Dear Sir,
We read with interest the paper by Petraco et al1 in which they advocate a hybrid instantaneous wave-free ratio/fractional flow reserve (iFR/FFR) strategy as a substitute for an FFR-only strategy to guide coronary intervention. Their findings are remarkably similar to what we reported over two years ago2 using the much simpler and more well-established index, resting Pd/Pa. Surprisingly, our findings are not even mentioned in their paper.
The concept of iFR has certainly caused a “stir” within the interventional cardiology community and has met with widely disparate reactions from outright rejection3,4 to cautious optimism5,6.The premise that iFR is independent of hyperaemia and that it correlates strongly with FFR in the clinically relevant range (0.6-0.9) has been challenged by several, well-established researchers in the field7. Furthermore, although termed “instantaneous”, iFR is in fact calculated as the ratio of a mean distal coronary pressure to a mean aortic pressure (Pd/Pa) during a predefined fixed part of diastole (the so-called wave-free period), for added “robustness and stability”; as such, it can be viewed as simply a refined resting Pd/Pa.
Having demonstrated excellent diagnostic agreement with FFR across a broad range of coronary stenoses, including the more clinically relevant intermediate stenoses8,9, the same authors now define the clinical utility of iFR by advocating its selective use with FFR in a “hybrid manner”1. For an iFR of <0.86, the authors advocate treating the lesion, for an iFR of >0.93, they recommend deferring treatment and for the intermediate range of iFRs (0.86-0.93), they recommend proceeding to FFR. By pursuing such hybrid strategy, the need for vasodilator drugs (and thus FFR) is obviated in 57% of cases, whilst maintaining 95% agreement with an FFR only strategy. Petraco et al’s study was a multicentre study, composed of two independent study cohorts and using two pressure wire systems, different routes of administration of adenosine (i.v. and/or i.c.) and different i.v. adenosine dosages (ranging from 140-200 µg/kg/min). As acknowledged by the authors, such methodological differences may have introduced some differences between the groups, and thus influenced their final conclusions.
In our large, single-centre study2, we investigated the relationship between resting Pd/Pa and FFR in 528 consecutive, “real-world” pressure wire studies. We consistently used the Radi pressure wire and a continuous i.v. infusion of adenosine at a dose of 140 µg/kg/min in all cases. We demonstrated a linear correlation between resting Pd/Pa and FFR, with a correlation coefficient of 0.74. When an FFR of ≤0.80 was defined as positive (as per FAME), a resting Pd/Pa of ≤0.87 had a positive predictive value (PPV) of 94.6%, whilst a resting Pd/Pa of ≥0.96 had a negative predictive value (NPV) of 93%. When an FFR of ≤0.75 was defined as positive (as per DEFER), the corresponding values for the resting Pd/Pa were ≤0.85 (with a PPV of 95%) and ≥0.93 (with a NPV of 95.7%). With such high positive and negative predictive values, we concluded that pharmacological vasodilatation and FFR measurement may not be necessary in 66% and 47% of patients, depending on whether DEFER or FAME criteria, respectively, are used to define a positive result. We also argued that the greatest utility of the resting Pd/Pa appears to be in predicting a negative FFR since resting values of Pd/Pa which predict a positive FFR constitute a minority of cases.
At a time when iFR technology is still maturing and in need of further validation before it can be more widely accepted, perhaps interventional cardiologists should consider using the much simpler, yet equally informative index, resting Pd/Pa, to guide their coronary interventions. After all, resting Pd/Pa is a readily available index which constitutes an integral part of any pressure wire procedure and does not require any sophisticated algorithms for its computation.
Conflict of interest statement
The authors have no conflicts of interest to declare.
We thank El-Omar et al for their interest in our work. Firstly, we would like to acknowledge the relevance of their previous research evaluating the relationship of baseline Pd/Pa ratio with hyperaemic fractional flow reserve (FFR) in a large population of patients undergoing pressure-wire interrogation of intermediate stenoses1. Their findings are indeed very supportive of the fact that, contrary to what has been widely reported over the last 20 years, baseline coronary haemodynamics can provide valuable information about coronary stenosis severity. In agreement with our proposed hybrid iFR-FFR strategy, they also demonstrated that a baseline index, Pd/Pa, could be used to limit adenosine administration in the catheterisation laboratory.
The Oxford Dictionary defines “instantaneous” as “existing or measured at a particular instant”, and “instant” as “a precise moment of time”. We believe that, therefore, iFR is not a misnomer. Being grammatically and semantically correct, we chose the term “instantaneous” to highlight the fact that iFR is measured at a precise moment of the cardiac cycle. Whole cycle coronary pressure indices, such as baseline Pd/Pa and FFR, are calculated as ratios of means and displayed as moving averages of 3-5 beats. The reason for doing so is because, as can be seen in Figure 1, an instantaneous ratio of Pd/Pa varies significantly over the whole cardiac cycle –in the example ranging from 0.8 to 1 within the same beat! However, closer inspection of the same trace will reveal a period in diastole (the wave-free period) during which, in each beat, the Pd/Pa ratio is remarkably stable, yielding therefore an instantaneous ratio of pressures (iFR) which can be reproduced in each cardiac cycle and used to reflect the severity of a coronary stenosis. This figure also clearly demonstrates the foremost importance of correctly identifying the wave-free window. Perhaps El-Omar and his colleagues are unaware of the fact that the well-established investigators of VERIFY rushed to develop an iFR algorithm for detection of the wave-free window and in doing so inadvertently included a portion of systole in their calculations. This in part explains the VERIFY investigators disappointing results, which differ markedly from RESOLVE and every other reported iFR study. Although we call for a great caution in interpreting the results of VERIFY, we welcome other investigators’ ambition to replicate our results in such a short period of time. Finally, El-Omar and his colleagues are correct to point out that the robustness and stability of iFR are improved when values are averaged over a longer period of time, as is the case for any biological or non-biological measurement. Yet, this is not in conflict with the fact that iFR is based on selective, instantaneous pressure measurements within the diastolic period.
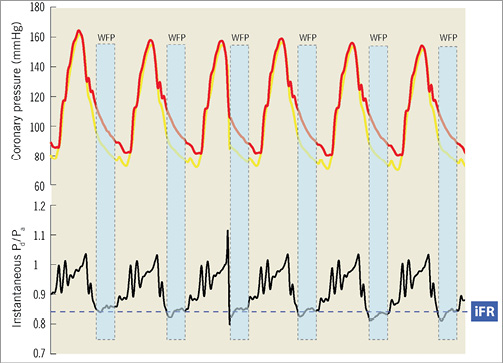
Figure 1. Whilst the instantaneous ratio of coronary pressures (Pd/Pa) is extremely variable over the whole cardiac cycle, sampling the wave-free window (WFW) permits the identification of a stable period of Pd/Pa, the instantaneous wave-free ratio (iFR).
It is also very reassuring for patients that our study results are very similar to those reported by Mamas et al1. We both found that 40-47% of patients would be spared from adenosine in a hybrid Pd/Pa-FFR strategy. However, any further detailed comparison with our dataset is not possible, since the proportion of any population free from adenosine can only be compared between samples with the same disease distribution. The fact that the article by Mamas et al didn’t include a histogram of FFR values nor provided the mean FFR value of their sample precludes any further insights on this aspect. More importantly, the authors did not base their analysis on the overall agreement between their proposed strategy and an FFR-only strategy, which again makes direct comparisons more difficult.
However, the unique and most important finding of our study is that a hybrid iFR-FFR strategy would spare 57% of patients from the need of adenosine, whilst maintaining the safety of a 95% agreement with FFR2. This number would increase to 76%, if the 0.75-0.8 (DEFER-FAME) grey zone is accounted for. Importantly, for any level of desired agreement with an FFR-only strategy, iFR would spare more patients from adenosine than resting Pd/Pa (Figure 2). We are also glad to report that this was indeed confirmed in the RESOLVE study, presented at TCT 2012, which demonstrated the superiority of iFR over Pd/Pa to spare patients from adenosine (57% vs. 40%) in hybrid strategies with FFR3. Therefore, we see their description of iFR as a “refined resting Pd/Pa” as absolutely correct and indeed complementary. We would, however, only permit ourselves to describe iFR as a “physiologically refined resting Pd/Pa”.
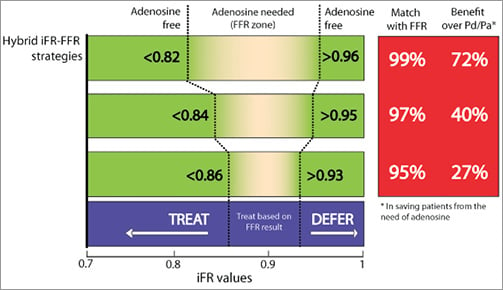
Figure 2. For each magnitude of desired agreement with an FFR-only strategy, the instantaneous wave-free ratio (iFR) spares significantly more patients from adenosine than Pd/Pa, when used in hybrid strategies with FFR.
The reasons for the improved performance of iFR lies in its refined physiological properties over whole-cycle Pd/Pa. Whilst iFR automatically samples a window of the cardiac cycle with the highest flow and pressure gradient, whole-cycle Pd/Pa includes systole in its calculation, which from the coronary haemodynamic perspective only represents noise. The practical implications of this improved signal-to-noise ratio of iFR is that it increases the range of values of the index for any given population. For instance, more than 95% of the patients in the study by Mamas et al had Pd/Pa values confined to a narrow 0.86-1 range (only 15 possible results). iFR, on the other hand, has a much higher dynamic range, with 95% of the values ranging from 0.73 to 1 in our study sample (28 possible results). Clinically, this means that 23% of our patients fell below the iFR treatment threshold of <0.86, in contrast to only 7% reported by Mamas et al with a Pd/Pa below their recommended cut-off of 0.87.
Despite these differences, we entirely agree that interventionalists shouldn’t be discouraged from using Pd/Pa in a hybrid strategy with FFR. This approach would spare a proportion of patients from adenosine and perhaps improve catheter laboratory logistics. Soon, when iFR becomes available and before clinical trials judge its role as an independent guide to revascularisation, a hybrid iFR-FFR strategy would enable full advantage of baseline coronary pressures to be taken, with nearly 60% of patients not requiring adenosine for physiological evaluation of coronary stenoses.
Finally, Mamas et al are right to point out that our estimations on the value of a hybrid iFR-FFR strategy are based on a retrospective analysis of real-life patient cohorts, and that this is invariably associated with limitations. In that regard, they should be aware that ADVISE II, a large prospective, multicentre and double-blind study investigating the classification agreement of iFR and FFR in the context of a hybrid strategy approach, is currently underway (http://clinicaltrials.gov/ct2/show/NCT01740895). ADVISE II will use a robust standardised data collection protocol and will be analysed in an independent core lab using the same software that will be available for online use in the catheterisation laboratory.
Conflict of interest statement
J.E. Davies holds patents pertaining to this technology, which is under licence to Volcano Corporation and is also a consultant for Volcano Corporation. The other authors have no conflicts of interest to declare.

