Abstract
Aim: The purpose of this study was to evaluate the impact of time-to-reperfusion on outcome after facilitated percutaneous coronary intervention (PCI) i.e. PCI following early pharmacological reperfusion therapy in ST-segment elevation myocardial infarction (STEMI).
Methods and results: The study population consisted of 262 consecutive patients with STEMI, aged <75 years, without cardiogenic shock, presenting <12 hours of chest pain onset, transferred from community hospitals to a catheterization laboratory with time delay >90 min after pharmacological reperfusion therapy (alteplase i.v. bolus 15 mg followed by an infusion – 35 mg/60 min; abciximab i.v. bolus 0.25 mg/kg followed by a 12-hour infusion – 0.125 µg/kg/min; unfractionated heparin i.v. bolus 40 U/kg [maximum 3000 U]). One hundred seventeen patients (44.7%) received pharmacological reperfusion therapy <3 h after chest pain onset, 101 (38.5%) at 3-6 h and 44 patients (16.8%) >6 h. Patent infarct-related artery rates at initial angiography were similar among the study groups. PCI significantly improved epicardial flow in all three groups. Mortality at 12 months was significantly related to time-to-pharmacological reperfusion (3.4% [<3 h], 4.0% [3-6 h], 13.6% [>6 h], p = 0.027). At 6 months left ventricular ejection fraction was significantly improved in the two groups of patients with time-to-pharmacological reperfusion <6 hours and the time-to-pharmacological reperfusion was the independent predictor of lack of left ventricular ejection fraction recovery.
Conclusion: Our study shows that among STEMI patients undergoing facilitated PCI, time-to-pharmacological reperfusion significantly affects left ventricular function recovery and long-term mortality.
Introduction
Initiation of fibrinolytic therapy within 6-12 hours after the onset of chest pain significantly reduces mortality in patients with ST-segment elevation myocardial infarction (STEMI)1,2. However, the ability of fibrinolytic treatment to open the occlusion responsible for STEMI declines with the increasing interval between symptom onset and the initiation of the therapy3. Primary percutaneous coronary intervention (PCI) for STEMI is free from this limitation and is associated with the highest efficacy in establishing the infarct-related artery patency4. Trials comparing routine fibrinolysis with PCI for STEMI have shown reduced 30-day mortality among patients undergoing primary PCI2,5,6. However, the need for a long-distance transport to a hospital offering 24/7 service by experienced operators, limits access to invasive treatment for myocardial infarction, as it may markedly delay initiation of reperfusion therapy from the onset of STEMI2. In fact, the increasing time from symptom onset to presentation directly and similarly affects survival in patients with STEMI receiving fibrinolytic therapy and undergoing primary PCI, particularly in high-risk patients4,7-11. Early pharmacological therapy may promote reperfusion and improve outcome by preservation of left ventricular function12. This may certainly overcome the delay due to long-distance transportation.
We have previously suggested that pharmacological facilitation can be successfully employed to allow prolonged (>90 min) transfer from a community hospital without interventional facility to the primary PCI centre13. The purpose of the present study is to evaluate the effect of time-to-pharmacological reperfusion on clinical outcome after facilitated PCI for STEMI following prolonged transfer.
Methods
Study population
The study population is represented by a consecutive series of 262 STEMI patients included in the Krakow Programme of Interventional Treatment for Myocardial Infarction between June 2001 and March 2002 and referred to the Department of Interventional Cardiology of the Institute of Cardiology, Medical College Jagiellonian University in Krakow from community hospitals with transportation time >90 min. Detailed inclusion and exclusion criteria have been provided elsewhere13. In brief, patients presenting within 12 hours after chest pain onset, with ST-segment elevation >0.1 mV in at least two adjacent leads or acute left bundle branch block, aged <75 years, without cardiogenic shock and contraindications to fibrinolysis entered the study.
Treatment
After exclusion of contraindications and phone contact with the primary PCI facility, patients received pharmacological reperfusion therapy in a community hospital. They were given aspirin (100-325 mg), intravenous bolus of unfractioned heparin (40 U/kg, maximum 3000 U), 15 mg alteplase and 0.25 mg/kg abciximab, and then intravenous infusion of alteplase (35 mg/60 min) and abciximab (0.125 ug/kg/min over 12 hours). Upon initiation of the treatment patients were transported by an ambulance or by air to the primary PCI centre at the Institute of Cardiology in Krakow. Patients received 300 mg of clopidogrel on admission to the interventional facility. Coronary angiography and angioplasty were performed as previously described13. A decision about bare metal stent implantation was made by the operator in case of suboptimal balloon angioplasty (diameter stenosis >30%), dissection impairing blood flow and/or possible reocclusion, and stenosis of proximal left anterior descending artery. Procedural success was defined as restored Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow and diameter stenosis <30% at the site of occlusion for balloon angioplasty and <20% for stent implantation. In some patients with TIMI grade 3 flow at initial angiography and clinical signs of myocardial reperfusion PCI was postponed or coronary artery bypass grafting was performed. Adjunctive pharmacological therapy was used in compliance with current guidelines for STEMI management.
Angiographic assessment
TIMI grade flow in the infarct-related artery and TIMI myocardial perfusion grade (TMPG) were assessed at baseline and after PCI, in compliance with the currently accepted criteria14,15. Analysis was performed in angiographic core laboratory at Krakow Cardiovascular Research Institute (Krakow, Poland) by an independent observer with New Quant32, QCAPlus software (Sanders Data Systems, Palo Alto, CA, USA).
Clinical assessment
The primary end point was mortality at 12-month follow-up. Re-infarction was defined as recurrent chest pain with new changes in the ECG (ST-segment elevation, left bundle branch block, new Q waves) and/or 2-fold elevation in creatine kinase over the normal upper limit or by a further 50% increase if already over the normal upper limit. Left ventricular ejection fraction was assessed by echocardiography (SONOS 5500 Agilent Technologies Inc., Palo Alto, CA, USA) according to Simpson in classical two- and four-chamber apical projections within 2 to 3 days after admission (baseline) and at 6 months.
Statistical analysis
Categorical data were presented as counts and proportions (percentages) and continuous variables were expressed as means ± standard deviations. Statistical comparisons between subgroups were performed using chi-square test and Fisher’s exact test for categorical variables, and paired Student’s t-test and the Kruskal-Wallis test for continuous variables, as appropriate. Cumulative risk of death was estimated using Kaplan-Meier curves and differences between the study groups were evaluated with the log-rank test. In addition, the multivariate Cox regression analysis was performed to find significant predictors of survival. Multiple linear regression was performed to identify independent predictors of left ventricular ejection fraction recovery at 6 months. A p value of < 0.05 was considered statistically significant.
Results
Our population is represented by 262 patients who underwent facilitated primary angioplasty. In 117 patients (44.7%) pharmacological reperfusion therapy was administered <3 hours after chest pain onset, 101 (38.5%) 3-6 hours, and 44 patients (16.8%) >6 hours. Table 1 summarizes clinical characteristics of the study population according to time from chest pain onset to pharmacological reperfusion.
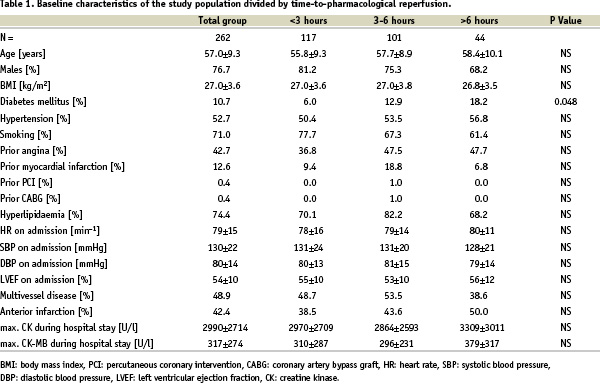
Diabetes mellitus was more frequent in patients with time-to-reperfusion >6 hours. Left ventricular ejection fraction on admission was similar among the study groups. Mean time from pharmacological reperfusion therapy to femoral artery puncture was 132±40 min and was similar among the study groups (132±43 min (<3 hours), 134±39 min (3-6 hours), 131±33 min (>6 hours), p=NS).
Time-to-reperfusion, angiographic and clinical outcomes
Frequency of TIMI grade 2 to 3 flow at initial angiography was similar among the study groups (89.8% (<3 hours), 80.5% (3-6 hours), 86.1% (>6 hours), p=NS) - see Figure 1.
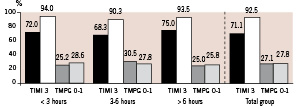
Figure 1. Angiographic results for time intervals from chest pain onset to pharmacological reperfusion therapy. (black bars - The Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow before percutaneous coronary intervention (PCI), white bars - TIMI grade 3 flow after PCI, dark grey bars - TIMI myocardial perfusion grade (TMPG) grade 0 to 1 flow before PCI, light grey bars - TMPG grade 0 to 1 flow post PCI). p<0.001 for all comparisons between TIMI grade 3 flow before and after PCI groups, p=NS for all comparisons between TMPG grade 0 to 1 flow before and after PCI groups.
PCI after early pharmacological reperfusion therapy was highly effective and angiographic results were similar among the study groups. The distribution of TMPG before and after PCI did not differ significantly among the groups, either.
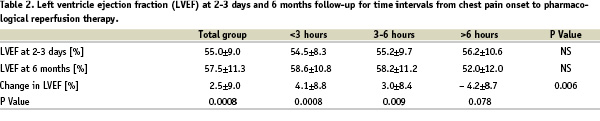
Despite no difference at baseline, left ventricular ejection fraction (Table 2) significantly improved at follow-up (6 months) only in patients with time-to-pharmacological reperfusion therapy <6 hours.
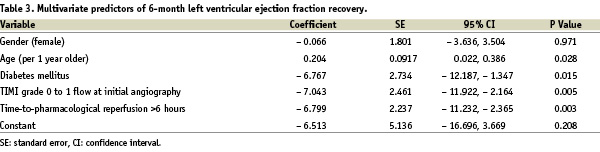
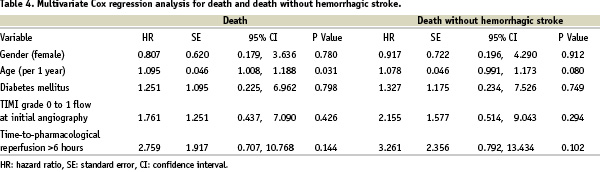
In the multivariate analysis, time from chest pain onset to pharmacological reperfusion, occluded infarct-related artery (TIMI grade 0 to 1 flow) at initial angiography and diabetes mellitus were the independent predictors of lack of left ventricular ejection fraction recovery at 6 months (Table 3).
As clearly reported in Figure 2 at 12-month follow-up mortality was also highest with the longest time to reperfusion.
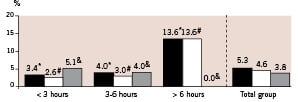
Figure 2. Clinical results at 12 months for time intervals from chest pain onset to pharmacological reperfusion therapy. (black bars – death, white bars – death without hemorrhagic stroke, grey bars – non-fatal re-infarction). * – p = 0.027, # – p = 0.007, & – p = NS.
The difference was already observed within 30 days and was stable till 12-month follow-up (Figure 3), but in the multivariate Cox regression analysis age was the only independent predictor of 12-month mortality (Table 4).
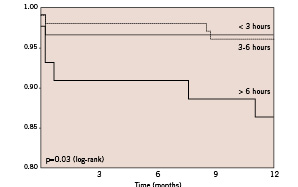
Figure 3. Kaplan-Maier survival curves for time intervals from chest pain onset to pharmacological reperfusion therapy.
Discussion
Recent data indicate that even long-distance transportation for primary PCI improves outcomes in comparison to fibrinolysis at hospitals without invasive treatment facility16-19. However, the mortality benefit associated with primary PCI in STEMI is sustained if time-to-reperfusion is <60 min20. According to the European and American guidelines, primary PCI is a method of choice in patients with expected delay to invasive treatment <90 min from a patient’s first medical contact21-23.
In patients with STEMI and expected transport >90 min routine fibrinolysis remains the treatment of choice. A good alternative could be facilitated PCI, i.e. out-of hospital pharmacological reperfusion therapy followed by PCI for STEMI24. This treatment option may shorten duration of myocardial ischaemia which is the main determinant of infarct size in experimental models25-27. Confirming these experimental studies, patency of the infarct-related artery before PCI has been shown to be associated with improved clinical outcomes and better preservation of left ventricular function at long-term follow-up28-30.
We have previously suggested that pharmacological facilitation of primary PCI, achieved with combination thrombolytic therapy (abciximab, unfractionated heparin and half-dose alteplase) can be successfully employed to allow long-distance transportation (>90 min) from community hospital without interventional cardiology facilities to the primary PCI centre. This strategy appears to confer a very high initial patency of the infarct-related artery upon arrival to the interventional facility and clinical outcomes equivalent to those seen in patients directly transferred for primary PCI13. In the present study, we demonstrated that the acute efficacy of such pharmacoinvasive approach is independent from the time to achieve reperfusion. This finding is in accordance with data on primary PCI and in contrast to standard fibrinolytic therapy for STEMI which efficacy diminishes with the increasing time from chest pain onset to reperfusion3. In the current study the efficacy of epicardial reperfusion and microcirculation as assessed by angiographic parameters was comparable in the study groups, and PCI after fibrinolytic therapy was safe and resulted in additional improvement of epicardial perfusion.
On the other hand, our data show that the time-to-pharmacological reperfusion does matter for long-term outcomes of STEMI patients treated with facilitated angioplasty. Similarly to primary PCI without facilitation and conventional thrombolysis, we noted increased mortality with prolonged time from chest pain onset to reperfusion4,7-11. In fact, in our study we demonstrated that despite similar rates in terms of preprocedural epicardial and myocardial perfusion, the immediate and late mortality was the highest in patients receiving pharmacological treatment >6 hours. Furthermore, the improvement in left ventricular ejection fraction at 6-month follow-up was only observed in patients with earlier pharmacological reperfusion (<6 hours). These data further confirm previous observation that optimal epicardial and myocardial reperfusion can not abrogate the deleterious effect of longer time-delay to treatment31,32. Our data are consistent with those by Brodie et al. who demonstrated that the short time-to-reperfusion was associated with improved left ventricular function at long-term follow-up4.
Conclusions
Our study shows that in patients with STEMI undergoing pharmacological facilitation during transportation, transfer to primary PCI centre, even in excess of 90 min can produce favourable short- and long-term outcomes as long as time from chest pain onset to initial fibrinolysis does not exceed 6 hours. In fact, patients with time-delay to reperfusion >6 hours, despite similar rates in terms of preprocedural epicardial and myocardial reperfusion, had no improvement in left ventricular ejection fraction and higher mortality in comparison with patients treated within 6 hours from symptoms onset. Future larger trials are certainly needed in order to confirm this finding.
Acknowledgments
The authors thank Dr Giuseppe De Luca for his invaluable comments. The study did not receive financial support from pharmaceutical industry or other commercial sources. It was financed entirely by the National Health Care Agency of Poland, Krakow Regional Division, as a part of the program to improve early detection and treatment of myocardial infarction in that region of Poland.

