Abstract
Aims: The treatment of coronary bifurcation lesions is technically challenging. Conventional 2-dimensional angiography lacks the ability to properly image the true bifurcation geometry or its plaque distribution. The objectives of this study were to reconstruct coronary bifurcation lesions in 3 dimensions (3D) and to analyse the geometric changes that may occur immediately after stenting.
Methods and results: The CardiOp-B system (Paieon Inc.), a novel system for 3D reconstruction of the coronary vessels, was applied in a retrospective evaluation of 121 angiographic images from 27 patients (74% men, age 71±13 years) with bifurcation lesions in the coronary arteries treated by angioplasty procedures. Angulations between the bifurcation branches were measured before and after stenting. Side-branch involvement was found in 70% of cases. Comparison of the pre- and post-stenting angulation yielded a significantly lower angulation between the distal main branch and side branch after stenting (71±17° versus 58±18°, p<0.001).
Conclusions: 3D reconstructions may provide new insight into complex bifurcation lesions in space and may serve as an important tool for planning interventional procedures and evaluating their results. The implications of the demonstrated angulation changes after stenting should be further evaluated.
Introduction
Advances in coronary intervention technologies and the introduction of drug eluting stents have left few areas in need of major improvement. Treatment of bifurcation lesions in the coronary arteries remains an important challenge1,2. Although numerous balloon and guidewire techniques have been suggested to cope with the geometry of bifurcation vessels, not one method has proven conclusively superior. Stent deployment depends on the specific geometry of the complex curvilinear bifurcation and the distribution of lesions within it. However, conventional 2 dimensional (2D) angiography lacks the ability to properly image or analyse these factors3-5. A system for three dimensional (3D) reconstruction of the coronary segments has recently been validated in non-complex lesions with excellent precision on in vivo testing6, but there are as yet no clinical studies assessing 3D reconstruction of bifurcation lesions. The objectives of this study were to evaluate the application of the 3D system in the reconstruction of coronary bifurcation lesions and to analyse geometrical changes that may occur after stenting.
Methods
Image acquisition
A retrospective case series design was used. One hundred and twenty-one images were acquired from 27 consecutive patients who were referred for diagnostic coronary angiography at the Rabin Medical Center. All had angiographic evidence of coronary artery disease at a bifurcation, with stenosis of at least 50% of diameter in one or more vessel segments (Table 1).
Single-plane digital angiography systems (Philips Medical System, The Netherlands and Siemens Medical, Germany) were used to obtain 3-5 cine-angiograms for each patient at 25 frames/sec. The gantry angle of the projections and the diameter of the catheters were determined by the individual operator. Analyses were performed off-line, after completion of the angiographic study, using end diastolic images selected from each of the different projections and transferred to a computer workstation.
Two dimensional analysis
All 121 images were analysed by an independent and experienced investigator (D.D.) using QCA software (Medview™, Medcon Telemedicine Technology, Israel). The following variables were examined: proximal and distal reference diameter; minimal lesion diameter (including the percentage of diameter stenosis); proximal and distal reference area; and minimal lesion cross-sectional area (including the percentage of area stenosis). The bifurcation lesion was classified according to the Institut Cardiovasculaire Paris Sud classification of bifurcation lesions7.
Three dimensional reconstruction and analysis
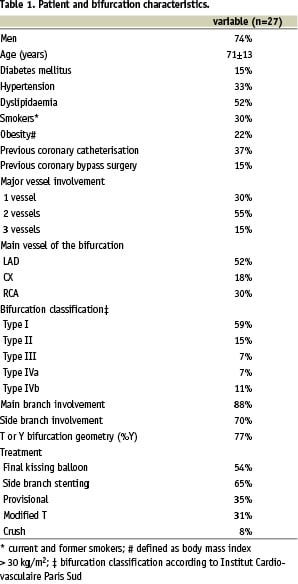
For 3D reconstruction, we used the CardiOp-BTM system (Paieon Inc.), which integrates information from at least two single plane angiographic images taken from different angles of projection (Figure 1)6.
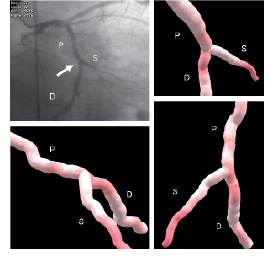
Figure 1. Demonstration of a coronary bifurcation (LCX-OM) bifurcation without significant obstruction. 2D angiography and 3D reconstruction in various projections. P- proximal main branch. D- distal main branch. S- side branch.
The initial steps in the 3D reconstruction protocol involve catheter calibration and demarcation of the region of interest. The rest of the reconstruction is performed automatically by the system. The time needed for reconstruction was between 3 to 25 minutes. The large variation in that time is mostly due to different levels of figure quality.
The reconstructions were analysed for the same quantitative parameters as those obtained from the 2D system. The bifurcation lesions were classified based on the 3D information and the findings compared with those from 2D. In terms of a 3D geometrical analysis, the angulations between the proximal main branch and side branch and between the distal main branch and side branch were noted, as presented by the system as a part of the bifurcation analysis. After stenting, it was possible to analyse only those cases in which at least two different projections of the bifurcation were available. This evaluation included a quantitative assessment of residual lesions as well as a geometrical assessment of angulation and comparison with the pre-stenting findings.
Statistical analysis
Means and standard deviations of sets of data are presented. Differences between continuous variables were analysed with t-tests. One-sided or two-sided tests were used as appropriate, and the significance threshold was set at p<0.05. BMDP statistical software was used for all analyses8.
Results
On 2D analysis, the distribution of the bifurcations according to the Paris classification was as follows: type I- 10 patients; type II- 4 patients; type III- 5 patients; type IV- 8 patients. The main branch was involved in 88% of cases; side branch involvement was found in 70%.
Of the 27 bifurcations studied, 26 were successfully reconstructed (Figure 2); in the remaining case, the lesion area was poorly represented by the chosen angles of projection.
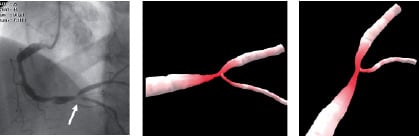
Figure 2. 3D reconstruction of coronary bifurcation lesion. 2D coronary angiography of the right coronary artery from the left-anterior oblique projection and 3D reconstructions from various projections.
In 25 of the 26 reconstructed bifurcations, there was complete agreement in bifurcation classification between the 2D analysis and the 3D reconstruction. In one case, a lesion was classified type III (involvement of only the proximal main branch) on 2D analysis and type II (significant lesions in both the proximal and distal main branch) on 3D reconstruction.
In 8 of the 26 reconstructed bifurcations there were not enough projections after stenting had been performed. As a result there was no ability to perform 3D reconstruction and to include those cases in the post-stenting analysis. Eighteen patients were included in the pre- and post-stenting 3D comparison (Table 2).
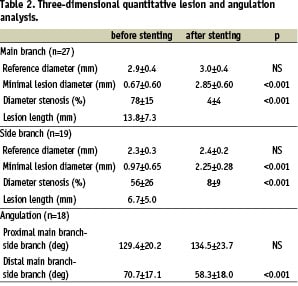
The results show that the angulation between the distal main branch and side branch was 71±17° before stenting and 58±18° after; this difference was statistically significant (p<0.001). Subgroup analysis of angulation changes after stenting, between the distal main branch and side branch, showed for most of the groups a statistically significant or a trend for decrease in angulation (Table 3).
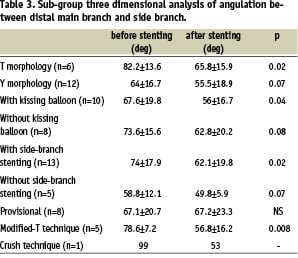
Importantly, in the eight cases where provisional stenting was the approach and the side branch was not stented, there was not even a small change in angulation. There was only one case, using the crush technique, that was examined both before and after stenting (Figure 3A).
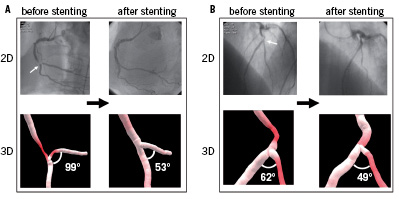
Figure 3. 3D reconstructions and angulation changes after stenting. A: A bifurcation lesion in the right coronary artery. The lesion was treated with crush technique with a significant decrease in the angle between the distal main branch and the side branch. B: A bifurcation lesion in the left-anterior-descending artery. The lesion was treated with a provisional technique without significant angulation angle change.
In this case, an enormous decrease in angulation was observed, although no statistical information can be derived. In terms of the angulation between the proximal main branch and the side branch before and after stenting, no significant change was found (129±20° and 135±24°, respectively).
Discussion
Since the early days of interventional cardiology, management of bifurcation lesions has been extremely difficult9-11. The anatomy of bifurcations is complex, comprising three segments (proximal main branch, distal main branch and side branch) that have an independent path in space. The relative dimensions of each segment and angulations between the branches are important haemodynamic factors. The wide variability of plaque distribution makes the scenario even more complex. Furthermore, any therapeutic strategy adopted in one branch will affect the other branches. Balloon inflation or stent placement can cause a considerable change in lesion distribution or “plaque shift”12,13.
The proper diagnosis and treatment of bifurcation lesions requires optimal angiographic techniques. The 2D angiography in current use can provide only an approximation of lesion stenosis, and length measurements are prone to some degree of foreshortening14. 2D angiography is also incapable of delineating the true curvilinear path in space of the segments and the angulations between them. Despite the introduction of numerous bifurcation intervention techniques in the last decade (kissing balloon, T stenting, modified T stenting, provisional stenting, culotte stenting, and the “crush technique”)15-21, outcomes will remain less than optimal unless imaging methods are improved.
Prompted by these findings, Paieon Inc. developed a novel system for the three dimensional reconstruction of bifurcation lesions. Using this system, interventional cardiologists can examine the complexity of each bifurcation in terms of geometry and lesion distribution. Such information has the potential to provide interventionalists with a sound basis for clinical decision-making. This is particularly important when the value of stenting the side branch is unclear22-25.
It has been previously noted that geometrical changes that occur after stenting could pose an increased risk for restenosis in that area26,27. An important finding in this study, which according to our knowledge was not reported yet in the literature, is the significant anatomical change that occurs in a bifurcation after stenting. After stenting there was a statistically significant decrease in the angle between the distal main branch and the side branch. This decrease in angulation appeared in all subgroups except for the group where provisional stenting was the approach and the side branch was not stented. The effect of this anatomical change and its possible correlation with higher restenosis rates requires further study.
Limitations of the study
There was only small number of bifurcations examined. Further investigation in a larger population is needed to corroborate the findings as well as the impact of post-stenting anatomical changes. An additional study should be performed to evaluate the contribution of the geometrical and quantitative information provided by the 3D system to clinical decision making in real time.
Conclusion
3D reconstruction provides new insight into the geometry of bifurcation lesions and may serve as an important tool for planning interventional procedures and evaluating their results. The implications of the demonstrated angulation changes after stenting should be further evaluated.

