Abstract
Background: Primary PCI (p-PCI) was shown to be the most effective reperfusion strategy for ST segment elevation myocardial infarction (STEMI). However, its success rates and clinical outcomes among the elderly patients are less well defined. The aim of this work was to access, whether primary PCI, as compared to thrombolysis, improves the outcomes of elderly patients with STEMI to the same extent as in the younger patient groups and whether this holds true also for the elderly patients presenting in cardiogenic shock or acute heart failure.
Patients: A total of 2,073 patients were analysed: 1,050 were enrolled in the randomised trials PRAGUE-1 and -2 and 1,023 entered a p-PCI registry at our institution. The mean age was 64 years, 29% were females. Three hundred and ninety patients were in the elderly (> 75 years) age group, 605 patients were aged 65-74 years and 1,078 patients were <65 years old. Acute heart failure was more prevalent in the patients that entered in the registry as compared to the randomised patients: Killip class IV 10% vs 1% (p < 0.001), Killip II-III class 29% vs 18% (p < 0.001).
Results: An optimal PCI result was achieved in 81% of the elderly and 90% of the younger patients (p < 0.001). The absolute mortality reduction by p-PCI compared to thrombolysis was 5.7% in the elderly and 3.7% in the younger groups (n.s.). The in-hospital mortality of Killip IV patients was 69% (elderly group), 54% (group 65-74 years, p < 0.001) and 27% (group <65 years, p < 0.001). The in-hospital mortality of patients without cardiogenic shock was low in all age groups: 4% (elderly), 2.7% (65-74 years) and 0.8% (<65 years).
Conclusion: Primary PCI is the most effective reperfusion strategy for the elderly patients presenting with STEMI.
The periprocedural mortality risk of the elderly patients undergoing elective percutaneous coronary intervention (PCI) was reported to be two- to fourfold higher than those of younger patients due to the presence of co-morbidities which include peripheral vascular disease and a more extensive coronary disease1. This difference may even be more pronounced in the setting of STEMI2,3. Elderly patients in cardiogenic shock may not benefit from revascularisation to the same extent as their younger counterparts4.
On the other hand, thrombolysis itself was shown to be associated with a survival disadvantage in patients > 75 years (hazard ratio 1.38, 95% CI 1.12 to 1.71, p=0.003) and is thus not considered
a valid reperfusion strategy for this patient group either5. Despite other6 reported mortality benefit of lytics over placebo (26% versus 29.4%, p=0.03) in patients > 75 years of age presenting with
a STEMI, the cardiology community remains reluctant to use lytics for these elderly patients. This scepticism was expressed by D.R. Thiemann saying that, “Thrombolysis in the elderly seems to offer more harm than good.”5
Our work was aimed at assessing whether primary PCI, as compared to thrombolysis, improves the outcome of elderly patients presenting with STEMI and whether this holds true also for the subgroup of elderly patients presenting with heart failure or cardiogenic shock.
Methods
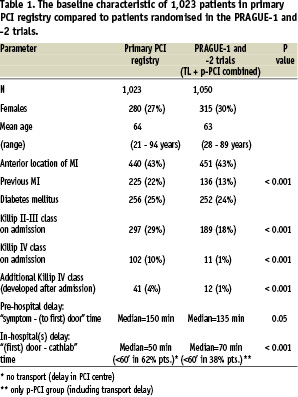
In this work we assessed data from 2,073 patients enrolled in the PRAGUE study program or entered in a single centre primary PCI registry. All patients were treated for a STEMI within 12 hours of symptom onset. Their baseline characteristics are listed in Table 1.
The PRAGUE-1 and -2 trials compared immediate thrombolysis in the nearest community hospital (without catheterisation facilities) versus inter-hospital transportation to a tertiary PCI centre for primary PCI. Both trials enrolled elderly patients as well (> 75 years of age). In parallel, a single centre primary PCI registry was started in the coordinating centre (Cardiocenter, Charles University Prague – University Hospital Vinohrady). The entry criteria to the registry and to the trials was similar (ST elevation myocardial infarction within 12 hours from symptom onset) with only one important exception; patients who had a contraindication for thrombolysis could not be randomised into the PRAGUE trials, but obviously they have been enrolled in the primary PCI registry. For more details see below.
Data from the primary PCI registry and the PRAGUE trials were merged in order to increase the amount of analysable patients with acute heart failure (Killip classes II - IV). A retrospective analysis was performed with a focus on age, Killip class and final clinical outcome (death from any cause during hospital stay up to day 30).
The PRAGUE trials data has been described in detail elsewhere.7,8 The PRAGUE-1 trial7 enrolled 300 patients with ST elevation myocardial infarction who presented to a community hospital without a cathlab in 1997-9. They were randomised into three groups: thrombolysis in this community hospital (TL, n=99), thrombolysis during transportation to a PCI centre (facilitated angioplasty, f-PCI, n=100) and transported to primary angioplasty without lytics (p-PCI, n=101). The f-PCI arm is excluded from this analysis because it was not part of the PRAGUE-2 trial. The PRAGUE-2 trial8 enrolled 850 patients who presented within 12 hours of symptom onset to a community hospital without a cathlab in 2000 - 2002. They were then randomised into two groups: thrombolysis in this community hospital (TL, n=421) or transported to primary angioplasty without lytics (p-PCI, n=429). Thus, for the purpose of this paper, 1,050 patients are analysed on an “intention-to treat” principle: 530 in p-PCI group and 520 in the TL group.
Registry data
During a 3 year period (2000-2002) a total of 1,023 patients were treated by primary PCI at the Cardiocenter, University Hospital Vinohrady, Prague, Czech Republic. Fifty-five patients randomised to primary PCI at the Cardiocenter Vinohrady during the PRAGUE-2 trial did not appear in the registry.
The baseline characteristics of the patients entered in the registry, as compared to the patients analysed from the PRAGUE studies, are listed in Tables 1-2. The mean age, proportion of females, diabetics and anterior infarctions was almost the same as in the PRAGUE trials. Patients in the registry had more frequent acute heart failure and shock, had more frequently previous infarction and longer pre-hospital delays.
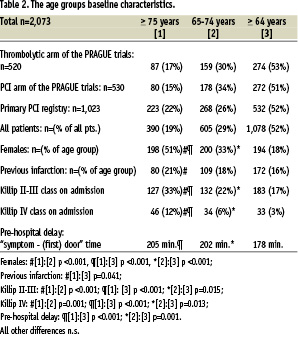
There were 390 (19%) elderly (> 75 years) patients among all 2,073 analysed. The age group 65-74 years comprised 605 patients (29%). The remaining 1,078 patients (52%) were younger than 65 years (Table 2). The elderly patients were more frequently females, and more frequently presented with heart failure or cardiogenic shock. The patients < 65 years presented to the hospital almost half an hour earlier then patients > 65 years.
All patients undergoing primary PCI, both in the registry and in the two trials, received aspirin (usually intravenous Aspegic 0.5 g) and bolus Heparin (5,000-10,000 units) in the pre-hospital phase. The PCI procedure included stent implantation in 78% of the patients. GPIIb/IIIa blockers were used in 4% of the primary PCI cases. Ticlopidine or clopidogrel was given daily from the first day and continued for at least one month to all patients with a stent in the registry, as well as to all patients (including the thrombolytic arm) in the trials. No drug eluting stents were used. Other medication (including additional heparin during PCI procedure) was left on the discretion of the physicians.
Outcomes assessment
The clinical end-point (death of any cause) was assessed at hospital discharge or on day 30, whatever came first. Cardiogenic shock was defined as systolic blood pressure < 90 mmHg with tachycardia (heart rate > 90 per minute) and with clinical signs of systemic hypoperfusion. PCI results were assessed by the interventional cardiologist performing the procedure at the procedure end. A fully successful PCI procedure was defined as TIMI-3 flow and residual stenosis < 20%. A partly successful procedure was defined either as the improvement of TIMI flow from 0-1 before PCI to TIMI-2 after PCI or as combination of TIMI-3 flow after PCI with residual stenosis >20%. Unsuccessful PCI was defined as any other finding. These definitions were used for both datasets (trials and registry). Due to the fact, that in-hospital outcomes were assessed, there were no missing data regarding the key factors: vital status, Killip class on admission and age.
Statistical evaluation
The chi-square, Fischer´s exact test, Student t-test and Wilcoxon two-tailed test were used for the analysis of these data.
Results
The mortality among trial patients as compared to the registry patients is described in Table 3. Despite the trend to higher mortality in the registry, neither difference is significant.
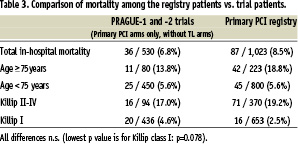
The prevalence of cardiogenic shock and pulmonary oedema is shown in Table 1. The prevalence of cardiogenic shock at the time of initial presentation is 10 fold higher in the registry (10%) as compared to the randomised trials (1%), p < 0.001. Also prevalence of milder forms of acute heart failure (Killip II-III) is significantly higher in the registry (29%) than in the randomised trials (18%), p < 0.001. Cardiogenic shock is 4 times more frequent among the elderly patients as compared to patients below 65 years (p < 0.001, OR 4.2). A total of 44.4% (173 from 390) elderly (> 75 years) patients initially presented with some degree of acute heart failure, while in younger age groups impaired Killip class at the time of initial presentation was in 20% (216 from 1078 patients, p < 0.001, OR=3.3) and 27.4% (166 from 605 patients, p=0.001, OR=2.1).
Angioplasty (with or without stenting) was not performed in 265 (12.8%) of the patients included in this dataset. This was because either: (1) TIMI-3 flow was present, chest pain absent, ST elevations resolved at the time of angiography with anatomy being more optimal for bypass surgery than for PCI (n=158), or (2) chronic total occlusion (old infarction or left ventricular aneurysm falsely diagnosed as acute infarction) (n=14), or (3) absence of significant coronary stenosis - usually wrong diagnosed, the true diagnosis being acute pericarditis, pulmonary embolism or no cardiac disease (n=34), or (4) coronary anatomy totally unsuitable neither for PCI or for CABG due to extremely advanced severe diffuse calcific narrowing of the coronary arteries (n=59). Interestingly, among the elderly group this was the case in 19%, while in patients < 75 years only in 11% (p=0.022, OR=1.5). Fully successful PCI procedures were at 81% in the elderly group vs. 85% in the “65-74” group (NS, OR 0.75) vs. 90% in the younger group (p < 0.001, OR = 0.47). Finally, partly successful procedure was at 88%, 90% and 94% (NS, OR=1.2, resp. p=0.001, OR=2.1) with decreasing age in groups (Figure 1).
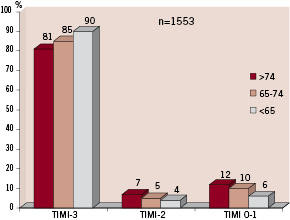
Figure 1. The results of primary PCI in age groups. TIMI-3 means in all patients including residual stenosis <20%. TIMI-2 means TIMI-2 flow with or without any residual stenosis. TIMI 0-1 means unsuccessful PCI procedure (even if stent was successfully deployed, but no significant distal flow occurred).
Figure 2 shows the influence of age and Killip class on the likelihood of in-hospital death among the registry patients. A person over 75 years presenting in cardiogenic shock has 69% risk of death despite the most effective, technically successful and timely use of reperfusion therapy. On the other hand, a person below 65 years of age, who is not yet in shock upon arrival in the hospital, has a in-hospital mortality risk of close to 0%, when treated by primary PCI. This percentage becomes 4% in the elderly patients.
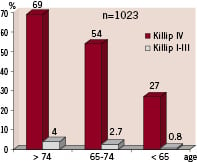
Figure 2. In-hospital mortality [%] after primary PCI related to age and Killip class. Primary PCI registry.
Transferring for p-PCI was beneficial in all patient age groups (this applies to the Prague trials data set only). Figure 3 shows impact of age and acute heart failure on the outcomes of patients treated by the two reperfusion strategies used in the trials. Figure 4 shows that the relative benefit from p-PCI is decreased in the elderly, however, the absolute benefit was the same across all age groups (4-6% lives were saved without influence of age on this number).
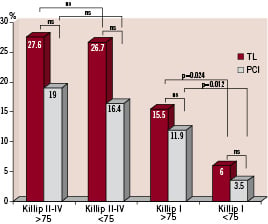
Figure 3. Thirty-day mortality related to age and Killip class in the PRAGUE 1 and 2 trials. Because only a few patients with cardiogenic shock have been randomised to the PRAGUE trials, Killip II-IV classes are shown together in this graph. Benefit from PCI is reduced among elderly patients presenting in heart failure. TL=thrombolysis.
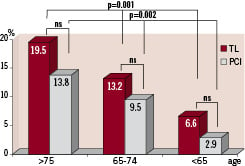
Figure 4. Thirty-day mortality in the PRAGUE trials as related to age. The relative benefit from PCI is decreased in the elderly, however, the absolute benefit is the same across all age groups (4-6% lives saved without influence of age on this number). TL=thrombolysis.
Discussion
The registry patients in this study had more frequent acute heart failure and shock, more previous infarctions and longer pre-hospital delays when compared to the randomised trials patients. The possible explanations may be multiple, but most likely it is a practical one: when a patients arrives at a hospital in a critical state, the healthcare professionals rush to help this patient as quickly as possible, and less frequently take the time to enrol such a patient in any randomised trial. Acute heart failure or shock complicating acute myocardial infarction is more frequent among patients with previous infarctions and also among those presenting late and thus further emphasizes this “real-life patient preselection”.
Randomised trials in general show more favourable outcomes when compared to registries9-16. Similar trends (albeit not significant) were found in this analysis. The prevalence of cardiogenic shock largely differs between randomised trials11,12 and real life registries13-16 of ST elevation acute myocardial infarction. The PRAGUE trials did not exclude patients with shock per this protocol, however only very few (1%) of the patients randomised were in cardiogenic shock on initial presentation. An additional 1% developed shock later in the course of their infarction. Despite our findings of only non-significant mortality difference between registry and trial patients, the trend is similar to previously published data.9-16 Possible explanations can be found in the very few exclusion criteria in the PRAGUE trials 7,8 as opposed to others.11,12
PCI was performed less frequently (81%) in the elderly group as compared to 89% PCI rate among patients < 75 years. Similar results (including much worse outcomes of patients over 75 years of age) were found in a recently published German registry.15 Elderly patients have substantially more co-morbidities including: previous infarction, renal failure, diabetes, and hypertension. Furthermore, there were more females among the elderly, and females are known to have frequently narrow and tortuous coronary arteries, less suitable for PCI.
Primary PCI in the elderly population may be technically challenging due to a more extensive coronary and peripheral atherosclerosis15 and a frequent lack of patient collaboration. For these reasons it carries a lower success and higher complication rate, as shown by our data. Despite the technical issues involved, primary PCI offers improved outcomes in this patient group. In the Euro Heart Survey on coronary revascularisation, in-hospital mortality of patients >75 years with ST elevation infarction treated by primary PCI was 8% and in those <75 years it was 4%.16 In a myocardial infarction registry with 8,828 octogenarians (mean age 84 years) in-hospital mortality following primary PCI was 14%.17 In real life, these patients are very rarely treated with thrombolytics and their mortality without PCI is between 23-31%.5,6,15
The impact of a successful PCI versus unsuccessful PCI on patient outcomes was described by the Italian group.18 At the 5-year follow-up, patients with non-optimal PCI results had a higher rate of all-cause mortality (47% vs 19%; P < 0.00001 by log-rank test) than those with an optimal mechanical reperfusion result. More than half (52%) of these patients died within the initial month.
Our data show, that primary PCI in the elderly population is equally effective as it is among the younger patients in terms of improving short term outcome. Considering our results and the meta-analysis of the initial landmark trials comparing primary angioplasty (without inter-hospital transportation) versus thrombolysis19, one may conclude that the older the patient, the more he/she benefits from primary PCI: mortality among patients > 70 years was 17% after lytics vs. 5% after p-PCI. The Zwolle trial20 found that in patients > 75 years, 2 year mortality was 33% after thrombolysis vs. 15% mortality after p-PCI. If we summarise the data from randomised trials21 and express them as saved lives per 1000 treated patients, we have these remarkable numbers: P-PCI saves 145 more lives than no reperfusion therapy and 59 more lives than thrombolysis.
For the subgroup of patients with STEMI complicated by cardiogenic shock, the SHOCK trial4 showed an increased mortality in elderly patients (age > 75) who underwent emergent revascularisation (PCI, CABG). The SHOCK trial registry22 however, showed a complete opposite trend. Our data confirm that in-hospital mortality of elderly patients in cardiogenic shock is extremely high (69%) and indicates that the mortality benefit from primary PCI (over thrombolysis) in elderly patients who present already in shock is less visible than in patients without heart failure. This may be interpreted for practice in the following way, that elderly patients with acute myocardial infarction should undergo emergent coronary angiography very early, before cardiogenic shock may develop.
Thus, primary PCI is an effective treatment for the elderly STEMI patients having an especially marked benefit for those presenting without shock. Elderly patients with acute myocardial infarction should undergo emergent coronary angiography as quickly as possible, before cardiogenic shock could develop.
Acknowledgements
This study was supported by the Charles University research project MSM0021620817.
The contribution of all physicians and nurses participating in the PRAGUE trials, and especially of those working at the Cardiocenter Vinohrady, Prague, who contributed to the registry section, is highly appreciated.