Recently, one of our contributing authors sent us a polite and friendly message. In his letter to the Editor in Chief, he mentioned that one of his manuscripts entitled “First double implantation of an aortic and mitral valve” had been rejected nine months previously by EuroIntervention and he was somewhat surprised therefore, not to mention upset, to discover that we were now publishing a similar first-in-man experience, when his own had been rejected.
We had to confess that one of our senior members had turned down this paper on his own without reporting it to the editorial board. This was undoubtedly an unforgivable oversight on our part, so we gave the author the possibility of reporting on his own first-in-man, with the benefit of including the nine-month follow-up results of his patient.
These two first-in-man procedures differed substantially. The originality of the first –the one which initially failed to be published– was that the operator first implanted the mitral valve and then the aortic valve, with less risk of modifying the geometry of the mitral valve1. The patient survived, but suffered a late complication caused by the migration of the aortic prosthesis into the outflow tract. The patient thus became a surgical candidate –an interesting paradox– and eventually died due to new oncological problems.
The other procedure, which had been published previously (prior to this one), involved a similar case; however, the implantation of the mitral valve was performed following the aortic valve implantation. In this case, the mitral valve affected the outflow tract substantially and, as a consequence, the patient developed an outflow tract gradient and died within 24 hours2.
These two “first-in-man” case histories prompt me to reflect on the very nature of first-in-man intervention and to try to capture the difference between an experienced operator performing what we call a “first in man” and a genuine pioneer.
If we look at the history of percutaneous interventional cardiology, the indisputable and universally recognised pioneer was Andreas Gruentzig. Still, it is interesting to remind our readers that Richard Myler, who is now largely forgotten by young interventional cardiologists, performed the first balloon angioplasty in the left anterior descending artery. Richard Myler was assisted by Andreas Gruentzig, and the device was inserted into the narrowed vessel through an arteriotomy performed by a surgeon on a patient under cardiopulmonary bypass.
It is also interesting to remember that Andreas Gruentzig had a hard time convincing his fellow cardiologists that his approach was feasible. Without the support of another pioneer, the surgeon Ake Senning, who performed the first implantation of a pacemaker in a human (he was also the father of the Senning operation), it would have been impossible for him to perform the first balloon angioplasty. In fact, this first patient was a patient of Professor Ake Senning, and it was Andreas Gruentzig and Senning who took full responsibility for treating the first case in September 1977.
Looking at the history of this case, it is interesting to read now what the patient himself said about the whole procedure. He kept telling us that he had complete trust in Andreas Gruentzig because of the honesty with which Andreas had, in advance, described the procedure, clearly explaining the entire process, not failing to emphasise the unknowns of the procedure, all of which helped to gain the full confidence of the patient. The trust of this first patient played a critical role in making Andreas Gruentzig the father of interventional cardiology.
Almost a decade later, the first stenting was performed by several other pioneers. Jacques Puel in Toulouse, preceding by a few weeks the procedure of Ulrich Sigwart from Lausanne where the Medinvent company was located. For the sake of history, it was in December of 1985, one year before the implantation, that Charles Imbert, a brilliant engineer, managed to miniaturise the WALLSTENT –the invention of the Swedish engineer Hans Wallsten– which was a double helix scaffolding endoprosthesis created for the acute treatment of aortic dissection – originally a request of Professor Ake Senning himself.
On the other side of the Atlantic, inventors such as Julio Palmaz, a radiologist, and Richard Schatz, a cardiologist, together developed the Palmaz-Schatz stent. Turning to South America, they worked with Eduardo Sousa who was the first to test this balloon-expandable stent in one of his patients in the presence of Julio Palmaz and Richard Schatz. It was Richard Schatz who had the idea of creating a link between the two compartments of the device, which would otherwise have been very rigid and non-flexible.
Conversely, the implantation of drug-eluting stents was, in many ways, a first-in-man intervention in Sao Paulo and Rotterdam, but we must say, with all due modesty, that this entailed nothing radically different from the implantation of earlier types of cardiovascular stents in terms of acute treatment. In short, there was little in the way of surprises to be expected from this new generation of stents simply because they possessed a cytostatic medium on their surface.
Similarly, one of the next first-in-man coronary procedures took place in New Zealand with the implantation of the first bioresorbable scaffold by John Ormiston shortly before the first case was performed in Rotterdam. The concept of bioresorbable scaffolds dated back to 1988 when Richard Stack at Duke in North Carolina, USA, had the idea of creating a stent in polylactide. Here again, by the time we implanted this new scaffold, the physicians were “just” the operators.
The story is radically different when we look at the field of valvular heart disease. Among today’s pioneers are Kahn et al who performed the first pulmonary balloon valvuloplasty in 1982. In the field of aortic valve replacement we have another indisputable pioneer with the same stature as Andreas Gruentzig, namely Alain Cribier, who was initially traumatised by the only transient benefit of the balloon valvuloplasty and obsessed by the challenge to make the result permanent. Alain Cribier also assumed full responsibility of the world’s first very spectacular valve replacement in a compassionate case.
Of course, I haven’t even begun to mention many of the other true pioneers in the fields of neurological treatments, stroke, left appendage occlusion, mitral balloon valvuloplasty and triple A, etc. By now I hope you have started to understand what I am outlining and are beginning to discern the differences between a true pioneer, an inventor, and just a very experienced physician operating on a patient with a new device for the first time worldwide. I would like to emphasise the difference between a new concept and a first application, between an idea that will change the face of medicine and the single individual who will use a device or procedure for the first time.
Looking back over the last 40 years we have seen several extraordinary individuals who were inspired by their passion to improve the non-invasiveness of treatments which before were exclusively surgical. First-in-man experiences, although accomplished by excellent operators, only apply or try to apply a variant of the great work already carried out by genuine pioneers.
As we enter this New Year, and look resolutely towards a better future, it is good to remember the lessons learned from the true pioneers in our speciality. True pioneering status can only be assigned when an individual has introduced –conceptually– a new way of practising medicine. While a first-in-man is certainly “pushing the limits” of interventional cardiology, we must never forget that these limits only exist –and our practice infinitely improved– because they were previously imagined, created and brought to the test by the true pioneers.
Postscript
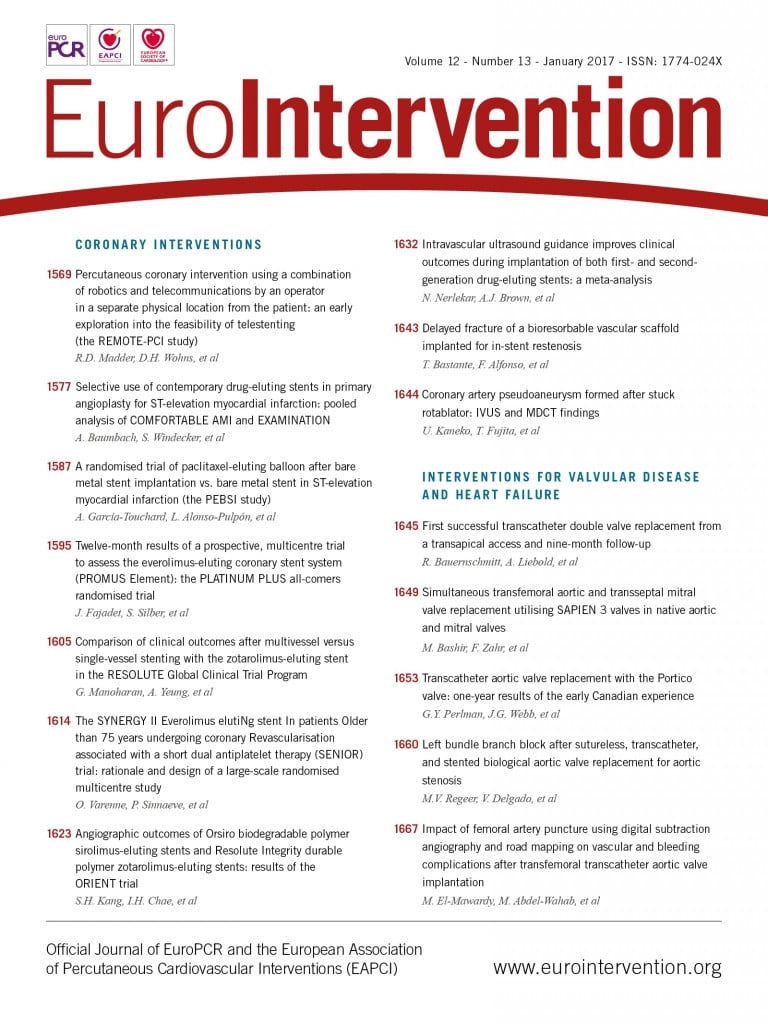
As we go to press we just received a third manuscript along the same lines as the others we mentioned earlier in our editorial. This one is on a simultaneous transfemoral aortic and transseptal mitral valve replacement3. The work of our pioneers has paved the way for the increase in our clinical expertise, now the expert operators are sharing their experience and we found it important to include this “breaking” third case study for you in this issue so you can see for yourselves.