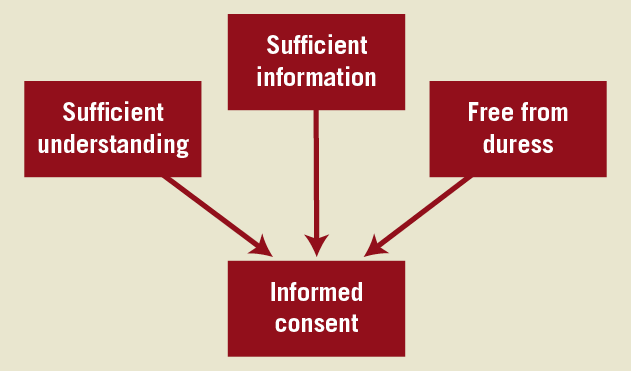
Figure 1. Essential requirements of valid informed consent.
The sufficient understanding element is also known as mental capacity, which is defined in the UK by the Mental Capacity Act 2005 as the degree to which a person is able to make a decision4. It describes situations in which a person may be considered to lack capacity, clarifies who can make decisions on their behalf, and how such decisions must be made. According to the Act, a person is unable to make a decision for himself unless he is able to understand the information relevant to the decision, retain the information, use or weigh that information as part of the process of making the decision, or to communicate his decision4.
The sufficient information requirement has largely been defined by the Bolam test, whereby, as originally described, “a doctor is not guilty of negligence if he has acted in accordance with a practice accepted as proper by a responsible body of medical men skilled in that particular art” (Bolam v Friern Hospital Management Committee [1957] 1 WLR 582 [McNair J]). While originally describing a best interests test, the Bolam principle has also been applied to patient information in Sidaway v Board of Governors of the Bethlem Royal Hospital and the Maudsley Hospital and Others [1985] 1 AC 871 (Diplock), among others. Subsequent cases have moved towards a “prudent patient” standard, defining risks that should be explained to patients as those that would affect the judgement of a reasonable patient (Pearce v United Bristol Healthcare NHS Trust [1999] PIQR P53, CA [Lord Woolf MR, Roch and Mummery LJ]).
For doctors practising in the UK these legal provisions have informed guidelines from the Department of Health, who begin by asserting that “It is a general legal and ethical principle that valid consent must be obtained before starting treatment or physical investigation, or providing personal care, for a person”5. This is echoed by the General Medical Council, as well as by various specialist societies, including the Society for Cardiothoracic Surgeons of Great Britain and Ireland, the European Society of Cardiology and the European Association for Cardio-Thoracic Surgery6,7.
In response to autonomy becoming the pre-eminent principle in medical ethics, and in response to increasing recognition of informed consent in the law and specialty guidance, informed consent requirements have become increasingly rigorous. Such “improvements” are aimed at making consent more specific and more explicit1. For example, consent forms have become increasingly complex, detailed and lengthy, including more and more risks. However, given the increasing complexity of cardiology and cardiothoracic surgery interventions, such rigorous consent may be unachievable.
Problems with informed consent
Informed consent practice frequently fails to meet these specific and explicit standards due to problems that may be considered under the headings of sufficient understanding, sufficient information and freedom from duress (Figure 2). All such impediments are exacerbated by any failure in standards of communication. Such failures include poor communication skills, impaired hearing, language barriers, and time-limited discussions of the risks and benefits of a procedure. In addition, non-specific consent taken prior to the procedure (“diagnostic angiogram query proceed”) fails to take into account lesion-specific risks as the anatomy is not yet known. Moreover, the operator may feel instinctively inclined to intervene on discovering a lesion without taking into account the full body of evidence and overall clinical picture. Therefore this process has clear limitations and does not constitute true consent.
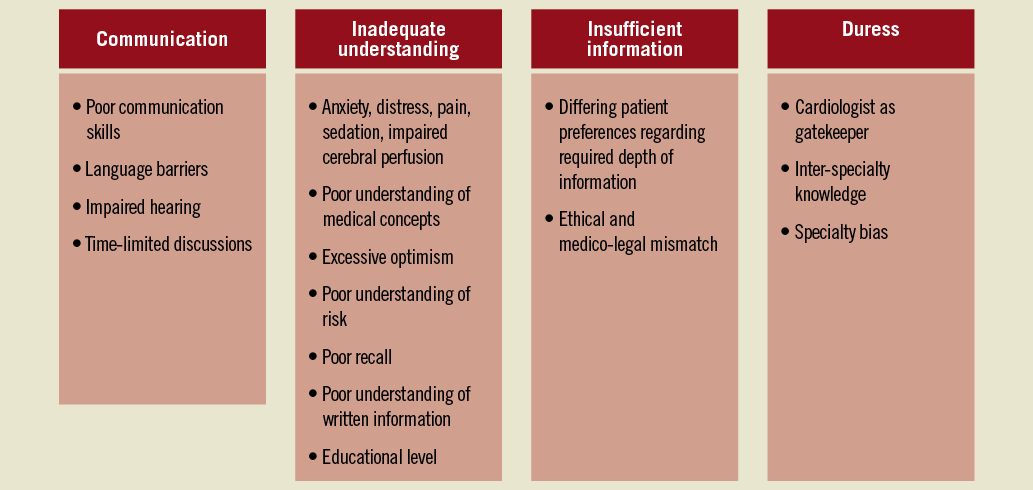
Figure 2. Reasons for failure of consent in PCI.
Sufficient understanding
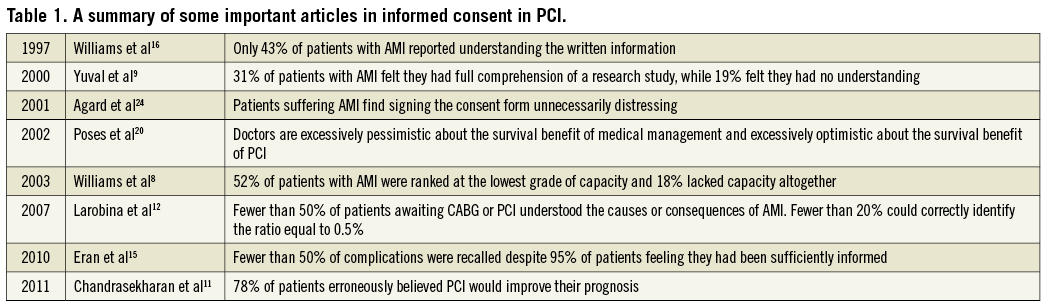
The difficulty in ensuring sufficient understanding is most starkly demonstrated in the context of emergencies. For example, many patients who require PCI lack sufficient capacity, for a variety of reasons, and therefore whether or not patients suffering acute myocardial infarction (AMI) are able to provide valid consent to primary PCI remains controversial. There are a number of potential obstacles to informed consent in the context of AMI. They include anxiety, distress, pain, the administration of sedation or opiates, and impaired cerebral perfusion. Williams et al prospectively studied 399 patients with AMI who were eligible for participation in the HERO-2 trial, and found that 75 of 145 (52%) were ranked at the lowest grade of capacity and 26 (18%) lacked capacity8. Similarly, in the research trial arena, Yuval et al found that only 31% of 129 patients who took part in the ISIS-4 trial perceived that they had full comprehension of the trial, while 19% felt that they had no understanding9. It is also apparent that doctors are bad at judging which patients have capacity. Smithline et al comprehensively evaluated patients’ ability to make informed decisions and, in addition to finding that patients’ cognitive abilities are temporarily affected in the acute phase, they demonstrated that physicians tend to overestimate the number of competent patients10. It became apparent when they adopted the Wechsler Adult Intelligence Scale to assess cognitive ability in AMI, a test that takes approximately 30 minutes in its abbreviated form10. Add to this a constantly evolving cardiology and cardiothoracic surgery literature and increasingly complicated and cognitively demanding interventions, and the result is that appropriate informed consent is only rarely achieved. It is not surprising, therefore, that some institutions may wish to adopt a system that utilises “assent”, a truncated form of the desired consent process. This may be justified on the premise that they act in the patient’s best interest but a key criticism of this process is that it can be interpreted as a slippery slope to paternalism.
In the elective setting it is evident that patients undergoing either coronary artery bypass grafting (CABG) or PCI have a poor understanding of medical concepts11,12. For example, it has been reported that fewer than 50% of such patients understand the causes or consequences of an AMI or stroke12. Similarly, it has been argued that patients are excessively optimistic about the benefits of their procedure, particularly where PCI is concerned12. For example, Chandrasekharan reviewed observational studies of patient understanding and perceptions of coronary revascularisation and found that 78% of patients believed PCI would improve their prognosis (the COURAGE trial concluded that no prognostic benefit is achieved by revascularising patients with stable angina, especially if ischaemia has not been induced, and outside the context of an ACS)11,13. In one such study, nearly a third of patients anticipated survival benefit even when they acknowledged their physician had not claimed this14. It is also suggested that many patients have poor understanding of risk. Larobina et al found that fewer than 20% of patients could correctly identify the ratio equal to 0.5%12. Use of such values is likely to prove difficult for patients with low numeracy skills. Finally, it is clear that patient recall is limited, even when information provision is adequate. For example, a prospective cohort study showed that fewer than 50% of potential complications were remembered despite 95% of patients feeling they had been sufficiently informed15.
Written information is also poorly understood. For example, only 43% of patients reported understanding the written information at the time of consenting to the HERO-2 trial16. A similar finding has been demonstrated in the stable setting, whereby the provision of written information made little difference to patient understanding17. In addition, comprehension is impaired by the mismatch between patient educational level and what is required by most information sheets and consent forms8,18,19.
Inadequate understanding is not limited to patients. Conference delegates were surveyed regarding the survival probability for medically managed patients with coronary artery disease, and the potential mortality benefit of CABG or PCI in such patients. The study demonstrated excessive pessimism regarding the survival of medically managed patients, and excessive optimism regarding the mortality benefit of revascularisation20. Further, Larobina et al identified that medical staff showed a poor knowledge of the concepts of material risk and medical negligence12.
Sufficient information
There are several problems with the sufficient information requirement for valid informed consent, which can be thought of as failure to provide information in line with the Joint 2010 ESC-EACTS Guidelines on Myocardial Revascularisation principles. These state that information should be “objective and unbiased, patient-orientated, evidence-based, up-to-date, reliable, understandable, accessible, transparent, relevant and consistent with statutory information”7. For example, it is not clear how much information patients should be given. Several studies have shown that patients want to be informed of all risks12,21,22, while many do not wish to be fully, or even partly, informed, and complain of information overload23. It is commonplace for patients to waive the informed consent process (“Do whatever you think, Doctor, I am in your hands”).
The trend has been to provide ever increasing information on risks and proposed benefits of a procedure, often via increasingly complex consent forms. For example, recent research work has advocated the use of consent forms that explicitly discuss risks18. However, consent forms can be a source of considerable distress, especially in AMI. For example, Agard et al surveyed patients suffering AMI and found a number of problems associated with written informed consent, especially in relation to the requirement to sign the form during the acute phase (one participant commented “I consider it unnecessarily brutal to put a paper under your nose when you don’t even know where you are. You can’t really make any decisions. That detail (the signing) is unnecessary, ethically incorrect.”)24. In addition, many institutions use consent forms that are generic and can therefore never be fully specific or explicit.
It is likely that contemporary informed consent demands continue to become formalised and protocolised, not in an attempt to improve standards but rather to avoid litigation25. However, the signing of a complicated consent form does not provide evidence of adequate informed consent procedures nor adequate communication. It is therefore debatable whether consent forms, as they are currently used, provide satisfactory legal weight when they fail to prove a consent process that generates sufficient understanding, provides sufficient information and is free from duress.
Free from duress
While it is not credible that doctors would exert undue influence on patients, it is noteworthy that the role of cardiologists as gatekeepers may introduce bias. In contemporary practice most patients see a cardiologist before they are discussed with a cardio-thoracic surgeon. Taggart points out that this means options for PCI are likely to be considered before surgery, and patients may not be given sufficient information or offered potentially more effective alternative therapies11. For example, they found that, for patients undergoing PCI, 65% were offered lifestyle modifications, 18-50% were offered medical therapy, and 13-15% were offered CABG11. Conversely, for patients undergoing CABG, 60% were offered lifestyle modifications, 44% medical therapy, and 64% PCI11. In addition, cardiologists may not be familiar with recent advances, evidence and techniques in cardio-thoracic practice, and so too surgeons may not be aware of new percutaneous techniques. This all confounds any attempt to supply the specific and explicit information that is required of contemporary biomedical practice. (Table 1)
Improving informed consent
There are three theoretical approaches to bridging the gap between genuine, ethically valid informed consent and the reality in many institutions, where many of the problems outlined above obstruct the process26. The first of these is to ignore the obvious deficiencies and proceed on the present course, conscious of the fact that much informed consent is perfunctory. This is clearly undesirable. The second, and preferred option, is to review and revise informed consent procedures to make them feasible, achievable, proportionate and justified. However, this would necessitate collaboration between judicial bodies, governing bodies, specialist societies and many more stakeholders, and does not appear imminent. The third approach is to attempt to improve the process in order to meet specific and explicit contemporary requirements. This would require far more rigorous informed consent protocols than currently exist in most centres, and even then may prove impossible. As a minimum, it would require classifying far more patients as lacking capacity than is currently the case1. Nonetheless, a plethora of novel solutions have been proposed to improve informed consent, many of which have narrowed, although not obliterated, the gap (Table 2).
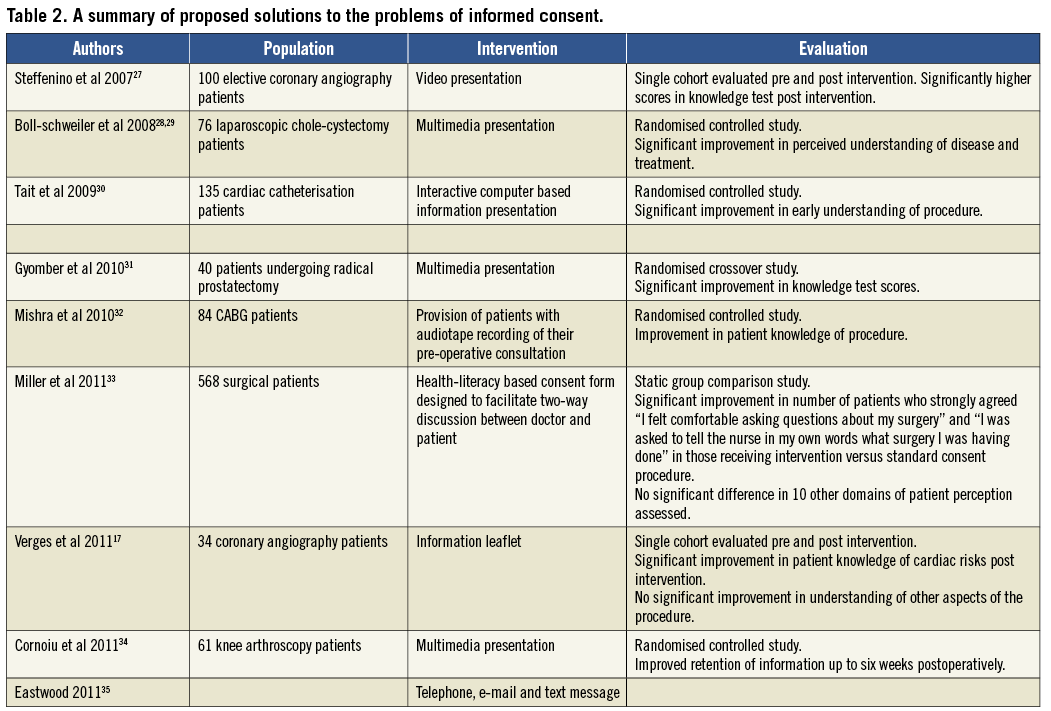
The evidence from these studies is limited by lack of blinding (particularly where the measured outcome is patient perception as opposed to knowledge), relatively small numbers and potential publication bias. Evaluation of the effectiveness of these new consent methods is clearly challenging: for example, assessing patient perception of their understanding does not necessarily equate to their actual understanding of the risks and benefits per se. Testing patient knowledge may indicate their level of understanding of the generic process, benefits and risks of the procedure in question, but does not necessarily indicate the quality of the decision-making process – for example, the level of risk specific to their unique clinical situation, and consideration of the alternative treatment options.
An alternative approach which has been evaluated in a recent systematic Cochrane review is the use of patient decision aids36. These are defined as “evidence-based tools designed to prepare clients to participate in making specific and deliberate choices among healthcare options”. They provide information regarding the health condition and treatment options, including benefits, risks and uncertainties of each, help the patient recognise the value-sensitive nature of the decision, and provide a structured framework for the decision-making process. In this systematic review, patient decision aids were associated with improved knowledge of treatment options and risks, reduced decisional conflict related to feeling uninformed and unclear about personal values, and more active involvement of patients in the decision-making process. There was variable effect on duration of consultation. Focusing on the whole decision-making process as opposed to the pure facts, and adopting a more individualised approach in this manner could potentially enhance the practice of obtaining informed consent.
In addition, a number of novel approaches have been tried in emergency research studies, and may contain lessons for clinical practice. For example, in the Corticosteroid Randomisation After Significant Head injury 1 (CRASH 1) trial, the study cohort were unable to consent to participation so the investigators used a consent waiver and informed patients and relatives afterwards37. Of 10,008 randomised patients, only one withdrew consent38. It has been argued that waiving consent could reduce time to treatment39. However, such an approach has no utility for conscious patients with AMI who, even if there is diminished capacity, need to be involved in the decision-making process. Other suggestions include community consultation on appropriate means of obtaining consent40, consultation of patient groups41, prospective informed consent in high-risk groups42, and continuous consent, whereby information is given gradually over a period of time43.
Finally, multidisciplinary decision making by a clinical/non-invasive cardiologist, a cardiac surgeon and an interventional cardiologist (the Heart Team) has been advocated44. This ensures that all treatment options are considered and discussed with the patient prior to a decision being made, and guards against unintentional bias.
Efforts to improve the informed consent process should be commended. However, it must also be acknowledged that they are unlikely to satisfy contemporary informed consent requirements (that are fully explicit and fully specific). After Manson’s excellent “Rethinking Informed Consent in Bioethics”, we assert that the key to ensuring effective informed consent is excellent communication1. He defines effective communication as being intelligible, relevant and adequately accurate, and it is unsurprising, he asserts, that, if consent is seen merely as the disclosure of increasingly specific and explicit information, it frequently fails1. Several studies of consent in the acute setting have shown that oral information is preferable to written information. For example, Williams et al found that only 18% of patients read the information sheet before giving or refusing consent to their participation in an acute myocardial infarction trial8 and Schats et al found this figure to be 9% in clinical trials in subarachnoid haemorrhage45. Yuval et al found that 95% of patients recalled receiving the oral information, whereas only 37% recalled receiving the written consent form9. Further, better comprehension of the information was related to a reported duration of more than 5 minutes and an opportunity for discussion at the time of consent9. Agard et al found that 84% of patients would prefer to receive only oral information24. Improving communication is therefore central to any attempt to improve informed consent. Indeed, as most patients consent, or otherwise, on the basis of oral information alone, special attention should be paid to this, including improved formal training and supervision. This might be facilitated, for example, by expanding the role of pre-assessment clinics and allowing sufficient time for the informed consent process. Further, it may be constructive to replace complex and arbitrary consent forms with documentary evidence of satisfactory communication. Such documentation could also conceivably have a role in the assessment and revalidation of doctors.
Nonetheless, it is impossible to ignore exacting legal requirements in contemporary practice and therefore some form of documentary evidence is still required. Manson advocates that these standards be more demanding under certain circumstances1:
“A doctor who offers a diagnosis and proposal for treatment in simplified language does not seek, and will not receive, highly specific consent to the proposed treatment: but this may be acceptable provided that the treatment does not deceive or manipulate the patient, and the subsequent treatment does not force or coerce. More demanding standards may be relevant where the treatment is less well understood, where going ahead without consent would violate important norms and where the risks are high.”
We may demonstrate this with some examples. The taking of blood is relatively uncontroversial, and it is reasonable that informed consent demands are less onerous for such procedures. It would be considered nonsensical to require fully explicit and fully specific consent for phlebotomy under normal circumstances. It is proportionate, however, to expect a more rigorous process in the case of complex surgery. So too in the case of diagnostic angiography versus PCI, where the latter should mandate more thorough informed consent procedures. Likewise, in cases where the treatment is less well understood it is essential that informed consent aspires to be more specific and explicit than might be the case otherwise. Thus, for procedures where the risks are minimal and in emergencies, some ethical requirements of informed consent could correctly be waived, without attracting paternalistic criticism, providing excellent standards of communication are upheld. In contrast, in cases where ample time is available, where the risks are high or where there is true clinical equipoise, it is proper that more stringent processes and documentation are upheld. It is therefore important to highlight scenarios in cardiology where this is the case, and recognise the role for informed consent in contemporary practice.
Equipoise in contemporary cardiology
It is clear that true informed consent is complicated by controversies in best practice. For example, the best strategy for PCI in left main stem (LMS) disease or complex three-vessel disease has yet to be ascertained. Decision making in these patients is a challenge and is often not helped by the myriad of data that is available at any one time. Data is continually being reassessed and improved and many interventionalists and surgeons do not have sufficient time to synthesise this in order to make a reasoned judgement. To improve this, studies such as SYNTAX have been beneficial but comparative outcome data is currently limited to three years. In addition, such studies often do not take into account patient comorbidities and hence it is difficult to appreciate the true risk. In order for consent to be specific and explicit, the risk needs to be accurately quantified. This is a fundamental problem in cardiac intervention. The surgical community has addressed this through their EuroSCORE and Parsonnet scores. It seems plausible that a marriage between anatomical risk stratification and comorbidity is crucial to improve risk stratification for consent. To this endeavour, preliminary attempts have been made with the clinical SYNTAX score but this should be validated on a larger scale.
Whereas with SYNTAX there is a collaborative approach between cardiologists and surgeons, no such consensus exists for lesions that are classed as type C, such as bifurcations, calcified vessels, tortuous anatomy and chronic total occlusions. In Europe, bodies of experts such as the CTO Club and European Bifurcation Club may evaluate the latest data, but the resulting consensus is not always communicated effectively to practising cardiologists who are making these decisions and to consenting patients on a daily basis. This is confounded by the fact that new technologies and techniques are constantly evolving and hence it is difficult to keep abreast of constantly changing data. Moreover, there is a lack of surgical representation in these societies. It is important that the potential of these societies to improve the consent process is recognised, with particular emphasis on the lesion subtype and taking into account all evolving, contemporary data. A novel approach may be to develop a lesion-specific electronically-based consent form endorsed and annually updated by these bodies of experts.
Some suggestions
For these situations a more specific and explicit approach is appropriate, while acknowledging the value of effective communication. Such an approach should also be individualised to avoid the many pitfalls with generic consent outlined above. The increasing use of risk scores in cardiology is a promising avenue for improving informed consent that is illuminated by emerging evidence and registry data. A number of contemporary and evolving algorithms are described by Farooq et al, including models that incorporate patients’ personal perceptions of the risks-benefit trade-off46. They describe work by Federspiel et al that validated the quantification of the level of risk that a patient would be willing to accept to maintain their present functional state46,47. Such patient-centred models have important implications for improving informed consent.
Indeed, Arnold et al have developed an internet-based programme designed to insert patient-specific outcomes of death, bleeding and restenosis into individualised informed consent documents48. Single-centre outcomes in the USA following the use of patient-specific risks were very positive, demonstrating improved participation, reduced anxiety, and better risk recall. This approach could feasibly be extended to local populations with the use of registry data and cohort-specific risk scores. It could also incorporate institutional (and operator?) success, and be presented to patients in a range of formats (hard copy, website or smart phone application, for example).
Conclusions
The shift from paternalism to autonomy in bioethics has heralded increasingly stringent models of informed consent. This usually manifests itself by way of ever more complex consent forms. However, while this serves to protect healthcare institutions from litigation, it does not ensure adequate informed consent. This is especially true for complex PCI where the cognitive infirmity of many patients renders existing processes obsolete. Rather, we have championed effective communication that is not littered with jargon. Indeed, where procedures are uncontroversial, we have questioned the value of contemporary consent forms, preferring instead documented evidence of satisfactory communication. Rather than asking patients to acknowledge every single possible risk, we would prefer patient information to be individualised, to incorporate risk algorithms and be more universally available. This should serve as an adjunct to effective communication, and should not serve to increase further the complexity of consent forms. Of course, a role remains for consent forms where specific and explicit information is necessary (in high risk, novel or non-evidence-based procedures); however, these should be proportionate and accessible. Further work is required to achieve a balance between medico-legal protection for institutions and not detracting from excellence in communication with arbitrary consent forms.
Conflict of interest statement
The authors have no conflict of interest to declare.

