Drug-eluting stents (DES) revolutionised invasive cardiology at the beginning of this century by preventing restenosis through the controlled release of drugs which inhibit intimal proliferation of the smooth vasculature. The worldwide use of these stents in more than seven millions of patients has shown that the restenosis rate is not zero, but close to 10% and that there is no vascular healing with re-endothelialisation of the stent1,2. The lack of vascular healing is associated with late and very late (> 1 year) stent thrombosis3 with a mortality rate of up to 40%. Some randomised studies4 or registries5 have reported a higher mortality rate for DES than for the old bare metal stents. Thus, some experts warn against using drug-eluting stents and recommend going back to the old bare metal stents (BMS).
Should we go back to BMS?
Bare metal stents have some advantages and disadvantages. One of the advantages is that these devices show vascular healing after 4-6 months with re-endothelialisation at almost 100%1. Late and very late stent thrombosis are rare events, seen only in patients with delayed healing or allergies towards nickel and chromium. These stents are easy to produce and cheap, and are easy to implant with a small profile and good trackability. Major disadvantage of this type of stent is that it is associated with restenosis rates from 15-20% and require re-intervention in 5-10%5. However, dual antiplatelet therapy is needed only for 1-2 months. Nevertheless, bare metal stents are a valid alternative to drug eluting stents but are no longer considered as a “state of the art” device.
Should we use preferably DES?
Since the first reports of the adverse events of drug eluting stents due to
– lack of re-endothelialisation
– hypersensitivity reactions2 to polymer (carrier substance for the drug) and
– inappropriate stent apposition (ISA) probably due to cell-toxic effects of the drug on the smooth vasculature.
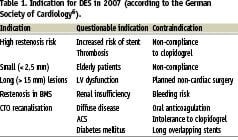
The most feared complication is late and very late stent thrombosis3 with a mortality rate of approximately 40%. Stent thrombosis occurs typically after stopping dual antiplatelet therapy with clopidogrel. A “jump-up” of major adverse cardiac events (MACE) was reported after stopping clopidogrel-treatment after 12 months. Thus, the indication list (Table 1) for drug eluting stents has shrunk to long lesions and small vessels as well as restenosis after bare metal stent implantation and chronic total occlusions6. All other indications can be covered by bare metal stents which show an equally good behaviour in large vessels, short lesions and patients with increased thrombotic risk etc (Table 1).
Should we use bio-active stents (BAS)?
New coating technologies allow improved tissue compatibility and reduce platelet aggregation and thrombin formation. One of the most bio-compatible materials is titanium which shows a very high corrosion resistance and tissue compatibility7. Vascular in-grow is faster for titanium than for stainless steel and re-endothelialisation is reached within weeks or months. The use of a bio-compatible alloy of titanium, namely titanium-nitride-oxide (TINOX) further improved tissue compatibility through the presence of NO-molecules on the surface of the titanium-coated stent8,9. Another bio-active stent is the endothelial progenitor cells capturing stent (EPC). This stent is believed to improve bio-compatibility, but first results showed a high restenosis potential with an angiographic late loss of up to 0,9 mm similar to bare metal stents.
New developments in the field of intracoronary stenting are aiming at a bioresorbable stent on the basis of a polilactic acid (PLA) or magnesium-alloy which are resolved within weeks or months and leave the vessel without foreign materials. However, several problems associated with these stents (inflammation, low radial force, high restenosis potential) need to be solved before these devices can be used in daily routine.
In summary, the recommendation to go back to bare metal stents cannot be supported due to the fact that these devices are not more “state of the art” and should be used only when there are
no other alternatives. Drug-eluting-stents represent a potential risk for the patient because they require long-term dual antiplatelet therapy with it’s inherent risk of bleeding and drug-drug interactions. A continuous risk of late and very late stent thrombosis associated with DES is due to the lack of vascular healing and delayed re-endothelialisation. Therefore, DES should be carefully used. In elderly patients, those with increased bleeding risk, patients requiring non-cardiac surgery, those with oral anticoagulation, intolerance to clopidogrel etc. New bio-active stents represent a true alternative to drug-eluting-stents or BMS and should be used more liberally.
The use of drug-eluting stents (DES) is the most effective way to reduce in-stent restenosis (ISR) according to randomised controlled trials in selected patient groups.1 However, there is no evidence that implantation of DES could influence mortality or prevent myocardial infarction (MI),2 and these devices may have some side effects as well. There has been growing concern that some patients develop stent thrombosis (ST), a life threatening complication, unusually late after the implantation of DES.1 Greater delay in arterial healing as manifested by poor endothelialisation and persistence peri-strut fibrin deposition may extend the risk of ST far beyond 30 days after DES implantation. Late ST (between one to 12 months) and very late ST (> 12 months) are potentially due to a mismatch between the stent and the vessel and may be related to stent malapposition, overlapping stent placement, penetration of necrotic core, excessive stent length, bifurcation lesions, hypersensitivity to drug or polymer, or thrombogenic surface.3,4 Premature antiplatelet therapy discontinuation has been the most important predisposing factor for late ST.5
The Academic Research Consortium (ARC) has developed a standardised definition of ST. According to ARC criteria, identical rates of ST has been observed in both selected DES and bare metal stent (BMS) patients up to four years according to recent pooled analyses of randomised DES trials.1,6 However, it is worth noticing, that a higher rate of late ST was observed in patients treated with BMS that was related to target lesion revascularisation (TLR), reaching it’s peak at 6 months. On the other hand, very late ST occurred more often in the DES patients that was not related to TLR. It would be highly interesting to see whether these late events of BMS are truly related to studied stents, or are they only closely associated with TLR-procedures with implantation of a second BMS or DES in observed restenotic lesions. In TAXUS and Cypher trials, 28% and 40% of definite or probable ST in the BMS group occurred after TLR, whereas ST was primary in 95% of TAXUS-patients and in 100% of Cypher-patients.6,7 Of note, it is important to notice that most of the randomised DES trials excluded so called “second ST” occurring subsequent to any TLR from the counts of episodes of ST. Recently presented data with the unrestricted use of first generation DES in routine clinical practice demonstrated that late ST occurred at a steady rate of 0.6% per year up to four years of follow-up.8
Pivotal DES trials have used thick strut BMS ensuring excellent DES results in reducing neointimal hyperplasia in fairly low-risk patients. The use of alternative materials (e.g. cobalt chromium) has enabled the production of thinner strut stents with higher radial strength. New strategies with BMS technologies have also been aimed at enhanced vascular healing. Titanium features superior biocompatibility when compared with stainless steel, gold, or other surface coatings. In vitro titanium-nitride-oxide showed diminished platelet adhesion and fibrinogen binding in comparison to stainless steel. Metallic sheaths coated with titanium-nitride or titanium-oxide exhibited higher cell density values on their surface compared to those without coating, supporting the view that deployment of stents with these coatings may achieve earlier complete endothelial coverage.9 The safety of a titanium-nitride-oxide-coated TITAN-2® “bio-active-stent” (BAS) has been confirmed by several clinical studies in both unselected populations, as well as in the most complex indications such as diabetics, small vessels and acute MI.10,11 The GENOUS® bio-engineered stent is coated with an antibody that captures circulating endothelial progenitor cells (EPC) for accelerated natural healing. The HEALING-FIM study showed that an EPC-capturing stent is safe and feasible for the treatment of de novo coronary artery disease.12 Recently, the use of EPC-capture stent during primary angioplasty has showed to be feasible and safe with no incidence of late ST and an acceptable rate of TLR.13 The safety and efficacy of GENOUS® stent will be determined within ongoing randomised trials (TRIAS LR and TRIAS HR).
The strategies aimed at reducing the risk of late ST should include optimised stent implantation and proper, long-enough antiplatelet therapy. Recent trial suggested a benefit of DES in terms of MACE in small vessels but the potential harm for large vessels (>3.0 mm).14 These results make sense, because neointimal hyperplasia is more important in smaller vessels less able to accommodate neointimal growth. Accordingly, BMS remains a valuable alternative to DES in large vessels. In addition, DES should be avoided in patients at increased risk of bleeding, those requiring long-term oral anticoagulation, and those scheduled for elective surgery. New generation bio-active stents with accelerated vascular healing could be a suitable option for these patients necessitating short term antiplatelet therapy. In addition, patients who are not able to take long-term antiplatelet therapy due to allergies to thienopyridines or poor compliance with extended antiplatelet therapy should not receive DES.
At this moment, should the heading of this article, “Why don’t we return to bare metal stents?” be favourably inclined? Due to our inability to accurately identify patients at risk for ST and the lack of effective therapies to mitigate the risk, advocates of BMS argue that the use of DES should be limited to small vessels and lesions with a higher probability of ISR. Since very late ST after DES placement has emerged as a major concern, and the new technologies for BMS that are now emerging, we could say that there is a place for these newer-generation bare metal “bioactive”-stents with proper vascular healing in present day interventional cardiology.
In all areas of medicine there are several treatment options. Usually the response to treatment differs between patients based on type and severity of the disease and on comorbidities. Different options also vary regarding risk of side effects and of cost. This is also the case with coronary artery disease in general and with stent selection in particular.
Drug eluting stents (DES) are designed to reduce neointimal hyperplasia and thereby restenosis. The superiority of DES over bare metal stents (BMS) is consistent in randomised trials and in registries with a relative risk reduction of target vessel revascularisation (TVR) of about 50-60%. However, the absolute reduction of restenosis and target vessel revascularisation is lower (3-4%) in registries1 compared to randomised trials or meta-analyses2 (10-14%) in which control angiography was mandated. There is also a large variation in relative and absolute benefits between different patients and lesions. Thus, in patients at high risk of restenosis such as diabetics treated with long stents with small diameters, 10 patients have to be treated with a DES in order to avoid one TVR3. On the contrary, in patients at low risk of restenosis, more than 160 patients have to be treated. Cost effectiveness, with the current price level of DES, has therefore been proven only in high risk patients4.
During the past several years there has remained an uncertainty over the long-term safety with DES as compared to BMS which is based on indications of worse late outcomes with DES than BMS in some randomised trials and long-term registries. However, after the last year’s accrual of additional results from several long-term registries and collaborative meta-analyses of all randomised trials, the overall long-term safety with DES seems comparable to bare metal stents (BMS) with similar rates of death or myocardial infarction up to four years. A major disadvantage with DES is, however, the remaining and continuous 0.5-0.6% per year risk of stent thrombosis5. This rare, but feared complication, with its high mortality seems to occur particularly after discontinuation of clopidogrel treatment6. Therefore, DES is associated with a need for prolonged dual antiplatelet therapy which is costly for the patient and, in addition, associated with risk of major bleeding that, at least at higher ages, might be larger than the risk of stent thrombosis itself. Today, the optimal dose and duration of thienopyridine treatment is unknown and the target of new, long-term prospective trials. A group prone to suffer from early and late stent thrombosis is the one out of four patients who respond poorly to clopidogrel7. Among patients with diabetes, poor responsiveness to clopidogrel is even more common, which further increases the risk of adverse events with DES8. Recent data from the TRITON trial indicates that the risk of stent thrombosis in the clopidogrel resistant and diabetic population can be overcome with prasugrel which however also will be needed over very long treatment periods with the inherent even larger consequences in added costs and probably higher risks of bleeding.
In patients with a high risk of restenosis these early benefits with DES therefore seem to compensate for the small increase in risk of stent thrombosis and major bleeding with long term thienopyridine treatment. However, in patients with a low risk of restenosis, the benefits concerning reintervention will be minimal and do not outweigh the risks of late stent thrombosis and risks and costs associated with long-term thienopyridine therapy. With the currently approved devices and drugs BMS should therefore be considered the first choice for stenting procedures. However, DES still has a place in the armamentarium, although reserved for patients at high risk of restenosis with presumed tolerance and adherence to long-term uninterrupted dual antiplatelet therapy. In patients with ST-elevation myocardial infarction, DES should generally be avoided, as this clinical evaluation is difficult and the risk of stent thrombosis increased.
So, why don’t we return to (only) BMS? And why don’t we return to (only) DES? Based on current knowledge and the available devices and drugs, both DES and BMS defend their use in different clinical settings based on risks of restenosis, bleeding and the public health economy. Currently, there is a fast development of new stent platforms, polymers and eluted drugs. Therefore, while recommending a restrictive use of the currently available DES, we eagerly await the new and safer alternatives without the long-term risks of complications and needs for long-term dual anti-platelet medication.
Percutaneous coronary angioplasty is an effective revascularisation treatment in patients with coronary artery disease. In the early days, it was limited by the occurrence of acute dissection and threatening vessel closure that required emergency cardiac surgery and a high incidence of recurrent narrowing of the vessel or restenosis. Restenosis after balloon angioplasty is a heterogeneous process caused by smaller, angiographically non-visible dissections, early and late recoil of the treated segment and intimal hyperplasia and tissue growth. When we started implanting metal stents in coronary arteries, initially the aim was for bail-out purposes in the setting of major dissection to prevent acute vessel closure. This proved to be an effective means to prevent urgent cardiac surgery. At first, acute stent thrombosis remained a major concern until we learned that dual antiplatelet therapy with aspirin and thienopyridines for four weeks could minimise this problem. Subsequently, the implantation of bare metal stents was shown to reduce restenosis compared to balloon angioplasty alone and the number and type of lesions and type of patients that we were able to treat percutaneously increased dramatically. With the development of in-stent-restenosis however, intimal hyperplasia with smooth-muscle-cell proliferation induced by injury to the vessel and a subsequent inflammatory reaction, turned out to be a rather difficult condition to treat. Moreover, stent implantation outside the setting of bail-out indications did not reduce the incidence of subsequent death or myocardial infarction. But stenting reduced the time of the procedure and increased the success rate, was technically easy with the availability of better, smaller and more flexible devices, expanded the indications for percutaneous procedures in a way that challenged the cardiac surgeons. Therefore, implantation of a bare metal stent during PCI was widely adopted as the preferred treatment. The occurrence of in-stent-restenosis in bare metal stents remained a problem, but the risk proved to be relatively predictable and dependent on reference vessel diameter, stent length, final lumen diameter after stent deployment, and conditions such as the presence of diabetes. With the availability of Cobalt-Chromium/thin-strut bare metal stents, clinical restenosis rates i.e. the need for repeat revascularisation because of recurrent ischaemia and anginal symptoms were below 10% in non-diabetic patients with large vessels and relatively short stents. In patients with non-focal or diffuse in-stent-restenosis, repeat balloon angioplasty, debulking, stent-in-stent were all disappointing with recurrent in-stent-re-restenosis of 30%-50%. Only intravascular brachytherapy seemed to be effective but this was not widely adopted. Thus, the use of drug-eluting stents for the treatment of in-stent-restenosis and for patients with complex multivessel disease that would otherwise have been sent to the cardiac surgeon seemed the logical next step. The rapid worldwide acceptance of drug-eluting stents for all indications and patients has surprised and puzzled many clinicians. Particularly, as drug-eluting stents compared to bare metal stents do not reduce the incidence of death or myocardial infarction, any signal of a late safety concern with late and very late stent thrombosis is worrisome. Recent meta-analyses1 and reports of large registries2 did not show an increase in the incidence of death or myocardial infarction associated with the use of drug-eluting stents compared to bare metal stents. However, the combined experience of the investigators from Bern and Rotterdam3 showed an incidence of stent thrombosis of 0.6% per year up to four years after implantation with no sign of a reduction in risk in later years. In addition, the problem of the long term treatment with dual antiplatelet therapy after drug-eluting stent implantation with its less than optimal effectiveness or its associated increased bleeding risk (dual antiplatelet: How high? How long? aspirin/clopidogrel resistance?) has not been solved.
Therefore, I would advocate the use of bare metal stents in lesions/patients with low risk of restenosis and “restricted” use of drug-eluting stents in lesions with high risk of restenosis such as long lesions, small vessels, chronic total occlusions and patients with diabetes. Patients with in-stent-restenosis after bare metal stent can be treated with drug-eluting stents which have been shown to be effective and safe for this indication. Finally, we need better technologies, even if this requires large expensive trials with long term follow-up.

