Transcatheter aortic valve replacement (TAVR) has evolved from a last resort therapy to the standard treatment of patients with severe aortic stenosis and high risk for conventional surgery1 and has shown comparable outcomes in intermediate-risk patients2. Improvements to available transcatheter heart valves (THV), the introduction of new technologies, expansion of indication to lower-risk cohorts and increasing operator experience have resulted in a considerable decline in one-year mortality rates to below 10%3.
Despite these improvements, several issues remain to be addressed. Among these is the problem of new permanent pacemaker implantations (PPI) and new-onset conduction abnormalities (CA) after TAVI, which has led to controversial discussion. While some investigations found no effect of PPI on mortality4,5, a recent analysis from the PARTNER trial identified chronic pacing as an independent predictor of one-year mortality after TAVI6,7. In parallel, new-onset CA, especially new left bundle branch block (LBBB), were associated with lack of improvement in left ventricular function8 and increased cardiac mortality4. Therefore, a reduction in new PPI rates is of paramount importance, especially with the possible extension of indications towards younger, lower-risk populations. In this regard, the pursuit to improve THV performance with minimisation of paravalvular leakage (PVL) but not at the expense of increasing rates of PPI and new-onset CA has been aptly compared to “sailing between Scylla and Charybdis”9. Indeed, among the so-called “next-generation” THV, the device with the lowest rate of PVL in the field, the LOTUS™ valve (Boston Scientific, Marlborough, MA, USA), also displays the highest rate of PPI10. Therefore, careful iterations of devices and careful appreciation of implantation techniques appear warranted.
Determinants of PPI and new-onset CA after TAVR are manyfold and include more patient-related factors, device-related factors and possibly operator-related factors. Among the former are predominantly a pre-existing complete right bundle branch block (RBBB), age and gender, while the latter include the type of THV used, depth of implantation and prosthesis oversizing11,12. Although the patient-related factors are given, operator- and device-related factors can be influenced. Traditionally, the PPI rate has been considerably higher with self-expanding compared to balloon-expandable THV13.
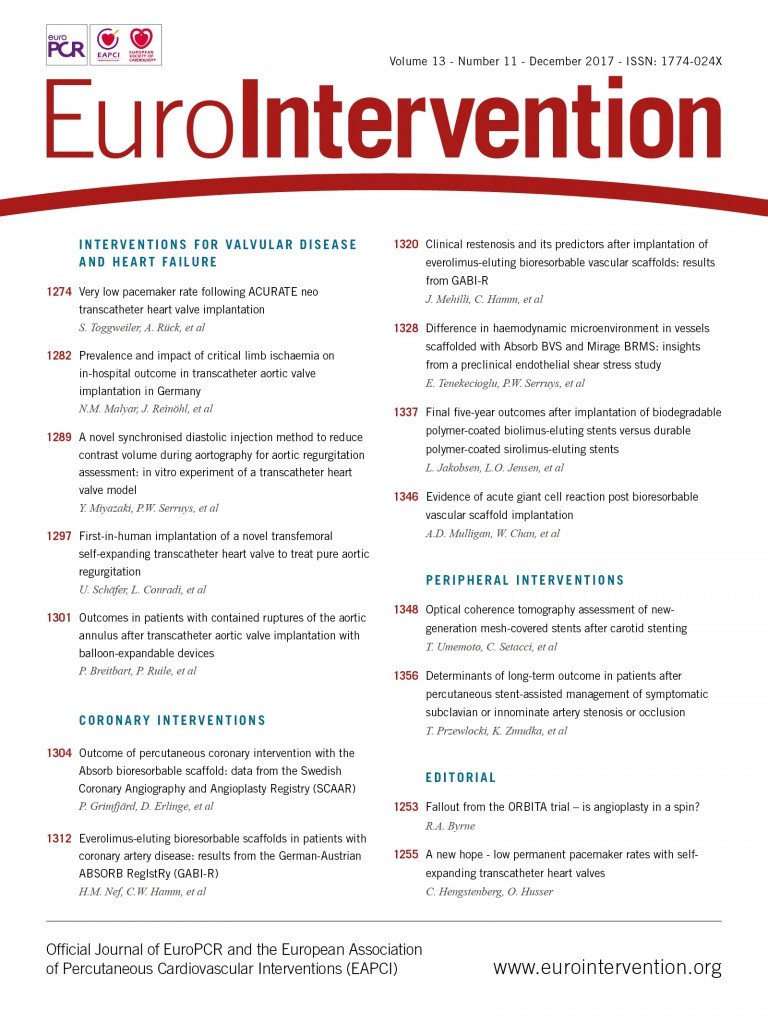
In this issue of EuroIntervention, an international collaboration of Swiss, Swedish and Danish investigators led by Stefan Toggweiler assessed the effect of a careful implementation of implantation techniques on the PPI rate with a novel self-expanding THV, the ACURATE neo™ (Boston Scientific)14.
The ACURATE neo received CE mark approval in 2014. It consists of a self-expanding nitinol frame with a porcine pericardial leaflet valve in a supra-annular position and a pericardial sealing skirt on the outer and inner surface of the stent body. In the present study, 175 patients were included from three European high-volume TAVR centres. In all patients, a conservative balloon predilatation strategy using a balloon about 2 mm smaller than the perimeter-derived annulus size was pursued with the aim of minimising trauma to the conduction system. Prosthesis size selection was performed as recommended by the manufacturer; however, in the case of a borderline value, the larger THV was always selected, resulting in a mean prosthesis oversizing of 1.4 mm. Post-dilatation was only performed in the case of significant PVL and was only used in 26% of the cases. Using this strategy, the rate of PPI was remarkably low at only 2.3% of the cases, corresponding to four patients. Baseline PPI risk of the patients treated was comparable to other populations with a prevalence of pre-existing RBBB in 9% of the cases. Other significant risk factors for PPI were diabetes, beta-blockers at baseline and a lower mean transaortic gradient. When analysing these cases more closely, it became evident that, out of these four patients with new PPI, three had pre-existing RBBB, being exactly the patient-related factor which is known to have the highest risk for PPI11,15. In two of those four patients, the development of high-degree AV block was observed a few days after the implantation. This is of great importance when discussing both the performance of TAVR in intermediate-risk patients and (very) early discharge.
There are some aspects of the present study that are noteworthy. First, data on PPI and new-onset CA with the ACURATE neo are relatively rare and the PPI rate in this study is one of the lowest observed with TAVR so far. Rates of new PPI at 30 days and one year with the ACURATE neo were 10.3% and 11.5%, respectively16, and in the post-market registry SAVI-TF 1000 the PPI rate was 8.2% (Möllmann H. 30-day registry results using a second-generation TF-TAVI system for the treatment of aortic stenosis. Presented at EuroPCR 2016, Paris, France). Recently, in the MORENA registry, a propensity-matched multicentre comparison of ACURATE neo with SAPIEN 3 (Edwards Lifesciences, Irvine, CA, USA), the rate of new PPI was 10.2% and significantly lower compared to SAPIEN 317. These data place the ACURATE neo in the lowest ranges of new PPI within the so-called “next generation valves”. Especially the promise of low PPI with the ACURATE neo may prove useful in patients at high risk for PPI such as patients with complete RBBB at baseline15.
Second, this study shows that a careful selection of technical steps may indeed result in a further improvement of PPI rates in TAVR. Indeed, this has also been attempted for the SAPIEN 3, where a higher implantation resulted in lower PPI rates18, and for the LOTUS valve applying the Depth Guard™ technology (Boston Scientific) (Van Mieghem N. Transcatheter Aortic Valve Replacement Using the Lotus Valve with Depth Guard: First Report from the RESPOND Extension Study. Presented at CRT 2017, Washington, DC, February 20, 2017). Balloon valvuloplasty for predilatation itself has been identified as a potential cause of new-onset CA19. Therefore, the concept of Toggweiler and colleagues appears logical to approach the issue of PPI and new-onset CA by modifying the predilatation strategy. Indeed, a recent study went even further by omitting the predilatation completely in 72 (out of 294) patients and observed equal safety and efficacy20. In this examination, however, the rates of new PPI were not reduced by the omission of predilatation. Therefore, the conservative strategy proposed in the present manuscript may offer the ideal approach and requires prospective validation by other groups.
Finally, an important finding is the observation that, using the ACURATE neo, device-related factors, such as implantation depth, prosthesis oversizing, and post-dilatation were not associated with a higher rate of new PPI. This has also been observed in another recent substudy of the MORENA registry (Pellegrini C et al. Predictors of Permanent Pacemaker Implantations and new Conduction Abnormalities using a Next Generation Self-Expanding Transcatheter Heart Valve. https://www.abstractserver.com/dgk2017/ft/abstracts/V120.HTM). Here, the PPI rate was 10% in 225 pacemaker-naive patients treated with the ACURATE neo.
Despite its strengths, the current study has several limitations, which are mostly mentioned in the limitations section of the paper. The study population was relatively small and the low event rate precluded multivariable models to identify predictors of PPI.
Therefore, we may need to limit our enthusiasm and be careful with conclusions drawn from this study regarding this promising PPI rate with this novel self-expanding THV, until more data and experience are available. Moreover, the implantation technique suggested by the investigators should be prospectively validated. The eagerly awaited results from the SCOPE trial programme (NCT03011346 and NCT03192813) will further inform us on the comparative effectiveness regarding the PPI rate of this novel THV compared to other balloon-expandable (SAPIEN 3) and self-expanding (Evolut™ R; Medtronic, Minneapolis, MN, USA) devices.
Taken together, the implantation of new permanent pacemakers is an important complication after TAVI. The present study gives us new hope for low PPI rates in self-expanding THV. The PPI rate with the ACURATE neo THV is encouragingly low (being first in class of “next-generation“ devices). In the current examination by Toggweiler and colleagues, the perspective to reduce this PPI rate even further with a conservative predilatation strategy appears promising.
Conflict of interest statement
C. Hengstenberg serves as a proctor for Edwards and Symetis; he received travel grants and speaker’s honoraria from Edwards and Symetis. O. Husser receives proctor fees and travel grants from Symetis.