Abstract
Aims: To compare Cheatham Platinum (CP) stent and Palmaz stent for the treatment of native and postoperative lesions of congenital heart disease (CHD) patients.
Methods and results: From January 1998 to December 2007, 96 CP stents and 77 Palmaz stents were implanted in 89 and 64 CHD patients.
All stents could be deployed. Decrease in pressure gradient was higher with the CP than with the Palmaz stent (36.1±23 and 23.4±18.3 mmHg, p=0.004). The procedure was more often successful with a CP than with a Palmaz stent (96% and 88% of patients, p=0.03). Stent-related complications were more rarely observed with the CP than with the Palmaz stent (9% and 27%, p=0.007). The incidence of vascular dissection was lower with CP than with Palmaz stent (1% and 6%), the incidence of stent migration was similar in the two groups (8% and 6%). Balloon burst, never observed in the CP stent group, was frequent in the Palmaz group (0% and 11%, p=0.001). There were no procedural deaths. The need for urgent surgery was similar in the two groups (2% and 1%).
Conclusions: Our findings show a superiority of the CP over the Palmaz stent concerning efficacy and reduction of complications rate for the treatment of cardiac and vascular lesions of children and young adults with CHD.
Introduction
Stents have been used widely during the last 20 years to treat stenotic lesions in patients with congenital heart disease (CHD). Classical indications are stenotic lesions of the aorta, the systemic veins, the pulmonary outflow and the pulmonary arteries1. The recent introduction of the covered stent has allowed the exclusion of fistulae and aneurysms whether or not they are associated with stenotic lesions2-4. Stents classically used in CHD patients such as Palmaz stents and their subsequent evolutions were not specifically designed for this purpose. Their use in CHD lesions is burdened by a relatively high incidence of complications5,6.
The Cheatham Platinum (CP) stent was designed in 1996 to treat aortic coarctation7 in adolescents and adults. This stent is manufactured from wire of a platinum-iridium alloy that is bent and welded to a cylindrical mesh work. This procedure offers the advantage of obtaining a stent with rounded extremities that can be dilated from 8 to 25 mm. These characteristics make it of interest for use in the paediatric and young adult populations. The purpose of our study was to retrospectively examine our results concerning 153 consecutive patients treated with either a Palmaz type stent or a CP stent, comparing the efficacy and safety of these two types of stents in the treatment of congenital heart lesions.
Methods
From January 1998 to December 2007, 96 CP stents (34 covered) (Numed, Hopkinton, NY, USA) and 77 Palmaz stents (Cordis, Johnson & Johnson, Warren, NJ, USA) were implanted in 89 and 64 patients, respectively. Palmaz stents, and those evolved from it (the Genesis stent), were used until January 2003. After this date the CP stent was preferred, except for children weighing less than 15 Kg.
Inclusion criteria were all CHD patients, weighing more than 15 Kg, treated by stent implantation (CP or Palmaz) for native or post-surgical lesions. The characteristics of patients at time of stent implantation are shown in Table 1.
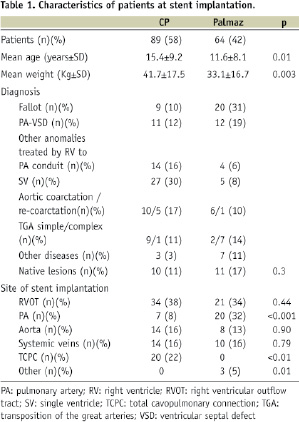
Diagnosis were: tetralogy of Fallot/pulmonary atresia with ventricular septal defect (VSD) (n=52); single ventricle (n=32); aortic coarctation (n=22); simple or complex transposition of the great arteries (TGA) (n=19); other anomalies treated by interposition of a right ventricle to pulmonary artery conduit (n=18); other diseases (n=10).
Patients were not indifferently treated by CP or Palmaz stent; in fact, only covered CP stents were used to exclude fenestrations of patients with total cavo-pulmonary connections and only Palmaz stents were used to treat stenotic lesions of vessels measuring less than 8 mm. These considerations explain why patients were older in the CP group and why there were differences concerning the site of stent implantation (Table 1).
The study was approved by the institutional review board. Written informed consent was obtained from children’s parents. Full and careful review of the medical record of each patient, including the full catheterisation report, was performed. Specific potential complications occurring during and/or after stent implantation were sought and recorded prospectively on a form. All adverse events were classified as serious or minor and related or not related to the procedure.
Stent implantation
Interventions were performed by two operators (GA, YB). The technique of stenting did not differ from that previously described and varied in accordance with the site of stent implantation1.
All exams were performed under general anaesthesia and mechanical ventilation, under antibiotic prophylaxis and heparin (50-100 UI/Kg). Vascular access varied in accordance with the site of stent implantation: the femoral vein was used in 119 cases; the internal jugular vein in seven and the femoral artery in 27.
Pressure gradient through the stenotic lesion and vessel diameter were measured before and after stenting. A Mullins long sheath (Cook Europe, Limerick, Ireland) was advanced over a stiff guidewire beyond the stenotic segment. Bare or covered CP stent (Numed, Hopkinton, NY, USA) and P308 or Genesis XD stents (Cordis, Johnson & Johnson, Warren, NJ, USA) were used in most cases. Premounted Genesis stents were used in eight cases in order to treat stenotic lesions of vessels measuring less than 8 mm in young patients. During the study period covered, CP stents were never used to treat stenotic lesions, namely aortic coarctation.
The CP stent was crimped on a BiB balloon (Numed, Hopkinton, NY, USA) in 77 cases and on a simple balloon (BALT, Extrusion, Monmorency, France; Tyshak or Z Med, Numed, Hopkinton, NY, USA; Powerflex, Cordis, Johnson and Johnson, Warren, NJ, USA) in 12. Palmaz stents were crimped on BiB balloon in 23 cases and on simple balloon in 41.
Predilation was performed in the presence of tight or calcific lesions by using high pressure balloons (Powerflex, Cordis, Johnson and Johnson, Warren, NJ, USA). Post-stent dilatation was performed in the presence of a persistent waist on the balloon or to stabilise the stent position after stent migration had occurred, by using Mullins balloons (Numed, Hopkinton, NY, USA). Angiography was repeated after stenting in order to confirm complete stent opening and to rule out vascular dissection.
Success of the procedure, in the absence of serious complications, was judged in accordance with:
– complete stent opening and / or a residual gradient < 20 mmHg for stenotic lesions involving the junction right ventricle to pulmonary artery and the aorta,
– complete stent opening and / or absence of residual gradient for stenotic lesions involving venous vessels
– complete stent opening and / or a residual gradient < 5 mmHg for stenotic lesions of pulmonary arteries
– complete stent opening and complete exclusion of aneurysms and communications promoting right to left shunt, when covered stents were used.
Complications were coded as stent-related (stent migration, balloon burst during stent dilatation, vascular dissection at implantation site) and non-stent-related complications (embolism, vascular thrombosis, arrhythmias, pulmonary oedema, cardiac arrest).
The seriousness of complications was defined as 1) mild: all transient events not accompanied by clinical consequences and not needing medical intervention; 2) moderate: all events that promptly recovered after medical intervention, without clinical consequences; 3) serious: all potentially lethal events needing prompt medical or surgical intervention and / or accompanied by permanent clinical consequences.
Statistical analysis
Descriptive statistics for the total population were obtained. Results were expressed as values and percentages for categorical variables and as mean ±Standard Deviation for continuous variables.
The variables studied were: diagnosis, age, weight, vascular access, site of stent implantation, native or post-surgical lesions, number of stents implanted per patient, type of balloon, need of pre-dilatation and post-stent dilatation, success of the procedure, frequency, type and seriousness of complications.
Independent risk factors of complications were identified using univariate analysis.
Chi-Squared or Fisher’s exact test for categorical variables and Student’s test with adjustment according to result of homogeneous variance test for quantitative variables were used, together with a review of univariate logistic model results.
A p-value less than 0.05 was considered statistically significant for stent groups comparison. A p-value less than 0.2 at univariate analysis was retained to entry a multivariate logistic regression model, performed by using stepwise procedure and aimed to identify potential predictive factors of complications. All statistical tests were bilateral. All analyses were performed using SAS 9.1.3 software.
Results
Haemodynamic data are shown in Table 2.
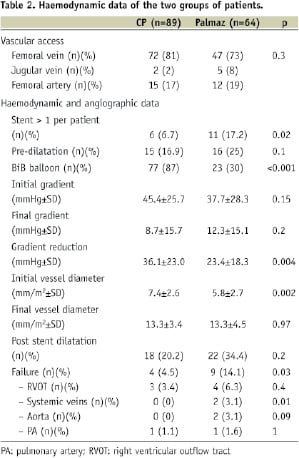
The types of vascular access were similar in the two groups. CP and Palmaz stents could be implanted in all cases.
The number of stents implanted per patient were significantly higher in the Palmaz group. Pre-dilatation was similarly used in the two groups of patients. A BiB balloon was more often used when implanting a CP stent and a simple balloon when implanting a Palmaz stent. Initial and final gradient through stenotic lesions were similar in the two groups, but the difference in gradient reduction was significantly higher in the CP group (36.1±23.0 mmHg and 23.4±18.3 mmHg, p=0.004). Initial vessel diameter was smaller in the Palmaz group, and final vessel diameter was similar in the two groups. Post-stent dilatation was similarly used in the two groups.
Thirty-four covered stents were used in 29 patients in order to exclude aneurysms (n=2) or fenestration of total cavo-pulmonary connections (n=27). In all cases, the stents could be implanted and led to aneurysm exclusion or total suppression of right to left shunt. Covered CP stents were implanted by using a BiB balloon in 18 cases and a simple balloon in 11 cases. Post-stent dilatation was used in three cases to improve stent adhesion to vascular wall. Three complications were observed: one stent migration into the inferior vena cava needing the implantation of a second stent, one air embolism in the inferior vena cava and the acute occlusion of a covered stent implanted to exclude collateral circulation prompting right to left shunt.
Failure, defined in accordance with the criteria illustrated above, was observed in four patients of the CP group and in nine patients of the Palmaz group (p=0.03). The efficacy of the CP stent was similar to that of Palmaz stent for the stenting of the right ventricular outflow, significantly higher than that of Palmaz stent for the stenting of systemic veins and higher than that of Palmaz for the stenting of aorta, but the difference was not statistically significantly (Table 2).
Twenty-five stent-related complications were observed. Numbers and types of complications are illustrated in Table 3.
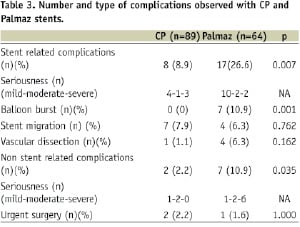

Stent related complications were more frequent in the Palmaz group. Stent migration was similar in the 2 groups, whereas vascular dissection more rarely occurred in the CP group, although the difference was not statistically significant (p=0.162). Balloon burst was never observed in the CP group. Three balloon bursts occurred in the Palmaz group when a BiB balloon was used, three when a simple balloon was used, one when a pre-mounted stent was used.
There were nine non-stent-related complications: two in the CP group (one air embolism and one acute stent thrombosis, occurring when using covered CP) and seven in the Palmaz group (two cardiac arrest, one flutter, one complete atrioventricular block, one ventricular tachycardia, one pulmonary oedema, one death) (p=0.04). The need for urgent surgery concerned two patients in the CP group (one homograft rupture and one stent migration in the right ventricle) and one patient in the Palmaz group (one aortic dissection).
There were no procedural deaths. In the CP group there was one late postoperative death of a child with pulmonary atresia-VSD and DiGeorge syndrome in whom stenting of the right ventricular outflow had failed. In the Palmaz group there was two periprocedural deaths: one child with pulmonary atresia-VSD died from haemorrhage after stenting of collateral vessels; one child with truncus arteriosus and severe dysfunction of the right ventricle died from persistent right ventricular dysfunction after stenting of both pulmonary arteries.
According to the results of univariate analysis, the incidence of stent-related and non-stent-related complications was not related to age, weight, vascular access, neither to type or site of lesions or to the need of pre-dilatation.
Complications were more frequently observed when post-stent dilatation and several stents were used. When considering the entire population (CP and Palmaz groups), complications more frequently occurred during stenting of the right ventricular outflow (48%), compared with stenting of systemic veins (12%), pulmonary arteries (20%) and aorta (16%). There were not significant differences between the two groups concerning the occurrence of complications during stenting of the right ventricular outflow (18 and 29%), systemic veins (7 and 20%), pulmonary arteries (0 and 25%) and aorta (7 and 38%), probably due to the relatively low number of complications observed (Table 3).
Multivariate analysis indicated a lower complication rate for patients receiving a CP stent (p=0.03) rather than a Palmaz stent. The need of post-stent dilatation was also identified as a predictor of complications (p<0.001).
Discussion
Our study shows that: 1) The use of CP stents to treat stenotic lesions of CHD patients is effective and relatively safe; 2) The overall efficacy of CP stents for the treatment of stenotic lesions is superior to that of the Palmaz stent; 3) CP stents’ overall safety is higher than that of the Palmaz stent; and 4) Covered CP stents can be safely used to exclude undesired communications between systemic veins and the pulmonary atrium or to exclude aneurysms.
The CP has been largely used in Europe to treat stenotic lesions of patients with CHD. However, few reports on CP stent exist8-10 and none shows a higher efficacy or safety compared with stents historically used to treat CHD patients. A disadvantage of CP stents over Palmaz stents is the necessity of sheaths 2 Fr larger than the implantation balloon. Indeed, although Palmaz stents have a limited possibility of over-dilatation and an important foreshortening, they can be inserted through sheaths smaller than 10 Fr. These differences in stent profile justify their use in different subgroups of patients.
Although our two populations were different concerning age, weight and indications to stent implantation, common indications for stenting (right ventricular outflow, systemic veins and aorta) were similar in the two groups and we did not find any correlation between age, weight or occurrence of complications.
As previously reported, we confirmed that the CP stent is effective to treat stenotic lesions of CHD patients8,10 and showed that its efficacy is higher than that of Palmaz stent.
In our series, stent-related complications were less frequent in the CP stent group. Stent migration was similar in the two groups, however balloon burst, generally causing stent migration or malapposition was never observed in the CP stent group. Although the BiB balloon was designed to prevent stent flaring, which is the more frequent cause of balloon burst, in our series balloon burst occurred during dilatation of two Palmaz stents mounted on a BiB balloon. We can assume that the different morphology of the stent edges, more than the modality of stent deployment, are responsible for this complication. Vascular dissection was also lower in the CP stent group, probably because of a diminished traumatism on adjacent structures induced by the rounded stent edges.
Non-stent-related complications were also more frequent in the Palmaz stent group. Namely, cardiac arrest, never observed in the CP stent group, was relatively frequent in the Palmaz stent group. Although in our series we did not find any correlation between age and non-stent-related complications, we cannot exclude that differences in the two populations are responsible for these results.
Stenting of the right ventricle to pulmonary artery conduit was introduced 15 years ago as a method to prolong the life of prosthetic conduits and diminish the number of surgical interventions in multi-operated patients11. In our series stenting of the right ventricular outflow was the most frequent indication to stent implantation and the procedure burdened by the higher incidence of complications. We could not find any difference of efficacy of CP over Palmaz stents concerning this indication. In our series, the incidence of complications in the two groups was similar and generally due to stent migration with or without balloon burst. In our center, stenting of the pulmonary arteries is rarely performed and limited to reconstructed pulmonary arteries. Palmaz stents were generally used for this indication, thus efficacy and safety in the two groups could not be compared.
Stenting is considered the elective treatment for re-coarctation of the aorta in adolescents and adults7. Primary stenting of the aortic isthmus, compared to balloon dilatation, might carry a lower incidence of re-coarctation, providing a theoretical lower incidence of dissection or tearing of the aortic wall, and thus diminishing the risk of aneurysm formation12. Some authors advocated the use of covered CP stent to diminish the incidence of complications on aortic wall during stenting10,13.
Although we observed only one minor complication during stenting of the aorta when using CP stents and the efficacy of CP stents was higher than that of Palmaz stent in this indication, the limited number of patients treated in the two groups did not allow us do show significant differences.
Stenosis of systemic veins can be observed in patients with TGA having had an atrial repair14,15 or in operated patients with pulmonary anomalous venous connection into the superior vena cava16. The incidence of complications during systemic veins stenting is relatively low. In accordance with previous results, in our series the incidence of complications during this procedure was low14,15 and the efficacy of the CP stent in this setting was significantly higher than that of Palmaz stent.
Covered CP stents were used to treat sub-atretic native aortic coarctation8,10, severe aortic coarctation12, native aortic coarctation or re-coarctation with aneurysm10, coarctation and patent ductus arteriosus2, collateral vessels prompting right to left shunt in a univentricular heart circulation17 and as a bail-out in cases of complications in the catheterisation laboratory. In our series we implanted covered stents only to exclude aneurysms of the pulmonary arteries3, collateral vessels prompting right to left shunt4 and to treat one homograft rupture. Apart from this last patient in whom stent implantation did not abolish bleeding, covered stents were effective in all other cases. No complications of covered stent implantations were reported in previous series10.
A particular group of patients receiving stenting in a systemic vein were patients with total cavo-pulmonary connection needing fenestration closure. The choice of devices to close fenestrations is guided by several factors, including size and location of the fenestration, its geometry, the need of placing a long sheath in the systemic atrium and patient weight.
We have recently shown that in old children a covered stent can be safely used to exclude fenestrations without entering the systemic atrium4. However, we limit this technique to children weighing more than 20 Kg. In fact the covered CP stent has to be inserted trough 12 Fr or 14 Fr sheaths. This technique in our series was accompanied by a very limited number of complications.
Study limitations
The study has several limitations. Although we present the retrospective results obtained in 153 consecutive patients, CP stents were only recently available in our center. After commercialisation, CP stents were used for patients weighing more than 15 Kg. Thus, although we excluded from statistical analysis patients weighing <15 Kg, the two populations were still different concerning age, weight of the patients and indications for stenting. These differences could not be entirely removed from the statistical model, due to the small number of patients included. However, it should be noted that, in our study, none of these differences were related to the occurrence of complications. Subgroup analyses were not performed as they would not be demonstrative.

