Dear colleagues
If you search on the website of NBC under the item “health”, you will find the following statements:
“Millions of Americans could be walking around with tiny time bombs in their hearts”
“By one estimate, the devices already kill 2000 Americans a year and no one knows what the long-term damage will be...”
“DES manufacturers Boston Scientific and Johnson & Johnson could end up rivalling VIOXX maker Merck as targets of lawsuits from people who suffer heart attacks.”
These three statements illustrate the DES thrombosis hysteria in the American lay media. Something similar was presented in passing in the European media. The specific studies that have prompted these media reports were the BASKET – late study (presented at the March 2006 American College of Cardiology’s annual scientific session in Atlanta, GA) and more recently, the Camenzind meta-analysis (presented at the September 2006 European Society of Cardiology/ World Congress of Cardiology meeting in Barcelona, Spain). A small but significant increase in death rate and myocardial infarction observed in these studies was noted in patients followed 18 months to 3 years after stent implantation.
The FDA met with the two manufacturers of DES to discuss any information they might have pertaining to the issue of stent thrombosis. They also requested that the two companies reassess the stent thrombosis rates in their respective trials based on a set of broad definitions recently established by a consortium of academic researchers who, in the spring and early summer of 2006, agreed on a series of definitions of clinical end points in relation to stent trials. The FDA also decided to convene a public panel of outside scientific experts to assist them in a thorough review of all data, making recommendations about what actions might be appropriate such as possible labelling changes or additional studies (FDA home page, updated December 7, 2006).
On December 7th and 8th 2006, in a packed hotel ballroom in Gaithersburg, Maryland, USA, the 21 member Food and Drug Administration panel listened to presentations from the two manufacturers and from researchers from the USA, Europe and Japan (these included Takeshi Kimura, Lars Wallentin, Adnan Kastrati, Antonio Colombo, myself, Gerrit-Anne van ES, etc.) who analysed the latest data from the large registries of patients who received these stents since they were introduced three years ago.
By the end of the first day, panel members agreed that – at least for on-label indications – DES appears to increase the risk of late stent thrombosis, but not the risk of death or MI. When asking questions to the panel, the chair urged them to clearly answer yes or no before adding their comments – and unanimously they all answered “no”. Interviewed by HeartWire, I said, “...that one word “no” was the critical moment in the day. If the panel had come to a statement
that DES increases the risk of death or of MI it would have been a dramatic day. But unanimously, they said no. It ranged from the ‘Hell No!!’ of Christopher White, to the ‘No, but’ of Steven Nissen, but it was an unanimous no, nonetheless. And I think that’s an important message for the community.”
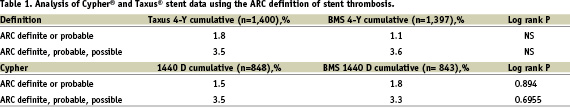
On day one, the presentations of both the Cypher stent data and Taxus stent data were analysed using the Academic Research Consortium (ARC) definition of stent thrombosis which showed no increased risk of stent thrombosis for either of these drug eluting stents when compared with bare metal stents (Table 1).
There was some reluctance from the members of the panel to accept the definition and the process through which they were generated. Again interviewed by the press, I personally voiced my irritation “to hear the ARC definition criticised”. “Okay,” I said, “so they were not created according to the process of the ACC or the AHA, but those two organisations didn’t attempt to do this in the first place! The point is not the definition, the point is the consensus. And we were so pleased to have the five major industry representatives around the table, as well as doctors from both sides of the Atlantic, and the FDA saying it is a good move. So to hear them say that due process was not followed, that was very irritating.”
For the rest of the first day the panel wrestled with the question of dual antiplatelet therapy. On Thursday (the first day of the conference) the panel said that those healthier “on-label” patients could be on therapy for three to six months as the stent labels recommended. But ultimately, on Friday (the second day) the panel endorsed the current ACC/AHA/SACI /ESC guidelines for PCI that recommended “ideally” extending dual anti-platelet therapy to 12 months in patients who have a low risk of bleeding in the so called “off-label” group.
On day two, the FDA panel warned against increased risk of death/MI/stent thrombosis with “off-label” DES use, but it also said that higher complication rates should be expected, and while it was concerned about widespread use of drug eluting stents in patients that these devices are not approved for, there doesn’t exist enough evidence to recommend restricting their use.
As stated by Dr. Bram Zuckerman for the FDA office of device evaluation at the end of the two days of deliberation, “it is not our usual structure to extensively regulate the practices of medicine, the relationship between the patient and the physician and their choice of devices used is something that we don’t want to tamper with. But when there is a significant health problem, the FDA and health and human services cannot ignore it. In our two days of deliberations, we have heard that there are signals that need to be very seriously looked at.”
Finally, the panel agreed that there needs to be larger and longer studies that would specifically look for the risk of stent thrombosis. Studies on the direction of dual antiplatelet therapy are also urgently needed. Some members suggested that future trials – and even future registries – that investigate the use of DES in multi-vessel disease must have, as point of comparison, an arm of CABG treated populations.