After a long hiatus, we can finally declare that major cardiology conferences worldwide have more or less returned to normal. However, what is noticeable is that the notion of “normality” now differs from conference to conference (“in person” only, “remote only”, “blended”, etc.). It is a widely shared opinion that in-person conferences have an extra spark of enthusiasm and participation. Simply having to step out of the daily routine to attend these events makes for a more enjoyable experience than quickly presenting content remotely, with the day’s busy schedule accumulating outside the door.
However, the prevailing feeling is that having the option to choose is now the best course of action. For example, the CRT conference in Washington DC and the ACC Congress in New Orleans, LA, both in the US, took place within a week of each other, in late February and early March. Nowadays, it may be challenging for attendees from Europe to participate in both events, since they are just seven days apart, potentially requiring two transatlantic journeys (never mind the time and resources). Of course, there are exceptions: my Twitter feed during those days showed clearly that some colleagues stayed in the US after the CRT meeting to attend the ACC annual conference, while others actually travelled twice.
In my case, I opted to attend one meeting in person and one remotely, and I greatly appreciated that the American College of Cardiology allowed me to choose my preferred modality at the time of the invitation. Not all congresses offer this option, but maybe they should, as the blended mode is nonetheless a valuable educational opportunity, as we have learned during the pandemic years. It would be a missed opportunity to return to the old ways and forego such options. In my humble opinion, congress organisers should carefully consider this option for the future, thus expanding their faculty and audience, reaching as many people as possible.
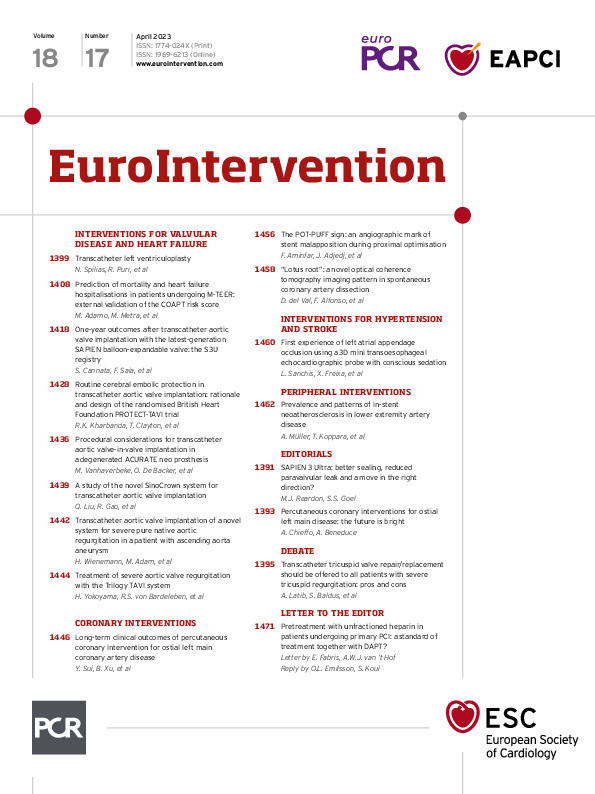
After this brief and personal reflection, let us move on to the review of the articles in this issue of the Journal. As usual, I wish you an enjoyable reading experience.
Let’s begin with the next instalment of our popular debate series. This time we tackle the subject of whether transcatheter tricuspid valve repair/replacement (TTVR) should be offered to all patients with severe tricuspid regurgitation. Given the low complication rates and improved quality of life that TTVR can offer, Azeem Latib and Antonio Mangieri argue that TTVR should be offered to all patients, even if only a modest reduction in tricuspid regurgitation is achieved. Additionally, the ineffectiveness of diuretic and other medical therapies as well as the high risk of isolated tricuspid regurgitation surgery contribute to their other reasonings. While Stephan Baldus and Felix Sebastian Nettersheim agree on the broad points, they argue that TTVR can be deferred in certain conditions when the causes of tricuspid regurgitation are treatable by means other than TTVR, such as in left heart disease, severe pulmonary hypertension and atrial fibrillation.
We now turn to an expert review by Nikolaos Spilias, Rishi Puri and colleagues on transcatheter left ventriculoplasty. With ever-increasing numbers in the heart failure population, there is an unmet need in novel therapeutic approaches. Interventional heart failure therapy is an emerging field that uses minimally invasive techniques for structural heart interventions. The authors address the rationale for left ventriculoplasty and present a history of the surgical and percutaneous attempts in the field. They provide an overview of novel transcatheter left ventriculoplasty devices and their respective trials, and they highlight the challenges associated with establishing such device-based therapies.
To continue, Marianna Adamo, Marco Metra and colleagues present the first external validation of the COAPT (Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation) risk score. Based on four clinical and four echocardiographic variables, the COAPT risk score was derived from the COAPT trial to predict two-year all-cause death or heart failure hospitalisation in patients undergoing mitral transcatheter edge-to-edge repair for secondary mitral regurgitation.
Next, Stefano Cannata, Francesco Saia and colleagues compare the one-year clinical and echocardiographic outcomes of transcatheter aortic valve implantation (TAVI) with the newest balloon-expandable SAPIEN 3 Ultra transcatheter heart valve versus its predecessor, the SAPIEN 3, in the S3U registry. Although the clinical outcomes were similar at one year between the two devices, they found that the significantly reduced rates of paravalvular leakage with the SAPIEN 3 Ultra, already seen at 30 days, were maintained at one year. Further studies with longer-term follow-up are needed to assess the potential impact of reduced paravalvular leakage rates on clinical outcomes. This article is accompanied by an editorial by Michael J. Reardon and Sachin S. Goel.
Rajesh K. Kharbanda and Tim Clayton, on behalf of the BHF PROTECT-TAVI trial investigators, describe the rationale and design behind the randomised British Heart Foundation’s PROTECT-TAVI trial. In this ongoing UK-based trial, they are studying whether the routine use of the SENTINEL cerebral embolic device (CEP) reduces the incidence of stroke in patients with severe aortic stenosis undergoing TAVI, as well as the safety, efficacy and cost-effectiveness of the technique. With 7,730 patients randomised to TAVI with or without the CEP device, the primary endpoint is stroke at 72 hours post-TAVI. The principal results are expected in 2025.
In the first of two research correspondences, Maarten Vanhaverbeke, Ole De Backer and colleagues report on the planning and execution of a transcatheter aortic valve in transcatheter aortic valve (TAV-in-TAV) procedure to treat a degenerated ACURATE neo bioprosthesis in a 74-year-old male. Using meticulous preprocedural multislice computed tomography analysis, they identified the optimal second transcatheter heart valve implant position and height and implanted a 26 mm balloon-expandable SAPIEN 3 under rapid pacing, resulting in good valve haemodynamics and coronary access.
In the second research correspondence, Qingrong Liu, Runlin Gao and colleagues describe their initial experiences with the SinoCrown valve. This novel self-expanding valve, with a nitinol stent and three valve leaflets made of bovine pericardial tissue, has a hanging connection design that allows it to be fully retrievable and repositionable. Implanted in ten patients through either transfemoral or transapical pathways, there were no deaths, disabling strokes, myocardial infarctions, conversions to surgery, or major procedure-related complications at 30 days. Further studies with larger cohorts and longer-term follow-up are warranted.
Next, we move to coronary interventions, where Yonggang Sui, Bo Xu and colleagues investigate the long-term clinical outcomes and risk factors for adverse events in isolated left main ostial lesions, compared with mid-shaft or distal left main bifurcation lesions, following drug-eluting stent implantation. In a registry of over 4,600 patients, left main ostial lesions were found in nearly 14% of patients. With a primary endpoint of target vessel failure, they found that the long-term prognosis of ostial left main lesions following a percutaneous coronary intervention (PCI) is favourable; when compared with the mid-shaft lesion group, the risk of myocardial infarction was similar but was significantly lower when compared with the distal bifurcation lesion group. Improved technique and devices that avoid procedural complications might improve the prognosis of patients receiving PCI for ostial left main diseases. This article is accompanied by an editorial by Alaide Chieffo and Alessandro Beneduce.
Farhang Aminfar, Julien Adjedj and colleagues describe the creation of the POT-PUFF sign, an angiographic sign for identifying stent malapposition in the mother branch. They hypothesised that the successful progression of contrast medium (PUFF) through an inflated proximal optimisation technique (POT) balloon could better detect stent malapposition than optical coherence tomography (OCT). While the effectiveness of the POT-PUFF sign was reduced for severe malapposition, the specificity and negative predictive values were over 90%, and the POT-PUFF sign could be relied upon to rule out stent malapposition.
In peripheral interventions, Arne M. Müller, Tobias Koppara and colleagues evaluate the prevalence of in-stent neoatherosclerosis in patients with symptomatic in-stent restenosis of the lower limb vasculature through the use of intravascular OCT imaging. In-stent neoatherosclerosis formation, predominantly thick-cap fibroatheroma, was found in 76.7% of the studied lesions, and its extent and frequency was associated with the length of time since stent implantation. The authors suggest that the identification of OCT patterns indicating neoatherosclerosis in the aftermath of lower limb stent implantation might be helpful in the development of mitigation strategies.
And now for more thoughts on novel experiences and clinical insights, let’s turn to the articles themselves.