Since its earlier days, procedural and technical difficulties allied to poor immediate and long-term outcomes have turned the percutaneous treatment of bifurcated coronary lesions into one of the most challenging scenarios of interventional cardiology1,2.
In the mid 1980’s, when balloon angioplasty was the standard percutaneous approach, the treatment of bifurcation lesions was considered a procedure of exception for carrying a high risk of acute ischaemic complications (e.g. acute coronary thrombosis) and restenosis. Usually, kissing-balloon was the preferred technique to minimise plaque shift to the side branch and improve immediate outcomes3,4.
In the early 1990’s, the use athero-ablative techniques (rotational and directional atherectomy) decreased the need for repeat lesion revascularisation but increased the procedural complications after percutaneous approach of bifurcations5-7.
In the mid 1990’s, coronary stenting, through its scaffolding properties, became the treatment of choice for bifurcated lesions, mainly because of its impact in reducing acute complications. However, it was yet to be determined which was the best technical approach to reduce restenosis and improve long term outcomes in that specific population. Basically, the remaining issue was how to achieve the best results in the main branch while preserving the side branch. In the bare metal stent era, several reports investigating the outcome of stenting solely the main vessel versus stenting main vessel and side branches, reported dissimilar results; although both techniques proved to be safe and feasible, substantial restenosis rates of up to 40% were observed8,9. Of note, among those receiving stents in both branches, T-stenting was superior to Y-stenting in reducing adverse events (86.3% vs. 30.4%, p=0.004).
For several years now the advent of drug-eluting stents has significantly lowered the restenosis rates following the percutaneous treatment of coronary atherosclerotic disease in virtually all subgroups of patients and lesions. Also, new guiding catheters, low profile balloons and the dual antiplatelet therapy (association of thienopyridines and aspirin), have improved the clinical and angiographic results of these procedures. However, the preliminary data on DES in bifurcations are mainly based on small sub-studies, most of them with sirolimus-eluting stents. Pan et al reported in 2004 their experience with Cypher for treatment of 91 “true” bifurcations, comparing a simple approach (stenting the main vessel and balloon dilatation for the side branch) to a complex approach (stents for both vessels)10. Although restenosis rates were slightly lower among the patients treated with the simple approach, no difference in clinical outcomes was observed, probably due to the small sample size. Colombo et al, in the SIRIUS-bifurcation study, compared the two strategies (stent in the main vessel versus stent in the main and side branches) in 86 patients with bifurcated lesions11. They concluded that sirolimus-eluting stents effectively reduced restenosis and target lesion revascularisation rates and that there was no clear advantage in stenting both branches. However, the deployment of the second stent (in the side branch) was difficult to avoid in most of the cases due to poor acute results (dissections and/or significant residual lesions) at the ostium of that branch. More recently, Ge et al compared two contemporary bifurcation approaches – T-stenting and “crush” – using drug-eluting stents12. In their analysis, crush stenting with final kissing balloon post-dilatation was associated with a reduced rate of restenosis in the side branch when compared with the T stenting technique. Importantly, in bifurcation lesions treated with drug eluting stents, the restenosis rate remained relatively high in the side branch. Recently, Steigen et al published the results of the Nordic Bifurcation Study, showing that the simple strategy of stenting only the main vessel was associated with reduced procedure and fluoroscopy times and lower rates of procedure related biomarker elevation, with equivalent long term target lesion revascularisation rate when compared to the strategy of stenting main and side branches13.
But what makes the percutaneous treatment of coronary bifurcations so cumbersome? Although the estimated involvement of “true” bifurcations in the coronary artery disease is in the order of 15 to 25%, experienced operators usually say that “you never really face two identical bifurcations”. Figure 1 illustrates the three most accepted classifications of bifurcated lesions. Special attention should be paid to Medina’s classification, currently the prevalent classification, due to its simple, logical and comprehensive way to classify bifurcation lesions. Nevertheless, it is not rare to find in the clinical scenario a case difficult to fit in one of these types.
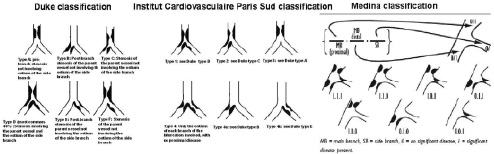
Figure 1. Despite the numerous classifications currently available for bifurcation lesions, these three are probably the most representative ones, with special emphasis to the Medina classification, the easiest to memorise and the one which better correlates with clinical outcomes after percutaneous interventions.
Moreover, the angle formed by the main and side vessels can vary considerably and play an important role, not only in limiting the acute success of the procedure, but also influencing the long-term outcomes. Other potential issues that can increase the duration and complexity of the procedure and impair the short and long term success when dealing with these lesions are:
1. Use of 2 guide wires: It demands more attention on the part of the main operator regarding the relationship between the wires, the main branch (MB) and the side branch (SB) in order to avoid confusion, delays and loss of position during the procedure.
2. Positioning of the guidewire through the side branch: It is a frequent problem, especially when we face T-shaped lesions, narrowed side branch (diameter less than 2.0 mm), proximal tortuosity and suboclusive ostial lesions.
3. “Snow-Plow effect”: it is frequently observed after the treatment of Y-shaped and “false” bifurcation lesions. The occlusion of an unprotected side branch under this circumstance could represent its permanent loss and impair the outcomes of the intervention.
4. Failure in re-crossing the guidewire, the balloon or a second stent through the struts of the first stent delivered in the main branch: The inability to access the side branch would prevent the “kissing” balloon post dilatation, a highly recommended final step in the treatment of bifurcation lesions.
In an attempt to overcome these problems, a variety of techniques were developed in recent years (Figure 2). Currently, in our Institute, “V”, “Y” and “simultaneous kissing-stent” (SKS) techniques, with the deployment of two or more DES, are preferred to treat “true” bifurcation lesions when main and side branchs have a reasonable size (> 2.5 mm) and their ostium have important disease (% of stenosis > 50%). For all the other scenarios, stenting the main vessel and “provisional” stent in the side branch is the favoured approach in our service with reduced costs and at least comparable long term results.
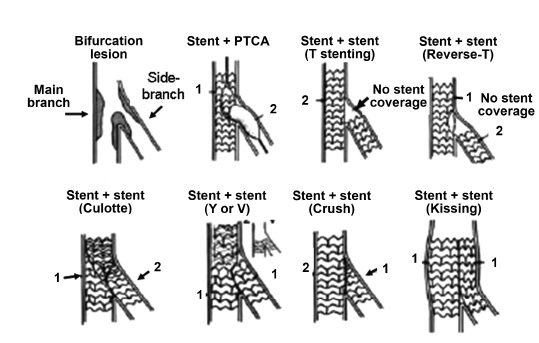
Figure 2. A schematic representation of different percutaneous approaches to “true” bifurcation lesions. The use of a stent in the main branch and balloon angioplasty (a “provisional” stent) in the side branch remains the most cost-effective approach whenever non-dedicated stents are used to treat these type of lesion.
Some limitations and risks of the above-mentioned techniques are:
1. Side branch jailing
2. Failure to wire the side branch through the stent struts
3. Inability to pass the balloon through the stent struts
4. Inability of the single cell to withstand balloon side branch dilatation
5. Inability to scaffold the ostium of the side branch
6. Inability of the stent structure to withstand balloon side branch dilatation.
The limitations of these approaches have increased the necessity to continue improving the search for the ideal treatment to bifurcated lesions. Instead of “rebuilding” the bifurcation and struggling to achieve an optimal final geometry of both main and side branch with conventional stenting techniques, a first generation of dedicated bifurcation stents was developed. However, their deployment was challenging, demanding the placement of two guidewires in each of the branches in order to allow a smooth advancement and delivery of the 2 distal modules of the stents to their respective sites14. Besides, they were “stiff” and not flexible making them hard to deliver. As a result, the initial clinical experience with these platforms was not very encouraging.
Even so, it is still a belief among those who frequently battle with bifurcations that a dedicated bifurcated stent is the definite response to the technical demands of this subset of lesions. Based on this credence, a new generation of dedicated bifurcated stents, some eluted with antiproliferative drugs, have been recently developed and tested.
Currently, there are three major types of stents dedicated to bifurcations:
1. Pre-formed stents with side ports to facilitate the access to the side branch after treating the main vessel (e.g. Ariste, SLK view, Invatec, etc.);
2. Conical stents for the geometry of the ostium (e.g. Axxess, Nile CroCo, Petal, etc);
3. Stents designed to treat the side branch first (e.g. Sideguard, Tryton, etc.).
Yet, different stent delivery systems providing permanent access to the side branch or allowing reliable stenting (and final “kissing balloon” dilatation) of the side branch ostium have also been developed lately. In this group, the most representative example is the Y-med sidekick (Y-med Inc), comprising a 6 Fr guide compatible stent delivery system with a rapid exchange steerable guidewire with a fixed-wire platform designed to preserve side branch access during bifurcation stenting. A First-in-Man study with this new delivery system is currently ongoing, led by Dr Eberhard Grube.
Next, we will describe the most recently developed bifurcated stents and whenever available, their preliminary clinical results. It is important to keep in mind that most of the numbers presented in the next paragraphs came from oral communications during major international meetings and symposium and have not yet been published. Table 1 summarises the main characteristics of each of the mentioned stents.
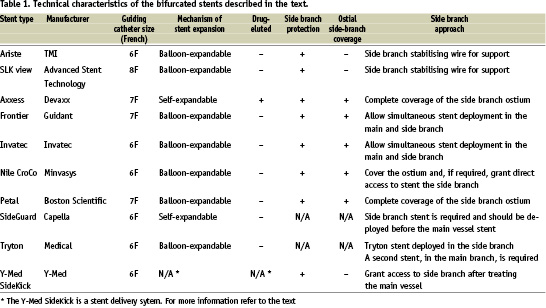
Ariste stent (TMI)
This side branch adaptive stent is comprised of a balloon expandable 316L stainless steel stent with a side branch support structure in the centre of the stent, a rapid-exchange balloon catheter, and a side branch stabilising wire (SSW) ready to use and encased in a peel-away lumen to minimise wire crossing, a common procedural complication associated with bifurcation cases. The stent is delivered using a single balloon catheter on a 0.014” main lumen guidewire. Four markers on the side branch support structure of the stent help with positioning and orienting the stent at the bifurcation (Figure 3). As the stent approaches the targeted bifurcation, the operator may torque the catheter to align stent central opening with the side branch ostium using the radiopaque tantalum markers as a guide. Due to advanced stent design, stent deployment is achieved using a single balloon, thus the profile is comparable or smaller than conventional DES (such as Cypher). The side branch support portion of the stent is automatically deployed as the main body of the stent expands. The side branch support structure is equipped with markers that, after deployment, help with positioning of a second stent in the side branch. It is available in diameters from 3.0 to 4.5 mm (main vessel) and 2.0 to 3.5 mm (side vessel) and it is 6 Fr compatible.
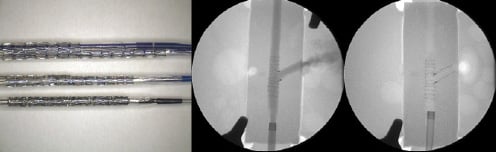
Figure 3. On the left, a picture of the Ariste system with the stent for the main vessel and a central aperture with four markers to allow the approach of the side branch for a final “kissing” balloon dilatation, or eventually for the deployment of a second stent in that position as illustrated on the angiogram (seen in the central and right panels).
AST SLK-View™ (Advanced Stent Technology)
This over-the wire system consists of a 316 L stainless steel flexible slotted-tube stent with a side aperture located at the middle segment of the platform. It has two guidewire lumens and one lumen for inflation of the balloon. The main branch guidewire lumen is located at the tip of the balloon catheter. The side branch wire lumen is parallel to this one and protects the wire during its passage between the balloon and the crimped stent. At the distal end of the delivery system there is an expandable 20 mm-balloon with the crimped stent. Three gold radio-opaque markers can be identified at the proximal end, middle and distal end of the balloon respectively. The presence of the side hole was conceived to allow the placement of a stabilising catheter and provide access to side branch after stenting the main vessel (Figure 4). This system requires an 8 French catheter and it is available in two diameters – 3.0 mm with 2.5 mm side hole and 3.5 mm with 3.0 mm side hole – and a single length (17 mm). Although the procedural success rates were high and varied between 87% and 98%, binary restenosis was observed in up to 28.3% of the main vessels and 37.7% of the side branches16.

Figure 4. Similar to the Ariste stent, the AST SLK-view system consists of a slotted stainless steel platform with a side hole in its middle portion to facilitate the access to the side branch. The proximal and distal edges of the stent, as well as the middle aperture, are identified by gold radio-opaque markers.
Despite the favourable initial reports regarding procedural success and safety, the AST SLK-View stent still needs to be tested in a large cohort. Also, a drug-coated version would certainly be much appreciated.
Axxess™ (Devax, Inc.)
The AXXESS Plus Biolimus A9-coated-stent was the first bifurcated stent designed to elute an anti-restenotic drug. This system consists of a self-expanding Nitinol platform (AXXESS™ stent), a bioabsorbable polymer and a successfully clinically tested anti-proliferative drug, the BiolimusA9™.
The system is deployed at the bifurcation and expands into the main and side branch, providing complete vessel coverage at the level of the carina. With the Axxess stent covering the ostia, branch vessel stents are placed just distal to the bifurcation (Figure 5). Distal stents are implanted in their natural shape, and do not need to be “remodelled” by “kissing-balloon” inflation to fit the anatomy of the bifurcation. The flared shape of the AXXESS stent matches the geometry of most bifurcations.
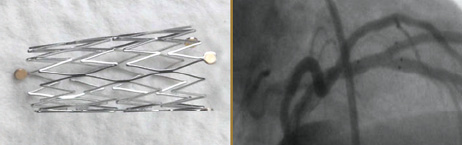
Figure 5. The Axxess Plus system consists of a self expanding nitinol stent with a bioabsorbable polymer eluted with Biolimus A9. The presence of radiopaque markers at the proximal and distal edges of the stent makes the placement of the stent easier. Through the central hole, a second stent can be delivered to complete the treatment of the bifurcation.
Biolimus A9™, the coating drug used in this system, is a new molecular entity (C55H87NO14) that is more lipophilic than Sirolimus™ and Everolimus™. It works as an immunosuppressant binding to FKBP-12 and inhibiting mTOR activity (Figure 6). Its safety and efficacy in the treatment of non-bifurcated lesions has already been demonstrated in the clinical scenario.
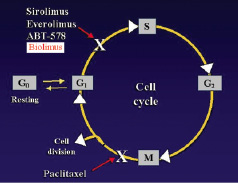
Figure 6. Biolimus A9, a sirolimus analogous, interrupts the cell cycle in the transition from the G1 to the S stage, efficiently blocking in-stent neointimal proliferation.
The multicentre Axxess Plus Clinical Study was designed to evaluate the acute and long-term (12 months) clinical utility of this novel system for the treatment of bifurcated lesions in native coronary vessels, including left main coronary artery. In March of this year, Costa et al presented the midterm follow up results of this study (American College of Cardiology, scientific sessions, 2006). Of the 136 patients enrolled, they reported procedural success in 129 of them (94.9%). Three patients had in-hospital myocardial infarction. When only the AXXESS stent was analysed, the restenosis rate in the main branch was 4.8% When a second DES was placed in the side branch the restenosis rate was 7.9%. When only balloon angioplasty was performed in the side branch, the restenosis rate was significantly higher (25%). When no additional procedure was considered to the side branch, the restenosis was around 12%. However, in 80% of the cases, an additional drug eluting stent was required to be deployed distal in the main or side branch. When they were included in the analysis, the restenosis rate in the main vessel increased to 11.9% and in the side vessel to 14.3%. Overall, this result was considered very encouraging and far better than any reported series using non-dedicated drug-coated stents for the treatment of bifurcated lesions.
Multilink Frontier (Abbott Corp.)
This new system was designed for preserving side branch access. Its integrated-tip design allows single tip delivery, avoiding wire wrap. Wire position is maintained in both branches throughout the procedure (Figure 7). Furthermore, it allows stent deployment by simultaneous “kissing balloon inflation”, and optimal main branch and side branch ostium scaffolding.
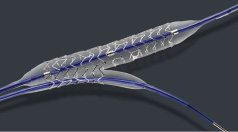
Figure 7. Multilink Frontier is another system that has a side hole to allow easier access to the side branch. It is a 7F non-eluted platform with two wires (main and side branch) and the central aperture as illustrated here.
This novel platform is available in diameters from 2.5 to 4.0 mm for the main branch and 2.0-2.5 mm for the side branch and in the single length of 18 mm. Its current version is 7.0 French compatible.
Lefreve et al published in 2005 the results of the multicentre FRONTIER Stent Registry, which evaluated the incidence of combined MACE (primary endpoint), as well as device success rate and target lesion revascularisation (secondary endpoints) in the period of 180 days17. They reported a procedure success rate of 93%. Two patients presented in-hospital acute myocardial infarction secondary to side branch occlusion during the procedure. At six months, the MACE rate was 17.1%, mostly due to target lesion revascularisation TLR (13.3%). Importantly, no subacute stent thrombosis or death was reported.
Based on the enthusiastic preliminary results of this system, a drug-coated version of this platform is expected to be soon available.
The Invatec system (Invatec)
The Invatec bifurcation stent has either a single or double balloon stent delivery system that aims to provide easy access for provisional T- stenting.
This stent delivery system can reach a precise positioning of the side cell, correctly facing the side branch through its axial self-positioning and rotational self-positioning properties. The axial self-positioning property features a “stopper” to position the side cell at the side branch level. The rotational self-positioning property allows the delivery system to automatically turn the side cell exactly towards the side branch (Figure 8).

Figure 8. The Invatec “twin rail” 6F system consists of a single catheter splitting into two distal balloons with a central “stopper” to make the stent positioning easier. The side aperture allows simultaneous “kissing balloon” or “kissing stent” if necessary to stent the side branch.
The double-balloon system is quite similar to the Multilink Frontier except for the fact that the side-balloon here is a full dilatation balloon to be used for the kissing-balloon technique whereas in that other system the stent has a short tapered side branch balloon.
Both systems (single and double balloon) have been compared in a randomised, prospective way in the “Double versus single balloon stent delivery systems for bifurcation lesions” or Desire Study. In a preliminary report (A. Colombo, Joint Interventional Meeting – JIM, Milano, 2004), a total of 34 patients had already been enrolled and completed the 6-month follow-up. Procedure success was obtained in 94% of the cases. At the end of 30 days, no major event was observed. However at 6-month follow-up, the overall restenosis rate was 33% with 19% of target vessel revascularisation. No comparison data between single and double balloon strategies was presented at that time.
Nile CroCo™ (Minvasys)
This is a single operator device with two independent, yet joined together catheters (Figure 9). It requires independent catheter manipulation and pressure monitoring. The postulated advantages are that the system allows: Instant post stent “kissing-balloon” dilatation; optional side branch stenting; high stability within main artery and direct access to side branch vessel; low balloon profile and unique side branch tip design for better crossability treating up to 90º angulated lesions; and finally, that it is a real 6 French compatible system for faster and safer procedure.
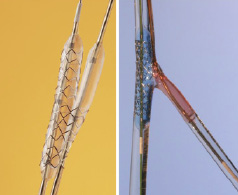
Figure 9. The Nile CroCo platform was conceived with a balloon catheter (for side branch dilatation) and a stent (for main branch treatment) mounted on the same system allowing very fast “kissing” balloon dilatation post stent deployment. Additionally, it is a 6F compatible device.
This cobalt chromium device is available in diameters ranging from 2.5 to 3.5 mm for the main branch and 2.0 to 3.0 mm for the side branch and in the single length of 18 mm.
This feasibility and effectiveness of this device is currently being evaluated in a multicentre European registry with Drs. Lefèvre and Pavlides as principal investigators. Preliminary data from the first 75 patients enrolled showed 95% of procedure success. Final kissing balloon dilatation was performed in 93% of them. Interestingly, total time of the procedure was on the average inferior to 30 minutes (27.5±14.2 minutes).
Petal™ (Boston Scientific Corp.)
The newly developed Petal™ system, with a side aperture and deployable struts, has come as an attractive solution to the frequent problem of side branch occlusion caused by vessel deformation and plaque shift when we approach coronary bifurcations (Figure 10). Coronary stents with a side aperture and a sleeve may be clinically advantageous to maintain access to the side branch, stabilise the side-branch orifice, and deliver the appropriate drug to the side-branch ostium.
As for now, a paucity of clinical studies and lack of a drug-coated version are the major limitations of this platform.

Figure 10. The Petal system is another example of a device designed with a side aperture to approach the side branch during bifurcation treatment. As an increment, this stent has deployable struts (a “sleeve”) in the side hole, conceived to deal with the “snow-plow” and ostium deformation, often seen after stenting the main branch.
Sideguard™ (Cappella)
This Nitinol self-expanding device embraces the philosophy of stenting one vessel at a time. While conventional approaches for treating bifurcation are to stent the main branch first, try to preserve the side branch ostium using balloon technique, and then place a second stent, the Sideguard approaches bifurcations from a complete different angle, using a low-profile (less than 3.5 Fr), single catheter delivery system that does not require rotation (Figure 11). Its short length, flexible and self-expandable design grant this platform better navigability, even in the presence of calcified side branch ostium, optimising scaffolding, helping to preserve the lumen geometry of the bifurcation, and minimising the trauma on the vessel wall – all major predictors of poor clinical outcomes. The next generation of this device is intended to be coated with an anti-restenotic drug carried on a biodegradable polymer.
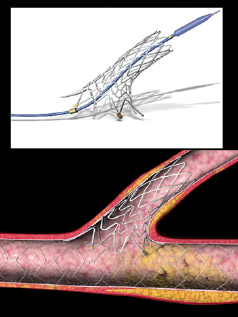
Figure 11. The Sideguard, a short, self-expandable nitinol system, was designed to approach very angulated and calcified lesions. The gold markers at the proximal edge facilitate positioning this stent at the “true” ostium.
Tryton (Medical Inc.)
This cobalt chromium stent has been designed to provide effective treatment to bifurcation lesions with a comparable coverage and radial strength as that available with new generation stents used in straight lesions. The Tryton side-branch stent is unique in that it is delivered using a single guidewire and does not require any rotational orientation. In addition, this device has been designed to treat all anatomically significant angles of bifurcated lesions. It consists of three zones: (1) a side branch zone; (2) an intermediate zone placed within the ostium of side branch, and; (3) a main branch zone (Figure 12). The cobalt chromium alloy provides a high flexibility combined to a low profile also granting to the stent moderate radiopacity without obscuring the lesion area during its positioning. It is mounted on a 5F guiding catheter compatible balloon-expandable system with six markers (four radiopaque markers within the distal balloon region and two proximal shaft markers). This system has a unique approach to the bifurcation lesion: the Tryton stent is first deployed across the side branch ostium with the side branch zone in the side branch and the main branch zone residing in the main vessel. The operator then selects and deploys the ‘work-horse’ of his choice across the lesion from the main branch zone of the Tryton stent, and distal to the bifurcation, to complete the lesion coverage in the main vessel.
After encouraging initial results in animal models, a First-in-Man study (TRYTON I) is currently ongoing with the first 20 patients treated with 100% of procedure success.
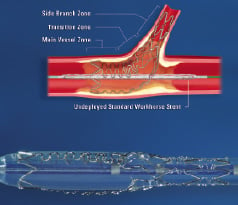
Figure 12. The Tryton system (on the left) consists of a cobalt-chromium stent with three zones to approach “true” bifurcation lesions. This system approaches the bifurcation in a “non-conventional” way, first treating the side branch and then the main vessel (please refer to the text to further details).
Conclusions
The percutaneous treatment of bifurcations is considerably more cumbersome, time-consuming, and expensive.
Current bifurcation techniques (even with DES) do not provide the same long-term efficacy observed for non-bifurcation lesions.
The new generation of dedicated stents specifically designed for bifurcations might be the solution in the near future. However, further clinical studies and the development of more drug-eluted platforms is mandatory to make them the first choice to approach coronary bifurcations.