Abstract
Aims: Recanalisation rates of coronary chronic total occlusions (CTO) remain sub-optimal. The retrograde technique was recently introduced to improve success rates.
Methods and results: From February 2005 until December 2007, 175 patients were treated with this technique in seven European centres by highly experienced operators: in 84 (48%) as primary strategy, in 41 (23.5%) immediately after antegrade failure and in 50 (28.5%) as a repeat procedure after previous antegrade failure.
Baseline characteristics revealed a mean age 61.4±10.8 years with 29.5% and 39% of patients having diabetes and a prior history of MI, respectively. The mean occlusion duration was 50.8 months (determined in 32% of patients). The target vessel was: LAD 21%, LCX 6.3%, RCA 71.4%. Epicardial collaterals were accessed in 20.6% and septal in 79.4% of the patients. Overall success rate was 83.4%. In 80.6% a wire crossed the collaterals and successfully delivered distal to the occlusion; success rate in this group was 91.5%. The technique implemented in the retrograde facilitated successful recanalisation was: retrograde wire/balloon crossing in 28%, CART in 34% and marker wire/“knuckle” technique in 48%. There was a great diversity between centres referring to the retrograde technique used. According to the initial strategy success rates were: primary 89.3%, immediately after antegrade failure 65.9% and repeat procedure after antegrade failure in 88%. In patients with failure to cross the collaterals success rate was 50%.
Septal rupture/haematoma occurred in 6.9% of the patients, periprocedural myocardial infarction (CK-MB rise) in 4% and TIA in 0.6% and wire entrapment in 0.6%. Mean fluoroscopy time was 59.3 mn and the mean contrast used was 420.9 ml. Drug eluting stents were implanted in all successfully recanalised vessels.
Conclusions: There is great diversity amongst European centres with respect to how the retrograde strategy has been adopted and adapted. The retrograde approach was used with high degree of success and safety and can thus be regarded as a valid contributor to the armamentarium of the modern day interventional cardiologist.
Introduction
Coronary chronic total occlusions (CTO) are identified in one third of patients undergoing diagnostic coronary angiography,1 with the incidence increasing with age.2 When indicated, successful recanalisation of a CTO is associated with a reduction in the future need for coronary artery bypass graft surgery (CABG)3, improvement in anginal status4 and left ventricular function5, as well as long-term survival.6,7 Despite these benefits, a recent analysis from the NHLBI database showed a decrease in the number of attempted percutaneous coronary intervention (PCI) procedures to CTOs from 9.4 to 5.7% between 1997 to 20048 highlighting the fact that CTO angioplasty is complex, requires familiarity with new equipment and techniques and is associated with increased patient and operator radiation exposure.9 Moreover, success rates for treating CTOs with conventional techniques have remained unchanged over time6,7,10-12 averaging 65-70% in experienced hands, well below the standard for non-occlusive coronary lesions.
Various dedicated devices for CTO treatment have failed to improve success rates in routine clinical use13-15 and currently are only indicated for specific anatomical situations. Cornerstones in the task of improving recanalisation rates have been the dual injection for visualisation of the vascular bed distal from the occlusion, the parallel wire technique and the dramatic improvements in dedicated CTO wires, over-the-wire balloons and micro-catheters, as well as the development of dedicated groups of experts focusing technical development, training and education worldwide. Furthermore, drug-eluting stents (DES) have allowed improved clinical outcomes with reduced target vessel failure compared to angioplasty or bare metal stents.16
One such technique, pioneered by our Japanese colleagues, encompasses accessing the retrograde collateral channels supplying the chronically occluded vessel. This remains distinctly different to the use of saphenous vein grafts, which is well described.1,17 These tiny collateral networks are now permitting successful CTO recanalisation,9,18-20 even immediately following an unsuccessful antegrade attempt which had resulted in considerable arterial dissection.21 This group of techniques, collectively embraced as the ‘retrograde approach’ to CTO recanalisation have helped re-focus attention on the benefits of successful CTO PCI and have led to enthusiastic uptake of the technique by European centres and operators in an attempt to improve the success rate of these complex occlusions. This multicentre study assessed patients treated using the retrograde approach for CTO recanalisation and aimed to examine the success rate and diversity amongst centres with respect to how the retrograde strategy has been adopted and adapted in clinical practice outside Japan.
Methods
Patient population
Patients from seven European centres undergoing CTO PCI, via the retrograde approach by highly experienced dedicated operators, performing at least 50 CTO procedures annually were included in this study. No clinical exclusion criteria were applied and patients with prior failed CTO PCI and those with a first CTO attempt were included, as long as the treatment strategy involved the retrograde approach. All patients were symptomatic and / or had evidence of viable myocardium/inducible ischaemia in the territory of distribution of the occluded vessel.
Definitions
Coronary CTOs were defined as thrombolysis in myocardial infarction (TIMI) grade 0 flow with a duration > 3 months, estimated from clinical events such as acute myocardial infarction in the same target vessel territory, sudden onset or worsening of the symptoms, or proven by previous angiography, or undetermined.17 Angiographic success was defined as restoration of TIMI flow grade 3 with stent implantation in the occluded segments and residual stenosis < 20% by visual estimate. Myocardial infarction (MI) was defined as > 3 fold increase of creatine-kinase MB. All patients were pretreated with aspirin and clopidogrel. Heparin was used to maintain an activated clotting time (ACT) > 300 seconds. Upstream use of glycoprotein IIb/IIIa inhibitor therapy or bivalirudin was avoided for the potential increased risk of bleeding in case of coronary perforation.
Quantitative coronary angiography
Quantitative coronary angiography (QCA) was performed using the Cardiovascular Angiography Analysis System II (CAAS II), Pie Medical, Maastricht, The Netherlands. The occlusion length was assessed from the beginning of the occlusion to distal antegrade or retrograde vessel filling from either bridging collaterals, non-target vessel collaterals or following simultaneous left and right coronary injection.
Retrograde techniques
CONTROLLED ANTEGRADE RETROGRADE SUB-INTIMAL TRACKING (CART) TECHNIQUE
The CART technique has been described in detail previously9,20 and involves the insertion of an antegrade wire advanced as far as possible beyond the proximal fibrous cap into the occlusion as well as a retrograde guidewire and balloon through collateral branches supplying chronically occluded vessels. A 6-8 Fr guiding catheter is positioned at the ostium of both the occluded and the donor vessel. A soft polymer-coated wire is used to engage the collateral which can be followed angiographically from the donor to the occluded vessel. The wire manipulation may or may not be directed by the acquisition of a sub-selective injection, via an over the wire microcatheter, used as a road map. After wire passage, dilatation with a 1.25 or 1.3 mm balloon at 2-4 atm in the collateral channel is performed and an OTW balloon with a diameter of 2.5 or 3.0 mm is advanced near the distal end of the occlusion and inflated at 3-6 atm to provide support to the attempts of retrograde wire probing. The soft hydrophilic wire may be replaced with a CTO dedicated wire, used to cross the occlusion from the distal true lumen. The retrograde wire is then advanced parallel to the antegrade wire that had been positioned subintimally to create a controlled subintimal dissection, by inflating the distal balloon at the level of the chronic occlusion. The antegrade wire is then advanced and steered subintimally towards the retrograde balloon to connect the two subintimal lumina. Wire advancement is followed in multiple angiographic views to ensure alignment. Following this, the antegrade wire can be advanced into the distal true lumen. When this enlargement of the channel is applied in an antegrade manner facilitating advancement of the retrograde wire to the proximal true lumen, the technique is named reverse CART. An example of the CART technique is depicted in Figure 1.
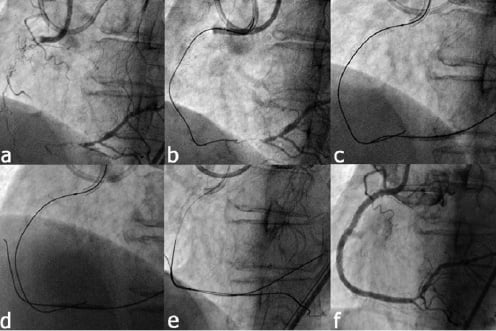
Figure 1. Illustration of the controlled antegrade retrograde subintimal tracking (CART) technique. a) Long, chronic occlusion of the right coronary artery. b) The antegrade wire is advance in the occluded segment but cannot reach the distal true lumen. c) After crossing and dilating the septal collateral, a balloon is inflated within the distal occluded segment. d) The subintimal flap/space created by retrograde balloon inflation is targeted by the antegrade wire with subsequent passage into the distal true lumen (e). f) Final result following drug-eluting stent implantation.
PURE RETROGRADE CROSSING TECHNIQUE
The procedure is the same as the CART technique, up to the point of reaching the distal cap. In this technique, the retrograde wire is advanced through the occlusion reaching the proximal true lumen and exiting in the ascending aorta or the antegrade guiding catheter where it can be trapped by inflating a balloon within the antegrade catheter to facilitate crossing of the occlusion with the retrograde balloon (retrograde wire trapping technique). At this point the retrograde balloon is advanced and inflated in the occlusion, re-establishing patency and allowing easy crossing of a soft wire antegradely. An example of the pure retrograde technique is depicted in Figure 2.
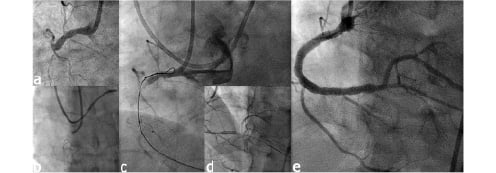
Figure 2. Illustration of the Knuckle wire technique. a) An occluded right coronary artery with blunt stump and bridging collaterals. b) A wire was advanced though the septal collateral up to the distal cap with formation of a loop at its distal end after penetration into the occlusion. c) Advancement of the wire through the entire length of the occlusion with creation of a dissection and large subintimal space which facilitates advancement of an antegrade wire through the occlusion (d). Due to absence of a connection with the proximal lumen and consequently absence of flow, there is no propagation of the dissection distally. e) Final result following drug-eluting stent implantation.
KNUCKLE TECHNIQUE
This is a variation of the CART technique, where the dissection of the subintimal space is created by the formation of a loop in the retrograde wire which is then advanced to the occluded segment. The principle is the same as the STAR technique22 from the antegrade approach with the benefit that there is no flow to propagate the dissection distally. Soft hydrophilic wires are preferable for this technique. The crossing and dilatation of the septal collaterals with a balloon is not mandatory although frequent. An example of the knuckle technique is depicted in Figure 3.
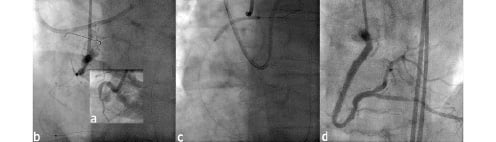
Figure 3. Illustration of the pure retrograde technique. a) An occlusion of the right coronary artery with presence of proximal tortuosity, blunt stump and presence of a large side branch. b) A retrograde wire was advanced through the septal collateral and successfully crossed the occlusion with its radiopaque tip visible in the ascending aorta. c) Dilatation of the occluded segment up to the ostium of the right coronary artery. Note the absence of an antegrade wire. d) Final result after antegrade crossing and drug-eluting stent implantation.
MARKER WIRE TECHNIQUE
After crossing the collateral, the wire is advanced up to the distal cap of the occlusion and is used solely as a marker without attempt to penetrate the occlusion retrogradely. It is the simplest embodiment of the retrograde techniques not requiring the crossing of the collaterals with a balloon and subsequent dilatation. Due to its relative simplicity, it is suggested as the technique of choice when embarking with the retrograde approach. An example of the marker wire technique is depicted in Figure 4.
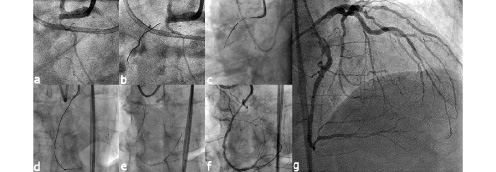
Figure 4. Illustration of the Marker wire technique. a) A proximally occluded right coronary artery. b) A soft, hydrophilic wire was advanced through the septal collateral and part of the occluded segment but could not reach the proximal true lumen. Attempts to cross and dilate the septal collateral channel with a balloon were also unsuccessful and the wire could not be exchanged for a dedicated CTO wire. c,d) The retrograde wire used as marker to guide antegrade wire crossing. e,f) Successful antegrade wire placement in the distal true lumen. g) Final result after completion of the intervention with drug eluting stent implantation. The septal collateral channel crossed is not visible since it was not dilated.
Statistical analysis
Descriptive analyses were used. Results are quoted as percentages for categorical data or as mean±standard deviation for continuous variables.
Results
Baseline clinical and lesion characteristics
From February 2005 until December of 2007, 175 patients underwent PCI for at least one CTO lesion using the retrograde approach in seven European centres. Baseline clinical and lesion characteristics are shown in Table 1.
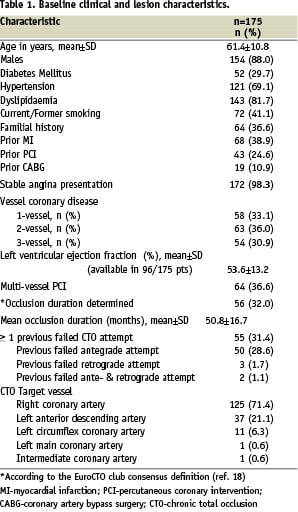
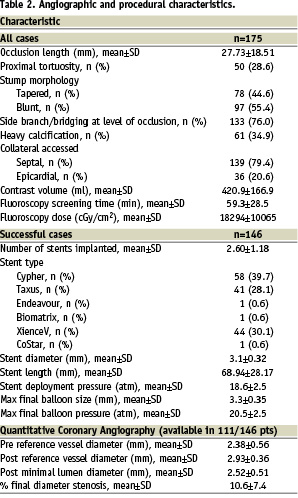
Mean age of patients was 61.4±10.8 years and 88% were males. One third of the patients had a previous unsuccessful CTO attempt. The majority of occlusions involved the right coronary artery (RCA, 71.4%) and the left anterior descending artery (LAD, 21.1%). The CTO lesions were calcified in over a third of patients with over half of all occlusions having blunt stump morphology. A side branch or bridging in close proximity to the occlusion was observed in over three quarters of cases. Septal collaterals were used to access the occlusion in 79.4% of cases, while an epicardial channel was used in the remaining 20.6%. The mean occlusion length was 27.73±18.51 mm. The occlusion duration could be determined in 32% of patients and was 50.8±16.7 months. The angiographic and procedural characteristics are presented in Table 2.
Treatment strategy
In 84 (48%) patients, a retrograde approach was the initial intended strategy (primary), while in 41 (23%) this was undertaken in the same session of an unsuccessful antegrade attempt. In the remaining 50 (29%) cases, the retrograde approach was a planned, elective procedure in patients with a previously failed conventional antegrade attempt and in whom a repeated antegrade approach was felt to be futile. There was great diversity among the centres as illustrated in Figure 5.
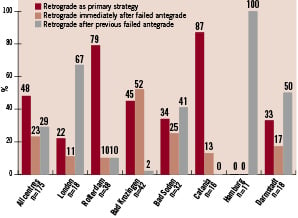
Figure 5. Overview of the retrograde strategy.
Procedural characteristics and outcomes
Overall success rate was 83.4%. In 80.6%, a wire crossed the collaterals and successfully reached the distal occluded vessel; the success rate in this group was 91.5%. Overall, the technique implemented in the retrograde facilitated successful recanalisation was: retrograde wire/balloon crossing in 28%, CART in 24% and “knuckle” technique in 48%; great diversity among the centres was observed (see Figure 6).
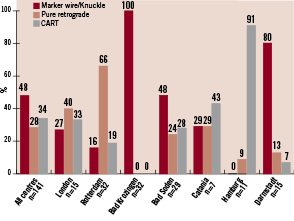
Figure 6. Overview of the retrograde technique in the retrograde facilitated cases.
According to the initial strategy, success rates were: 89% for primary, 66% for retrograde immediately after antegrade failure and 88% for repeat procedure after previous antegrade failure. After any antegrade failure, the success rate was 78%. In patients with failure to cross the collaterals, the success rate was 50%. Table 3 demonstrates the spectrum of guidewires used to both cross the collateral channel and then on to cross the occlusion.
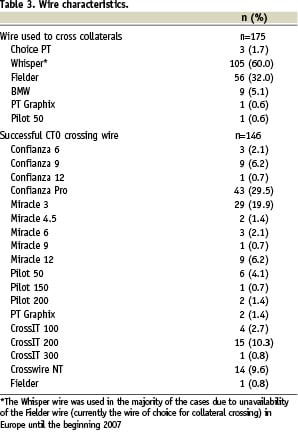
Table 4 lists the strategy used and the corresponding success rate.
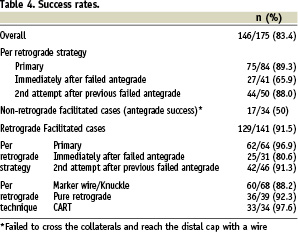
In all successful cases, DES were implanted with a mean stent length of 68.94±28.17 mm. The mean contrast volume used, fluoroscopic screening time and fluoroscopic radiation dose were 420.9±166.9ml, 59.3±28.5minutes and 18294±10065cGy/cm2, respectively.
Acute procedural complications and in-hospital outcomes are shown in Table 5.
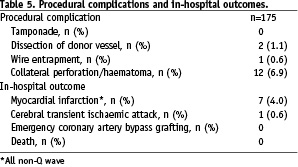
Septal rupture/haematoma occurred in 7% of the patients without clinical sequeale, periprocedural myocardial infarction (non-Q wave) in seven (4%) patients and transient ischaemic attack (TIA) in one (0.6%) patient. There were no cases of pericardial effusion requiring pericardiocentesis.
Discussion
This multicentre study has shown that the retrograde approach to CTO recanalisation can be applied to a large number of patients with a high degree of success and safety. Moreover, each dedicated European centre has adopted the technique in a different fashion, highlighting the great diversity that exists in clinical practice, namely with the particular strategy and equipment used. Nevertheless, using these novel techniques, the procedure can be applicable to a significant number of patients with coronary CTO and can therefore help improve the success rates of such complex lesions.
Previous small scale studies have shown that the retrograde approach is feasible9,20,23 however, interventional cardiologists have not been unanimous in their embrace of the technique, especially given its unique procedural requirements and the rather unaccustomed way to reach the occluded vessel. Nevertheless, exposure given by our Japanese colleagues during live case transmissions and congresses, together with their proctorship, have enabled a select group of European centres to adopt the retrograde techniques in their daily practice, therefore providing an alternative to surgery for symptomatic patients.
Indications for CTO recanalisation
The choice to engage in an often lengthy procedure is dependent upon the nature of the patient’s symptoms and evidence of reversible or viable myocardial ischaemia in the territory of the occluded vessel. Recent attention, particularly following the COURAGE trial24 has made many clinicians sceptical in performing any PCI, let alone a complex CTO procedure. Care must be taken however when interpreting such trial data in this highly specialised group of patients, especially given that such patients with CTO were not examined as part of the COURAGE trial. There is mounting evidence to support the benefits of a successful CTO procedure, both in the reduction of symptoms and need for invasive surgery and also in the reduction of hard clinical endpoints such as death and myocardial infarction.7,16,25
Techniques of retrograde recanalisation
The uptake of the retrograde approach amongst European centres has given a rather diverse picture about its implementation and adaptation. Differences were noted between centres as to the indications for such an approach, ranging from some centres performing the retrograde approach early on during a procedure, even as the initial strategy of choice, while other centres have adopted a more conservative approach, deferring it only to when a conventional CTO attempt is unsuccessful. Encouragingly however, centres have been able to introduce and excel in these highly specialised techniques using equipment readily available and licensed for clinical use in Europe. Most material specifically developed for retrograde approach is not yet available in Europe which is different than Japan where the pioneers are focussing on refined equipment to better handle the collateral channels e.g. with a tapered polymer wire (Fielder XT® Asahi Intec, Japan) or septal dilators and to improve retrograde wire manipulation, all currently not commercially available outside Japan. In our continent we have to accept 0.0014 soft polymer wires to select septal collaterals and small over-the-wire balloon catheters longer than 137 cm became available only recently.
As a rule of thumb, soft-tipped polymer wires are used to retrieve the retrograde collaterals and are positioned as a landmark for the kissing wires technique. Moderately stiff-tipped wires (e.g. Miracle 3-6 g) are preferred for retrograde penetration into the occlusion and stiff-tipped tapered wires (e.g., Confianza pro) for antegrade penetration. The latter wires are applied retrogradely only with great caution in order to avoid wire exit and disastrous perforation upon balloon inflation, which is a necessary step for the CART-technique.
In addition, changes in other procedural characteristics are becoming evident between centres inside and outside Japan. For example, European adoption has generally been to use smaller guiding catheter sizes compared to the 8 Fr sizes which are customary in Japan. Also, less intravascular ultrasound guidance is applied in Europe; however, this is a general feature in common to non-occlusive lesions as well. While Japanese experts tend to increasingly apply the reversed CART-technique, European operators so far have not adopted this variation.
Furthermore in Japan, preprocedural MSCT documentation of the occlusion length, tortuosity and calcification and the collaterals is gaining increasing attention and seems to be often used as an aid to decide if the procedure should be started in a retrograde fashion. According to our experience in Europe, MSCT is not used routinely before PCI of CTOs mainly because of costs, radiation exposure, and a lack of scientific data to demonstrate an advantage.
There was a profound difference in the success rates between patients in which a wire reached the distal cap compared to those in which there was failure to cross the collateral (91.5% vs. 50%). The latter is indicative of the complexity of the CTO in this cohort of patients and emphasises the contribution of the retrograde techniques in improving success rates in very complex CTOs.
An 88% success rate was achieved in patients with previous failed antegrade attempt. As the experience and the familiarity with the retrograde technique is increasing, the failure rates will decrease but it is important to keep in mind that it is worthwhile to refer patients after failed antegrade attempt to operators with large experience in the retrograde technique for a repeat procedure before considering surgery, especially when they are young or with single vessel disease or previous bypass surgery.
In patients without previous CTO failure, higher rates of success were observed when the retrograde approach was the primary strategy adopted compared to when this followed immediately after antegrade failure (89.3% versus 65.9% respectively). This was the case even in the retrograde facilitated cases (retrograde wire reached the distal cap) (96.9% versus 80.6% respectively). The operator/patient fatigue, contrast consumption or radiation exposure for the antegrade attempt may account for this outcome. In very complex CTOs, with expected low success rates, and in experienced hands it might be preferable to consider the retrograde approach as primary strategy but we are still far from considering it as a mainstream procedure for all CTOs.
In almost half the patients, the marker wire/knuckle technique was adopted with the CART and pure retrograde equally performed in the remaining patients. With all techniques, very high success rates were achieved. It is important to realise that there are no strict rules as to when to apply one or the other technique, and sometimes, their combination during the same procedure is mandatory to achieve a successful outcome. Regardless of the technique used, once the occlusion is crossed, clear evidence exists to support the implantation of DES which have considerably contributed to improved clinical outcomes, primarily as a result of significantly lower target vessel failure compared to angioplasty and bare metal stents, making DES the standard treatment for CTO PCI.16,26
Learning curve
The retrograde approach requires adequate proctorship and is not a technique to be tried without an already good foundation in CTO PCI via the customary antegrade approach. The dedicated materials and specialised guidewires require careful handling, particularly during the passage through the collateral channel. Here, the septal approach offers a distinct advantage to epicardial ones given that the septum appears to offer a remarkable resistance to wall damage and development of bleeding complications. Nevertheless, choosing the appropriate collateral is one of the main learning points with care to avoid tortuous and poorly visible networks. Regardless, the retrograde approach also has the potential to shorten the length of the stented segment because the subintimal track is limited to the occluded segment, except for the reverse CART-technique, and is unlikely to extend to a long segment distal to the occlusion as sometimes is experienced in the antegrade wiring techniques.27
Safety issues
As we have demonstrated, a high degree of procedural safety can be expected when the retrograde technique is performed by experienced operators. Nevertheless, there is a theoretical risk of catastrophic ischaemic complications upon injury, dissection or thrombotic occlusion of the collateral donating vessel. In our series we experienced 6.9% cases of septal perforation, all were contained and none resulted in any pericardial fluid collection. It should be mentioned, however, that there might be a considerable risk of disastrous perforations mainly of epicardial collaterals that will require immediate embolisation with coils. PCI for CTO in general is complex and generally a long procedure. Additionally, they demand higher volumes of contrast, particularly given the use of two guiding catheters with a double simultaneous injection to help visualise the septal channel and appropriate path to the distal occluded segment. None of the patients had a post-procedure creatinine rise but in patients with renal impairment, generous periprocedural hydration, acetyl-cysteine administration, and use of iso-osmolar contrast are recommended. Although this study did not compare the antegrade and retrograde approaches, contrast can be minimised by the retrograde approach as a wire positioned in the distal occluded segment is often enough to help guide passage into the true lumen.
The radiation exposure was higher than that typically observed in PCI of non-occluded vessels, however comparable with historical data for the antegrade approach.9 The potential benefits of an extensive attempt at CTO recanalisation with high chances for success must always be balanced with the possible risks involved in such a procedure.
Conclusions
There is still a great diversity amongst centres with respect to how the retrograde strategy has been adopted and adapted in Europe; however, a high degree of success can be expected in the hands of highly experienced CTO-operators. The approach is technically demanding though, with a steep learning curve. While experienced operators with a high volume of CTO-procedures should be encouraged to eventually implement the technique in routine clinical practice, especially after antegrade failure in patients with strong retrograde collateralisation, we strongly recommend not viewing the retrograde technique as a compensation for a lack of extensive experience to open CTO in a sophisticated antegrade manner.

