And here we are again, at the beginning of what is now our traditional special issue of EuroIntervention, coinciding with the long-awaited return – after two years of a solely digital existence – of our in-person EuroPCR.
It’s worthless to discuss what all this means for the interventional community, as it is so obvious to us all, but I would like to point out that after the recent scientific session of the American College of Cardiology, EuroPCR has also chosen the path of a “hybrid” transition: a path made up of content that can only be used in person and other content dedicated to virtual attendees.
The digital revolution, boosted by the pandemic, has brought us to this point; the event remains the same, but it can be attended in different ways, namely at the Palais des Congrès in Paris or from the comfort of your own home. Like a football match that you can see either at the stadium or from the sofa in your own living room, each way you participate comes with different emotions, but both can be satisfying. Overall, this means expanding the audience and breaking down distances in a way we would never have thought possible not so many years ago.
This year EuroPCR will feature a 4-day Course taking place in 21 session rooms, including 3 TV studios, and will feature more than 290 educational sessions, more than 400 hours of programme content and the return of real-time live cases.
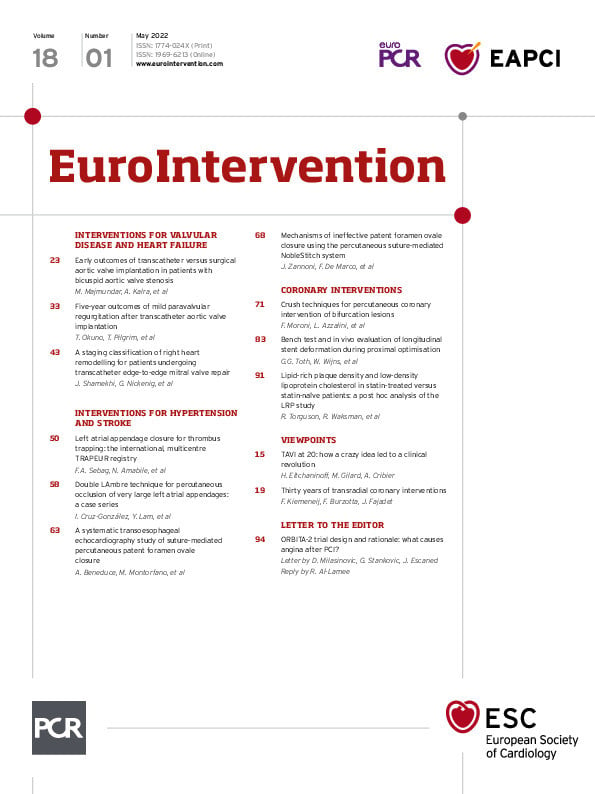
EuroIntervention will, as always, do its part to best represent the academic and practical vocation of our readers and the community they represent. So, here’s what awaits you in this issue (and also take a look at the ahead-of-print simultaneous publications at the time of the Course, where you will find quite a few surprises).
We begin this issue with two viewpoints that capture important moments in the history of interventional cardiology. In the first of these, Hélène Eltchaninoff, Martine Gilard and Alain Cribier, essential players in the story itself, lead us through the saga that preceded the first successful transcatheter aortic valve implantation (TAVI) 20 years ago this spring with all the elements that turned the almost dead-end drama of treating aortic stenosis in the very frail into a clinical solution and the dynamic field of valvular and structural disease we know today. The second viewpoint, by authors Ferdinand Kiemeneij, Francesco Burzotta and Jean Fajadet tell us about the 30 years in the development of the radial artery as an access point in coronary interventions.
Following the last viewpoint, the first clinical research article is on TAVI and looks at TAVI versus surgical aortic valve replacement (SAVR) in patients with bicuspid aortic valve (BAV) stenosis. While patients treated with TAVI had a higher need for pacemaker implantation, authors Monil Majmundar, Ankur Kalra and colleagues suggest that it could still be considered as a feasible alternative to SAVR which does not require concurrent aortic root repair. Still, they acknowledge that more studies are needed.
Continuing with TAVI, Taishi Okuno, Thomas Pilgrim and colleagues look at patients with mild paravalvular regurgitation (PVR) after the procedure and compared them with patients who had no signs of PVR in order to understand the impact of this phenomenon on outcomes at 5 years. The negative effects of PVR were seen to be consistent with an increased risk of mortality and, thus, could play an important role in choosing between TAVI or SAVR.
The mitral valve is the subject of the next article in which Jasmin Shamekhi, Georg Nickenig and colleagues study the different stages in right heart remodelling caused by mitral regurgitation to evaluate the impact remodelling has on patient survival after transcatheter mitral valve repair. The greater the extent of the remodelling, the more mortality was seen to increase. With this observation in mind, the authors developed a simple staging classification that characterises the extent of right heart remodelling and provides an objective basis for risk prediction for patients about to undergo a MitraClip procedure.
Turning to interventions for stroke, Frederic A. Sebag, Nicolas Amabile and colleagues present the multicentre TRAPEUR registry. Left atrial appendage (LAA) thrombus represents a contraindication to LAA closure, and this registry looked at patients who were treated using a thrombus-trapping closure procedure. While still in its early stages, the LAA thrombus-trapping closure procedure was seen to be safe and feasible in select patients, especially those who had contraindications to long-term oral anticoagulation.
While percutaneous patent foramen ovale (PFO) closure is considered a safe and effective treatment for secondary stroke protection, PFO closure systems can carry a potential risk of early and late complications. Alessandro Beneduce, Matteo Montorfano and colleagues discuss the potential of suture-mediated PFO closure using the NobleStitch EL device in a short report using highly sensitive transoesophageal echocardiographic findings. Continuing with the NobleStitch EL system, a research correspondence by Jessica Zannoni, Federico De Marco and colleagues presents a study designed to determine the specific mechanisms of failure that could occur with this alternative to traditional device closure.
A short report by Ignacio Cruz-González, Yat-yin Lam and colleagues explores the use of two devices for percutaneous LAA occlusion when the LAA exceeds the dimensions of a single device. Using the LAmbre device, the authors conclude that a two-device technique is feasible and safer than using a single device in this complex anatomy.
Treating coronary artery bifurcation lesions by percutaneous coronary intervention (PCI) carries many procedural challenges as well as a higher risk of adverse events. In an expert review focusing on different types of crush techniques, Francesco Moroni, Lorenzo Azzalini and colleagues go beyond the provisional single-stent approach to consider the treatment of more complex lesions involving both branches and requiring a two-stent approach. The crush techniques have been shown to have excellent long-lasting results, and the authors summarise the latest technical and clinical information concerning this approach as well as its future perspectives.
Translational research is the subject of the next article in which authors Gabor G. Toth, William Wijns and colleagues attempt to better understand longitudinal stent deformation occurring during the proximal optimisation technique in treating bifurcations by PCI. As opposed to what might be commonly believed, the authors note that this technique results in elongation rather than shortening of the proximal stent segment, a critical observation to be considered in procedural planning when choosing stent length or during stent positioning.
Finally, using near-infrared spectroscopy (NIRS), the Lipid Rich Plaque (LRP) study was designed to see whether lipid-rich plaques were associated with a higher incidence of non-culprit major adverse cardiovascular events. In this research correspondence, Rebecca Torguson, Ron Waksman and colleagues present a subanalysis of the LRP study looking at the correlation between lipid-rich plaques and both LDL and HDL cholesterol among patients enrolled in the LRP study.
And now, while you enjoy EuroPCR in person or virtually, “live” or on demand, let’s turn to the articles themselves.
Supplementary data
To read the full content of this article, please download the PDF.