I’m sure you’ll understand when I tell you that, since I’ve become Editor-in-Chief of this Journal, there have been countless times when I’ve had to sign a rejection letter. The moment I signed the first one, I was fully aware of how unpleasant it feels to be interrupting the legitimate aspiration of a group of authors to publish their work in EuroIntervention. We have tried to soften the tone of the rejection letter template, to be more personal and empathetic, to try to explain that an unfavourable decision often doesn’t mean your work is not liked, but that it’s just not liked enough. We hope this helps submitting authors understand that they’re in competition with a number of other papers that are all vying to occupy what in the end is a very restricted number of pages.
The truth is that there’s no way to sweeten the pill when it comes to breaking bad news. If it’s any consolation, I can boast a large number of rejection letters in my own career. I know exactly how it feels to think that you’ve been misunderstood, or that you’ve been made fun of because of your long and cumbersome submission – all of which ends with a quick, no escape decision. Just now I’m writing in the wake of yet another rejection, this time from a journal of which I am in such awe that I can’t even pronounce its name. After a day of formatting the paper to comply strictly with the author instructions (not to mention the time I needed to conduct the study and write the manuscript itself), I got a desk reject in 9 hours. This rejection took all my presence of mind to deal with, and I had to remind myself just what it takes to rationalise your frustration in these cases: “Some journals are lucky enough to have a wide choice of authors and simply cannot accept everything”; “Their task is not to judge a paper in an absolute sense, but in a relative sense”; “It is perfectly useless to appeal decisions that recognise reasons of various kinds, not the least the need to follow an editorial strategy”.
All nice words, right? But how it hurts, believe me, I know. And while the pill is difficult to swallow, let’s always remember that on the other side of the rejection there are people who know how it feels, and who are in the difficult situation of having to choose.
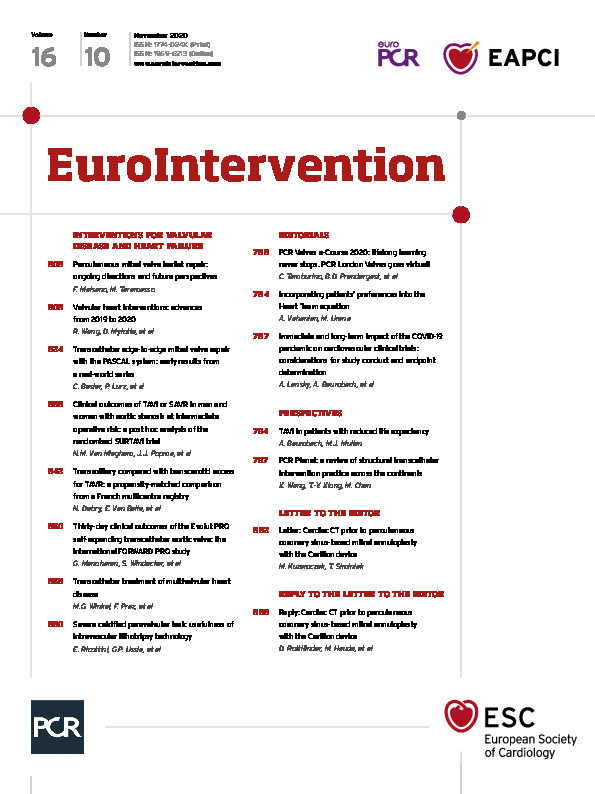
This month’s EuroIntervention highlights the PCR Valves e-Course, made possible thanks to the close and dynamic collaboration with the Course Directors who agreed to be the Guest Editors of this special issue. After the opening remarks by our Guest Editors we have a series of perspectives from international experts invited to comment on critical issues impacting on the treatment of valvular disease today, providing a more global view of the field and offering an interesting balance to the clinical papers that follow. This includes an examination by Alexandra Lansky and colleagues of one of the long-term aspects of the ongoing COVID-19 pandemic – it’s impact on the conduct of cardiovascular clinical trials and on our clinical research at present, and in the future.
Our “dialogue” begins with a perspective by Alec Vahanian and Marina Urena on ways in which the Heart Team can further centre their practice on the patient. They discuss the employment – when choosing among TAVI, SAVR or medical therapy – of a “consensus on decision making” that works by taking into account the different needs and desires of the patients themselves. Continuing with the idea of a more patient-centred approach, Andreas Baumbach and Michael J. Mullen offer their reflections on the choice of TAVI or SAVR in patients with symptomatic severe aortic stenosis (AS) and reduced life expectancy. By taking a more “holistic” view, they consider such parameters as the individual patient’s own desires balanced against their best interest in terms of procedural risk and benefits, bringing into focus the consideration of quality of life as opposed to questions of “mere” survival time in making clinical decisions.
Gender differences in clinical outcomes have been reported in the treatment of symptomatic, severe AS in patients at high operative risk using either TAVI or SAVR. Nicolas Van Mieghem, Jeffrey Popma and colleagues consider this question, evaluating 1,660 intermediate-risk patients who were randomised to either TAVI or SAVR in the international SURTAVI trial. While all-cause mortality or disabling stroke was seen to be similar between TAVI and SAVR for females and males, functional status improvement was more pronounced after TAVI in females. Quality of life and exercise ability for both sexes improved more quickly after TAVI than after SAVR, but after TAVI functional status improvement was more noted in females than in males.
Could a transcarotid (TC) or transaxillary (TAx) access site affect TAVI outcomes? This is the question examined by Nicolas Debry, Eric Van Belle and colleagues in a propensity-matched comparison of a French multicentre prospective registry which included 502 patients, with 374 undergoing TC-TAVI and 128 undergoing TAx-TAVI for symptomatic AS. Patients treated through the TAx access were matched 1:2 with patients treated through the TC route with a propensity score involving 20 clinical, anatomical and procedural variables, as well as by date of the procedure. While the two access sites provided similar outcomes in terms of mortality, stroke or TIA, the TAx access group showed less minor bleeding and fewer main access haematomas than the TC group. They conclude that randomised studies would be of interest.
Ganesh Manoharan, Stephan Windecker and colleagues present the FORWARD PRO study, a prospective investigation in routine clinical practice of the Evolut PRO – a supra-annular, repositionable valve. This international study, involving 629 non-consecutive patients from 39 centres, was independently adjudicated. It demonstrated encouraging outcomes of the Evolut PRO device with a low rate of all-cause mortality at 30 days and a low rate of greater than mild AR.
From Sichuan University, China, Xi Wang, Mao Chen and colleagues provide us with the state of the “PCR Planet” – a look at what is happening worldwide in the field of structural transcatheter interventions. An expert review by Rutao Wang, Darren Mylotte and colleagues looks at the percutaneous treatment of valvular heart disease worldwide, paying special attention to advances made over the last two years. Recent studies which have expanded patient selection into different levels of surgical risk or a wider range of age groups are reviewed. With an eye to the future, the authors consider the evolution not only of specific devices, but also of the impact of improved imaging technologies which provide the Heart Team with new elements to be used in their decision-making process. With valvular heart disease remaining a major societal burden, the authors conclude that our very dynamic field still promises much in the coming years.
Turning to mitral valve repair, a field which has witnessed an increasingly rapid evolution, it is only normal that questions still remain to be answered, while new devices need to be evaluated along with our overall understanding of patient selection as well as operator experience and performance. In their expert review, Francesco Maisano and Maurizio Taramasso look at these different aspects, reviewing ongoing randomised trials, registries and single-centre experiences to pinpoint the state of the art in percutaneous mitral valve leaflet repair today, all of which will be instrumental in further developing, widening and supporting indications for transcatheter edge-to-edge repair in different clinical scenarios in the future.
In terms of clinical research, Christian Besler, Philipp Lurz and colleagues study the real-world and clinical outcomes of the innovative PASCAL repair system, a new device for treating mitral regurgitation (MR) using edge-to-edge mitral valve repair. With fifty patients treated for severe primary or secondary MR, the device was shown to reduce MR effectively in these patients. In most cases, technical and procedural success was obtained, leading to improvements in NYHA functional class. This was a short-term study with a one-month follow-up; future studies will be needed to understand which patients and in which anatomical situations this promising system and device are best suited to reduce MR.
That’s it for this month’s special edition for the PCR Valves e-Course. Before I leave you, the Editorial Board of EuroIntervention would like to join me in thanking the Course Directors of the PCR Valves e-Course for their tireless enthusiasm and dedication which has made both the e-Course, and this edition of the journal, possible.
Supplementary data
To read the full content of this article, please download the PDF.