Abstract
Aims: The purpose of this study was to evaluate the impact of arterial access site on bleeding and ischaemic outcomes, overall and by treatment strategy, in patients with acute coronary syndromes (ACS).
Methods and results: In the ACUITY trial, 13,819 patients with moderate and high-risk ACS were randomised to either heparin (unfractionated or enoxaparin) plus a glycoprotein IIb/IIIa inhibitor (GPI), bivalirudin plus a GPI, or bivalirudin alone.
Per operator choice, femoral access was utilised in 11,989 patients (93.8%) and radial access in 798 patients (6.2%). There was no significant difference in composite ischaemia between the radial and femoral approaches at 30 days (8.1% vs 7.5%, p=0.18) or 1 year (14.7% vs 15.5%, p=0.77), although fewer major bleeding complications occurred with the use of radial access (3.0%vs4.8%, p=0.03). Use of bivalirudin monotherapy was associated with significantly less 30-day major bleeding than heparin plus GPI after femoral access (3.0% vs 5.8%, p<0.0001), but not with radial access (4.2% vs 2.2%, P=0.19). Major or minor organ bleeding was reduced with bivalirudin monotherapy compared to heparin plus GPI to a similar extent with both femoral (4.1% vs 7.4%, P<0.0001) and radial (4.9% vs 7.2%, P=0.26) access.
Conclusions: Transradial compared to femoral arterial access is associated with similar rates of composite ischaemia and with fewer major bleeding complications in patients with ACS managed invasively. Bivalirudin monotherapy compared to heparin plus GPIs significantly reduces access site related major bleeding complications with femoral but not radial artery access, though non-access site related bleeding is reduced by bivalirudin monotherapy in all patients.
Abbreviations
ACS: acute coronary syndromes
CABG: coronary artery bypass graft surgery
GPI: glycoprotein IIb/IIIa inhibitor
MI: myocardial infarction
PCI: percutaneous coronary intervention
TIMI: thrombolysis in myocardial infarction
UFH: unfractionated heparin
Introduction
Current practice guidelines generally recommend an early invasive strategy of angiography, followed by either percutaneous coronary intervention (PCI), coronary artery bypass surgery (CABG) or medical management for patients with moderate and high-risk acute coronary syndromes (ACS)1,2. Although pharmacologic regimens consisting of aspirin, clopidogrel, a glycoprotein IIb/IIIa inhibitor (GPI) and unfractionated or low molecular weight heparin are also recommended in conjunction with interventional management, bleeding is a major concern in these patients3,4 and has been consistently associated with increased mortality and other adverse outcomes5-12. In the Acute Catheterisation and Urgent Intervention Triage strategY (ACUITY) trial, in which 13,819 moderate and high-risk ACS patients were randomised to unfractionated heparin or enoxaparin plus a GPI, bivalirudin plus a GPI, or bivalirudin alone, major bleeding within 30 days not related to CABG occurred in approximately 5% of patients, minor bleeding occurred in 19% of patients, and 2.3% of patients required blood product transfusion. The use of bivalirudin alone resulted in comparable rates of ischaemic events, significantly fewer major bleeding complications, and superior net clinical outcomes compared to combination therapy with unfractionated heparin or enoxaparin plus GPI13,14. In addition to anticoagulant choice, the selection of vascular access site has also been shown to impact bleeding complications. Radial artery compared to femoral artery access has been associated with a reduction in the risk of access-site bleeding and other vascular complications15-18. The impact of radial compared to femoral artery access on ischaemic and bleeding events has not been extensively evaluated in a large cohort of patients with ACS treated with contemporary antithrombotic regimens and an early invasive strategy. We therefore assessed the impact of the arterial access site from the ACUITY trial database.
Materials and methods
Study design
The study design of the ACUITY trial has been previously described in detail19. Briefly, 13,819 patients with moderate and high-risk ACS from 17 countries were randomly assigned in open-label fashion to one of three antithrombin regimens: unfractionated heparin or enoxaparin plus GPI, bivalirudin (IV bolus of 0.1 mg/kg and an infusion of 0.25 mg/kg/h with an additional bolus 0.5 mg/kg and an increased infusion rate of 1.75 mg/kg/h if the patient continued on to PCI) plus GPI, or bivalirudin alone. Patients assigned to GPI were randomised again to routine upfront use vs deferred selective administration after angiography in patients undergoing PCI.
Interventions
Patients were managed with an early invasive treatment strategy based on American College of Cardiology/American Heart Association and European Society of Cardiology guidelines1,2. Angiography was performed within 72 hours after randomisation, after which patients were triaged to PCI, CABG, or medical management at the investigating physician’s discretion. The choice of the arterial access site was left to the discretion of the investigating physician. Access site information was only collected for the first coronary angiography procedure. Patients undergoing deferred PCI, in whom a different access site was potentially used, were excluded from the present analysis (n=28), as were patients with brachial access (n=90) or whose records lacked access-site information (n=914). After excluding these patients, the study population consisted of 12,787 patients.
Aspirin 300-325 mg PO or 250-500 mg IV was administered daily during the index hospitalisation, followed by 75-325 mg daily indefinitely after discharge. The initial dosing and timing of clopidogrel were left to investigator discretion as per local standards, though a 300 mg or greater loading dose was recommended in all cases no later than two hours after PCI. Clopidogrel 75 mg daily was recommended for one year in all patients with coronary artery disease.
Endpoints
The three primary endpoints at 30-days in ACUITY were composite ischaemia (defined as the occurrence of death, myocardial infarction [MI] and unplanned revascularisation for ischaemia); non-CABG major bleeding (defined as intracranial or intraocular bleeding; access site haemorrhage requiring radiological or surgical intervention; ≥5 cm diameter haematoma; reduction in haemoglobin of ≥4 g/dL without or ≥3 g/dL with an overt bleeding source; reoperation for bleeding; or blood product transfusion); and net clinical adverse outcomes (defined as composite ischaemia or major bleeding). Bleeding endpoints were not collected beyond 30 days. The present analysis thus evaluates the impact of arterial access site and randomisation arm on the rates of major bleeding at 30 days, and the rates of composite ischaemia and mortality at 30 days and one year.
Statistical analysis
Comparisons of baseline, angiographic, and procedural characteristics were carried out according to access site (femoral or radial). All analyses were by intention to treat. Continuous variables are reported as medians and interquartile range, and categorical variables were summarised as percentages. Categorical variables were compared by Chi-square and continuous variables were compared by the non-parametric Wilcoxon rank sum test. Kaplan-Meier plots were used to depict major bleeding and composite ischaemia event rates for radial and femoral patients. Cox models were used to adjust for baseline imbalances between the two groups.
Results
Baseline characteristics of study population. The femoral approach was used in 93.8% (n=11,989) of patients, and the radial approach was used in 6.2% of patients (n=798). As described in Table 1, significant differences were present in the baseline characteristics of patients treated by the radial approach and those treated by the femoral approach.
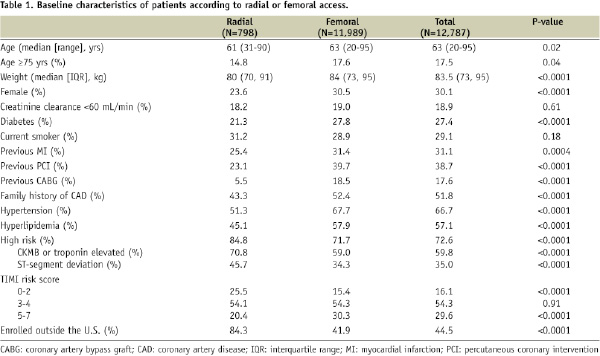
Patients in the femoral group were older, more often women, were more likely to have cardiac risk factors and established coronary artery disease and were more likely to be enrolled in the US. Patients treated by the radial approach more frequently had positive biomarkers and ST-segment deviation.
Clinical outcomes by access site
As seen in Table 2 and Figure 1, the 30-day and 1-year rates of composite ischaemia were similar for the radial and femoral approaches.
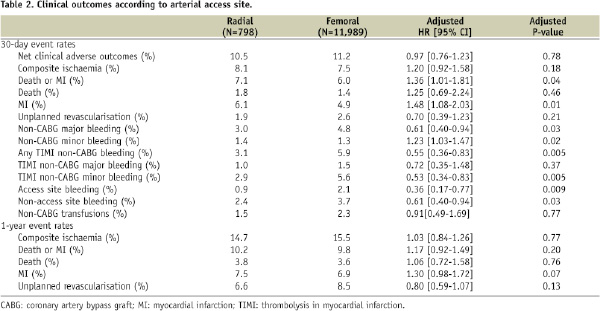
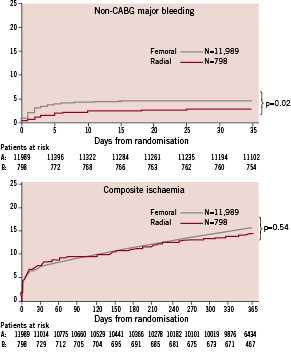
Figure 1. Kaplan-Meier curves for 30-day non-CABG major bleeding (top) and one-year composite ischaemia (bottom).
However, a significant reduction in non-CABG-major bleeding at 30 days was observed with the radial approach compared to the femoral approach (adjusted HR [95% CI]=0.61 [0.40-0.94], p=0.03) (Table 2 and Figure 1).
Transfusion rates were not significantly different between the radial and the femoral approaches, however. At 30 days the adjusted rates of MI (6.1% vs 4.9%, adjusted HR [95% CI]=1.48 [1.08-2.03], p=0.01) and composite death or MI (7.1% vs 6.0%, adjusted HR [95% CI]=1.36 [1.01-1.81], p=0.04) were higher in patients treated by the radial artery compared to the femoral approach, though there were no statistically significant differences in composite ischaemia. At one year, there were no significant differences in ischaemic event rates between patients treated with femoral vs the radial artery approach.
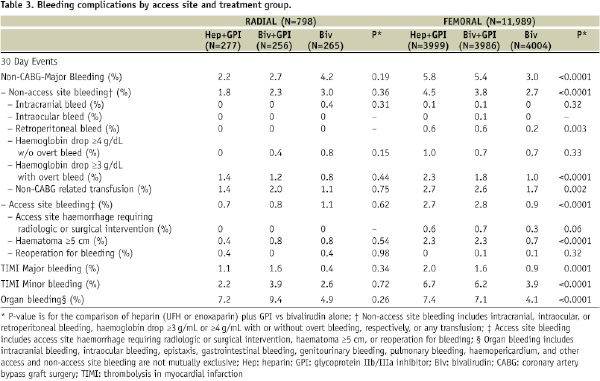
Bleeding and transfusion by access site and treatment group
As seen in Table 3, bivalirudin monotherapy compared to heparin plus a GPI significantly reduced the 30-day rates of non-CABG-related major bleeding, transfusion, and non-access-site bleeding in patients treated with the femoral approach patients. A bivalirudin-alone strategy was also associated with lower rates of TIMI major and minor bleeding complications in femoral-approach patients. In contrast, rates of non-CABG major bleeding, access-site bleeding, and transfusion were not significantly different between the randomisation arms in patients managed with the radial approach. The rates of major or minor organ bleeding were reduced to a similar extent in patients treated with bivalirudin alone compared to heparin plus a GPI and were present with both femoral access (4.1% vs 7.4% respectively, p<0.0001) and radial access (4.9% vs 7.2% respectively, p=0.26).
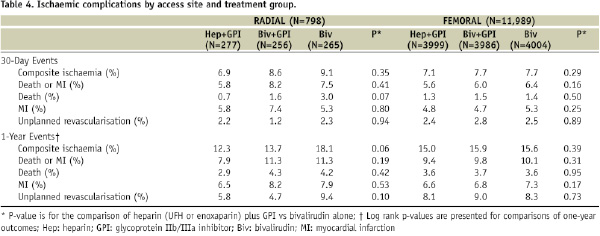
Ischaemic events by access site and treatment group
As seen in Table 4, there were no significant differences in the rates of ischaemic events rates at 30 days and one year among patients treated with bivalirudin alone compared with heparin plus a GPI, regardless of the arterial access used.
Discussion
The current study demonstrates that the effect of bivalirudin in reducing access site haemorrhage in patients with ACS undergoing invasive management may be restricted to those treated with femoral artery access. Among patients in ACUITY with vascular access obtained by the radial artery, haemorrhagic complications occurred with similar frequency in patients treated with heparin plus GPIs and bivalirudin monotherapy. Of note, however, as might be expected, non-access site related bleeding and organ bleeding were reduced to a similar degree with bivalirudin monotherapy compared to heparin plus a GPI managed by both femoral and radial artery access, though the difference did not reach statistical significance for the radial approach given the small sample size.
Femoral access site complications are responsible for a significant proportion of the bleeding complications in patients with ACS managed invasively12. In patients in whom femoral artery access is obtained, the sheath is often removed several hours after the procedure to allow recovery of coagulation after antithrombin discontinuation, a situation that may increase bleeding. Alternatively, femoral sheaths may be removed immediately with the use of vascular closure devices. However, these devices have not been found to reduce the rate of haemorrhagic or vascular complications in randomised trials20,21. The short half-life of bivalirudin, which allows rapid recovery of normal haemostasis after the infusion is discontinued, along with avoidance of GPI, likely contributes to the reduction in haemorrhagic complications with femoral artery access11,14.
In most prior studies, radial artery access has been associated with fewer bleeding events and transfusions compared to the femoral approach15-18, presumably because the radial artery is superficial and easily compressible. Patient comfort is increased, nursing staff workload is reduced, and outpatient treatment may be feasible22,23.
As evidenced in the ACUITY trial, radial artery access is still not widely utilised, though significant country by country variation in its use is known to exist24. The transradial technique requires a specific set of skills, and a significant learning curve is present that must be traversed. Radial artery spasm, arterial puncture failure, vascular anomalies and failure to reach the ascending aorta are obstacles which impede widespread uptake of this approach. However, with appropriate training, comparable success rates with the radial and femoral approaches may be achieved even in complex cases, with reduced rates of haemorrhagic and vascular complications15-18,25, justifying more widespread use of this technique. As shown in this study, a substantial proportion of bleeding complications still occur which are not related to the access site, a finding that supports the use of safer anticoagulant regimens to optimise patient outcomes.
The evidence base that is available supports a switch to radial access for most PCI procedures with the aim of improving outcome by reduction in access site bleeding. The MORTAL study26, recently published, retrospectively examined the association between access site, transfusion, and outcomes in over 32,000 patients who underwent PCI in British Columbia from 1999 to 2005. The main finding was that by reducing vascular access site complications, the use of the radial access site was associated with a 50% reduction in transfusion rate and a relative reduction in 30-day and 1-year mortality of 29% and 17%, respectively (p<0.001), which corresponds to around 1% absolute risk reduction at one year. Continuing randomised trials and namely a substudy of the OASIS 7 trial will ultimately confirm or refute these findings27.
Several limitations of this study should be considered. The present analysis is a post-hoc analysis from the ACUITY trial. Randomisation between the femoral and radial approaches was not performed. Since 93.8% patients in the ACUITY trial were managed via femoral access, the results in the relatively small radial artery access patient group must be considered observational and hypothesis-generating only. Even after multivariable adjustment to account for baseline differences, the extent to which unmeasured confounders affected the propensity for operators to have chosen the radial vs femoral access site cannot be determined.
Conclusions
In conclusion, in moderate- and high-risk patients with ACS undergoing an early invasive strategy, the use of the radial artery access site is associated with a significantly lower rate of major bleeding complications in comparison to the more conventional femoral artery access route. Treatment with bivalirudin monotherapy rather than heparin plus a GPI reduces the risk of major access site bleeding complications associated with femoral access, whereas access site bleeding complication rates are comparable with both regimens after transradial access. Bivalirudin monotherapy compared to heparin plus a GPI also reduces non-access site related bleeding complications in all patients. Further study is required to determine whether the rates of major ischaemic complications are comparable in high-risk ACS patients managed with radial rather than femoral access.