The first EuroCTO Club meeting after the new Eucomed rules became effective was a success, a testimony to the motivation of the 250 active physicians participating, mainly members of the Club, benefiting only in part from the educational grants provided by the generous contribution of the industry. The congress scientific programme always starts with a review of the recent CTO literature, this time including four randomised trials. The absence of changes in magnetic resonance imaging (MRI)-measured left ventricular ejection fraction (LVEF) and end-diastolic volume in the Evaluating XIENCE and Left Ventricular Function in Percutaneous Coronary Intervention on Occlusions After ST-Elevation Myocardial Infarction (EXPLORE) trial1, randomising 304 patients with a CTO in a non-culprit vessel within a week after STEMI, was confirmed by another smaller randomised trial in a less acute setting, the Recovery of Left Ventricular Function After Stent Implantation in Chronic Total Occlusion of Coronary Arteries (REVASC CTO) study2. Mashayekhi et al2 found no differences in regional wall thickening, again measured with MRI, in the 205 CTO patients randomised to receive or not receive revascularisation. In their original publication, the EXPLORE investigators suggested a possible improvement limited to patients with left anterior descending (LAD) occlusion. They now extend this to patients having good collateral flow to the CTO territory3, but still without clear evidence of clinical improvement. In the EXPLORE trial, anginal symptoms improved in the CTO group at one year but became similar at three years with a paradoxical worse cardiac mortality in the treated group (6.0% in the CTO PCI group vs. 1.0% in the CTO no PCI group, p=0.02)4. These results are totally at variance with the evidence confirmed in multiple trials, the last in the special population of 201 cardiogenic shock post-STEMI patients with non-culprit CTO included in the IABP-SHOCK II trial5, that CTO determines an independent mortality risk at 12 months after myocardial infarction (HR 1.30, 95% CI: 1.02-1.67, p=0.03). Also, the survivors to the acute phase have a worse prognosis in this trial substudy, with appropriate electrical shocks from the implantable cardioverter defibrillators (ICD) significantly more frequent in the presence of a non-culprit CTO, a finding confirmed in the 240 patients with CTO out of the 720 patients enrolled in the eCTOpy-in-ICD registry6. The favourable results both in terms of improved LVEF and dyspnoea in the low LVEF cohort of the 839-patient study conducted in Bad Krozingen and Zurich7 were discussed during the meeting by Galassi, who also elaborated on further indications for the use of LV assist devices during PCI. With 834 patients enrolled despite the premature termination, the Drug-Eluting Stent Implantation Versus Optimal Medical Treatment in Patients With Chronic Total Occlusion (DECISION-CTO) trial (ClinicalTrials.gov Identifier: NCT01078051) remains the largest randomised trial of CTO recanalisation (Park SJ. Presented at the American College of Cardiology Congress 2017, Washington DC, USA, March 2017). Its negative outcome (no difference in MACE in the intention-to-treat analysis) stunned the CTO operators at the time of presentation last year. Now we realise that the fundamental bias of allowing non-CTO artery treatment at the time of randomisation is in part responsible for an outcome totally different from the results of a countless number of registries comparing patients with failed vs. successful CTO PCI, the most recent being a registry of 5,496 patients from the PanLondon BCIS database8. The DECISION-CTO investigators rightly decided to present a per protocol analysis, considering a crossover of 78/398 (19.6%) from medical treatment to PCI, most of them in the first three days post randomisation, and a crossover in the opposite direction of 7.0% (Lee SW. DECISION-CTO: updated QoL and long-term outcomes. Presented at TCTAP 2018, Seoul, Korea, April 2018). Patients in these two groups had an incidence of combined MACE completely at variance with the incidence observed in the group of initial randomisation, partially invalidating the results of the intention-to-treat analysis. In the light of this high crossover rate, the lack of symptomatic improvement at one year initially reported can also be viewed differently, especially after new data showing that, at three to six and 12 months, all the functional indices improved in the successfully treated group. These results are at variance with all other reports including the marked improvement of quality of life at one month in the recently published individually monitored 1,000-patient Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures (OPEN CTO) registry9,10. Martin-Yuste, the top enroller of the EuroCTO trial11, reviewed its results. The recent publication of this trial, surely the greatest achievement of the EuroCTO Club with a highly significant improvement of angina frequency (5.23, 95% CI: 1.75-8.71; p=0.003) and quality of life (6.62, 95% CI: 1.78-11.46; p=0.007) at 12 months in the PCI group, certainly played a major role in eliminating restrictions to CTO recanalisation in the most recent European Society of Cardiology Guidelines on Myocardial Revascularization, with indications now only focused on symptoms and ischaemia, irrespective of lesion complexity12. In a paragraph dedicated to CTO recanalisation, recommendations include the need to ensure viability in case of regional myocardial impairment, the discouragement to proceed ad hoc and the opportunity that these procedures be reserved to expert CTO operators.
Other highlights of the congress included an update on the CASTLE score13 (Table 1), an acronym for the five elements (previous CABG, age, stump, tortuosity, length, extent of calcification) affecting success in the EuroCTO registry, a report prior to publication of the trends in CTO recanalisation from the 2008-2015 registry14 (Figure 1), and many technical lectures on the characteristics and mode of use of recently introduced dedicated devices, from guidewires to microcatheters, dual lumen catheters, trapping devices alone or in combination with guide extension, and low-profile balloons.
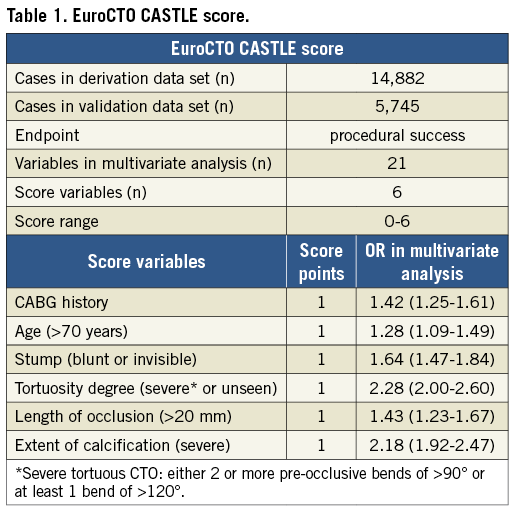
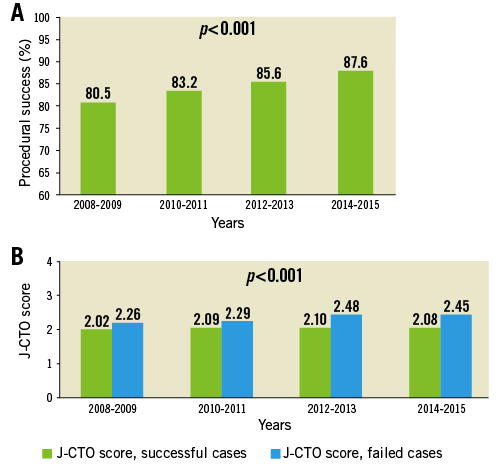
Figure 1. Procedural success trend in the EuroCTO Registry and the importance of the J-CTO score. A) Procedural success and B) J-CTO score. Adapted from the presentation by G. Sianos at EuroCTO 2018, Toulouse, France. https://www.eurocto.eu/events/it-IT/858/10th-experts-live-cto-workshop/presentation
As in the last five years, some of the most experienced operators in the Club demonstrated new techniques and material during live cases, working with the support of colleagues from the Rangueil University Hospital coordinated by N. Boudou and D. Carrié (https://www.eurocto.eu/events/it-IT/858/10th-experts-live-cto-workshop/video). The cases selected truly reflected the target audience - extremely complex CTOs requiring all the skills, tricks and attention of the operators to overcome truly ambiguous stumps, extreme tortuosity and calcification, very long occlusions, curly invisible septal and epicardial collaterals, very poor LVEF requiring Impella support during the procedure. The absence of complications in all cases and the success in 10/11 CTOs approached (90.9%) confirms the steady progress in this field. The EuroCTO Club meeting is unique because it offers the possibility to see at work US (Karmpaliotis, De Martini, Brilakis), Japanese (Yamane, Nasu) and European operators (Werner, Garbo, Boudou, Lefevre, Di Mario, Avran, Sianos, Galassi, Bufe, Mashayekhi, Ledermann, Levesque, Quillet, Hovasse, Drogoul, Tchetche, Weilenmann). In past editions differences were clear, with Japanese operators stressing careful wire manipulation and the importance of avoiding subintimal tracking or limiting it to the occluded segment, and US operators focusing on rapid change of procedural strategy following the hybrid algorithm, ready to move to anterograde dissection re-entry (ADR) or retrograde strategies for long lesions or ambiguous caps. This year the general impression was that the best of the two worlds joined in this European blend, taking full advantage of the extraordinary steerability of modern dual-core guidewires but also accepting knuckling and other aggressive strategies in the worst anatomies. Very trackable microcatheters, dual lumen catheters parked in a side branch originating at the occlusion site to penetrate the occlusion or re-enter a side branch at the distal end or facilitate the parallel wire technique, trapping balloons and combined trapping-guide extension devices were certainly instrumental in reducing the procedure duration and minimising contrast and X-ray exposure (no procedure went above 350 ml and 3 Gy).
EuroCTO Experts Live will be back in Berlin on 13-14 September 2019, to showcase once again the new advances offered by the science and technique of CTO recanalisation.
Conflict of interest statement
R. Garbo is a consultant for Terumo, Volcano and IMDS. D. Hildick-Smith is an advisor/speaker for Abbott, Boston, Medtronic and Terumo. The other authors have no conflicts of interest to declare.