Abstract
Aims: Acute myocardial infarction (AMI) complicated by unprotected left-main shock (LMS) remains a highly morbid event among acute coronary syndromes. Whether early percutaneous coronary intervention (PCI) in the stent era improves the clinical outcome remains poorly defined.
Method and results: 25 consecutive patients who presented with LMS were treated by primary stenting of bare metal stents for the unprotected left main lesion with an aid of conventional supportive measures. Mean age of the patients was 67 (range, 46-89), 84% were male, with an initial mean systolic BP of 88mmHg (range, 40-120), HR of 82 bpm (range, 38-130), and symptom onset to reperfusion of 4.8hours (range, 1.5-17). An initial TIMI grade 0 flow was noted on the emergent CAG among 56% of the patients, but after PTCA and stenting, TIMI grade 3 flow was obtained among 84%. 30-day mortality was 32%, while one patient underwent emergent CABG for subacute stent thrombosis and 3 patients required elective CABG for residual disease during admission. Among 11 patients who were discharged alive, one required further institutionalization for ischemic brain injury, and the 2 required target vessel revascularization for restenoses. The major adverse cardiac events (death, re-infarction, stroke, and target vessel revascularization) occurred in 68% (17/25) over a 12-month follow-up, including 40% of mortality.
Conclusions: AMI complicated by unprotected LMS could be treated effectively with a prompt application of stenting and result in an acceptable mortality and morbidity.
Introduction
Recent evidence suggests that even the patients with left main trunk (LMT) disease, which has long been considered to be an absolute indication for surgical revascularization (i.e., coronary artery bypass grafting, CABG), could be safely and effectively treated by PCI among the selected group of clinically stable patients1. It remains unknown whether stent-supported PCI could be applied safely to the patients with acute myocardial infarction (AMI) complicated by left-main shock (LMS) on emergent basis.
Method
In the last 7 years, 852 patients with AMI underwent primary PCI for revascularization of the infarct-related artery within 24 hours from symptom onset. AMI is defined as at least two of the following criteria; prolonged chest pain (more than 20 minutes); electrocardiographic changes (ST segment elevation or depression by more than 0.1 mV) in more than two adjacent leads; and creatine phosphokinase myocardial band (CPK-MB) elevation more than double the normal upper limit. Among them, 25 consecutive patients, who presented with LMS, were treated with stenting of bare metal stent for unprotected left main disease.
LMS was defined as the left main disease of ≥70% stenosis and a culprit for AMI shock defined as persistent systolic blood pressure (BP) below 90 mmHg or more than 30 mmHg lower than the baseline systolic blood pressure and signs of systemic hypoperfusion, including clouding of consciousness and sign of oliguria. Hemodynamic abnormalities were defined by Cardiac Index (C.I.) below 2.2 L/min/m2 of body surface area and mean pulmonary capillary wedge pressure (PCWP) more than 18 mmHg by Swan-Ganz catheter. Written informed consent was obtained either from the patient or the family.
Primary angioplasty
Once a diagnosis of cardiogenic shock was made in the emergency room, patients were treated with mechanical ventilation and insertion of IABP after administration of aspirin (162 mg PO) and an intravenous 10,000 units of heparin. IV arginine vasopressin (pitressin 20 U/mL, Sankyo, Tokyo, Japan), and IV dopamine were administered to doses of 0.2 to 0.5 IU/min and DA to doses of 5 to 20 mcg/kg/min, respectively, to maintain mean arterial pressure of more than 70 mm Hg before and during the index procedure. Selective coronary angiography was performed for the limited views once an unprotected LMT disease was recognized, using a non-ionic, low osmolar contrast agent (Iomeron 350, Eizai, Tokyo). Coronary blood flow was graded based on thrombolysis in acute myocardial infarction (TIMI ) classification2.
The LMT lesions are characterized into 4 different types; ostial, body, distal and diffuse types, which are illustrated in figure 1. A single stent was used for the lesions of ostial or body types, and “Y-stenting” or “Culottes stenting” for the lesions of distal or diffuse types, depending upon the anatomy of the lesions. A final kissing balloon inflation was universally applied at high pressure (>12 atm) in the left main bifurcation for the lesions of distal or diffuse types. All patients received aspirin (243 mg/day, indefinitely) and ticlopidine (300 mg/day for 4-6 weeks) after the procedure.
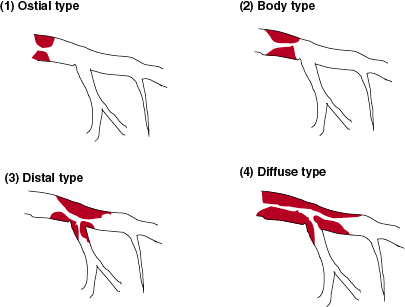
Figure 1. Four different morphology of the left main lesion of (1) an ostial type (2/25), (2) body type (7/25), (3) a distal type (8/25), and (4) a diffuse type (8/25). Corresponding mortality at 12 months for each type was 50%, 28%, 37.5% and 50%, respectively.
The patients were followed clinically and information was collected on death of any cause, stroke, MI, and target lesion revascularization (TVR) either by PCI or CABG.
End-point of the study
The primary end point of the study was mortality and major adverse cardiac events (MACE, consisting of any death, MI, stroke and TVR) over the 12 months follow-up. Hierarchical analysis was applied for predefined events.
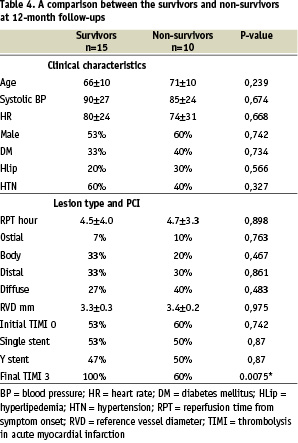
In comparison with the survivors (n=15) and non-survivors (n=10), continuous variables were summarized as means±SD and were compared by Student t tests between the groups. Categorical data were expressed as percentages and evaluated by the chi-square or Fisher exact test when appropriate. Data were analyzed using commercially available statistical software (Stat View 5.0, Abacus, Berkeley, CA, U.S.A.). A value of P < .05 was considered statistically significant.
Result
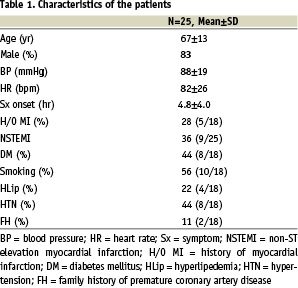
Patients’ characteristics (Table 1)
Mean age of the patients was 67 years predominantly male population (83%), with a mean time from symptom onset to reperfusion of 4.8 hours. Initial systolic blood pressure upon arrival in the Emergency Room was 88±19 mmHg, HR of 82±26 bpm on average. It was of note that 36 percent of the patients developed non-ST elevation myocardial infarction (NSTEMI) at the time of presentation. History of MI was noted in 20%, diabetes mellitus in 36%, smoking in 48%, hyperlipidemia in 24%, hypertension in 44% and family history of premature coronary artery disease in 12% of the patients.
Angiographic characteristics
A mean number of other vessel involvements except for LMS was 2.1. Predominant initial TIMI flow grade was 0 in 56% (14/25), with a 4 different morphology of the left main lesion of an ostial type 8% (2/25), body type 28% (7/25), a distal type 32% (8/25) and a diffuse type 32% (8/25). With a combination of mechanical ventilation, IABP support, IV fluids, IV arginine vasopressin and catecholamine administration, 22 patients (88%) had maintained more than 70 mmHg of the mean arterial pressure at the conclusion of the procedure. The remaining 3 patients, who could not achieve the mean arterial pressure, failed to result in TIMI grade 3 flow at the conclusion of the PCI.
Coronary interventions
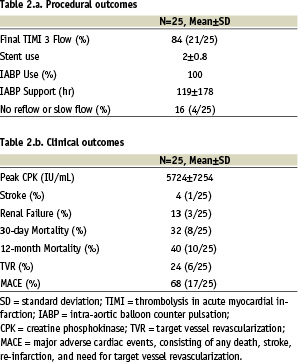
Single stent, in which predominant stent was NirTM stent (Boston Scientific, MN, USA, n=8) among the 13 stents deployed, was used for 2 cases of the ostial type, 7 cases of the body type, and 4 cases of the diffuse type. The reason for a single stent for diffuse disease was non-dominant left circumflex artery (i.e., stenting from the left main to the LAD, n =2), calcified ostial lesion of the left circumflex artery (n=1), and chronic total occlusion of the left anterior descending artery (i.e., stenting from the left main to the LCX, n =1). Y-stent deployment, in which predominant stent was S 600 TM series (Medtronic Inc., USA , n=13) among the 25 stents deployed, was applied for 8 cases of the distal type, 4 cases of the diffuse type. Stent was successfully deployed in all cases on an average use of 2 stents in one patient. TIMI grade 3 flow was achieved in 84% (21/25) of the patients, but the remaining patients resulted in TIMI grade 2 or less, due to no-reflow or slow flow phenomena. IABP was used with an average support duration of 114 hours. One patients developed severe leg ischemia on the side of IABP (of 8F sheath) secondary to advanced preexisting atherosclerotic disease of the femoral artery (Table 2a).
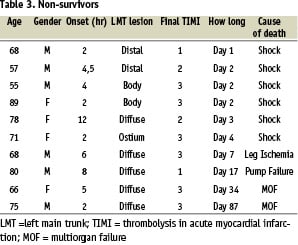
Clinical outcomes
Four patients who did not achieve TIMI grade 3 flow of the LMS died of refractory shock in 3 and of slowly progressive pump failure in 1 (Table 3). Among 21 patients who achieved TIMI grade 3 flow, 6 patients died of refractory shock in 3, of leg ischemia in 1, and of multiorgan failure in 2 (Table 3). Peak level of creatine phosphokinase (CPK) resulted in a mean of 5724 IU/L (range, 2309- 25, 870 IU/L). Renal failure, defined as an increase of serum creatinine >2 mg/dL or need for hemodialysis during admission, developed in 12%. Mortality for each left main lesion type was 50% of the ostial type, 28% of the body type, 37.5% of the distal type and 50% of the diffuse type (p=0.763, p=0.467, p=0.861 and p=0.484 in comparison of survivors and non-survivors, respectively. Table 4).
Among the initial survivors after PCI, one patient developed recurrent MI due to subacute stent thrombosis at 6 th day of admission and underwent emergent CABG. Three patients underwent elective CABG, whose coronary anatomy of the remaining disease was deemed unsuitable for PCI. All who required CABG during index admission survived operation and were discharged alive without any clinical consequences. One patient required institutionalization for ischemic brain injury resulting from prolonged cardiopulmonary resuscitation (>30 min) on admission.
Radionuclear ventriculography among the survivors revealed a mean left ventricular ejection fraction (LVEF) of 34%( range, 25-39). 10 patients who underwent follow-up coronary angiography at a mean of 4 months, 2 patients required revascularization; one underwent PCI for restenosis (_50% of the diameter stenosis) of the proximal LAD and one underwent CABG for LMT restenosis (figure 2). 30-day mortality was 32%, and 12-month mortality of 40%. Overall MACE, consisting of any death (10/25), MI (1/25), stroke (1/25) and TVR (6/25), were recorded in 68% (17/25) over the mean of 12 months follow-up (range, 9-24) (Table 2b).
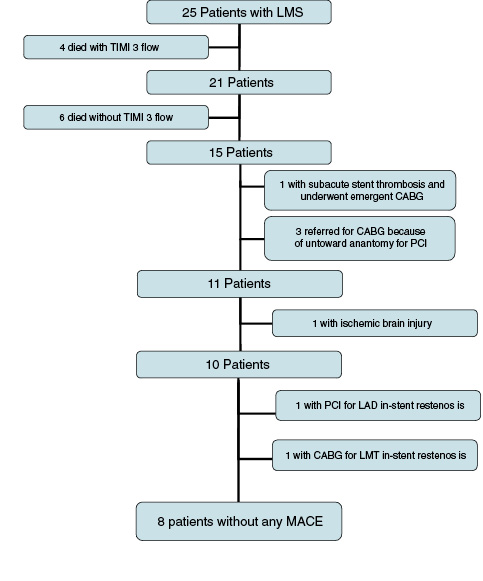
Figure 2. Clinical outcome over 12-month follow-ups; LMS = Left Main Shock, MACE = Major Adverse Cardiac Events, consisting of any death, MI, stroke and target vessel revascularization either by PCI or CABG
Discussion
LMS has the highest mortality of 69 to 94% among the patients with CS complicated by AMI3,4. As in the case of elective PCI for stable effort angina or unstable angina, unprotected left main disease in AMI setting has been considered one of the contraindications to PCI5. There is a paucity of data, however, regarding the clinical outcomes of LMS patients undergoing emergent CABG or PCI.
Ellis et al. reported treatment of unprotected LMT stenosis in the multicenter registry in which patients with LMT disease and AMI were treated by PCI with balloon angioplasty (75%), stents (18.8%), and DCA (6.7%), resulting in 75% of angiographic success of revascularization and TIMI grade 3 flow and 69% (11/16) of in-hospital mortality3.
Although anecdotal report of successful emergent CABG for unprotected LMS appeared in the literature6, operative mortality in such patients remains not elucidated in substantial numbers. Recently, Marso et al. reported there series of the PCI for the unprotected LMT disease during AMI in which 92% (37/40) presented with cardiogenic shock, resulting in 70% (16/23) in-hospital mortality of balloon angioplasty group and 35% (6/17) in the stent treated group7. They used a single stent in most of the cases, consisting predominantly of Palmaz-Schatz and Wiktor stents. The 12 months rate of death or CABG was 83% and 58% for the balloon angioplasty and stent groups, respectively (p = 0.04). Therefore, there seems reasonable to speculate that prompt revascularization for unprotected LMS is related to better clinical outcomes and that stent, not balloon angioplasty nor CABG appears to be contributing to those improving outcomes.
Although 12-months mortality of 40% in the study population seems to be quite promising, significant contributing factors for improving clinical outcomes appeared to be related to the hemodynamic control in the periprocedural period by mechanical and pharmacologic support. Arginine vasopressin (VP), which is secreted from the pituitary gland and raises blood pressure by increasing resistance of capillaries and arterioles, is reported to be effective in maintaining blood pressure in catecholamine-resistant vasodilatory shock after cardiac surgery8 and in increasing the chances of resuscitation for an out-of-hospital cardiac arrest9. Therefore, sustained effect of VP might have been advantageous in terms of maintaining the coronary perfusion pressure after stent deployment and have helped to avoid the overdosage of dopamine, which might further have aggravated the myocardial oxygen demand. Although disadvantages of “Y stenting” or “Culottes stenting” in terms of complexity of the procedure and of increase in metallic surface area with potential of thrombotic occlusion do exist in treatment of distal lesions of the left main trunk, advantages obtained such as maintenance of luminal patency and adequate coronary perfusion would outweigh the disadvantages with the advent of recent antiplatelet therapy for stenting consisting of aspirin, ticlopidine and more recently clopidogril10. In fact, achievement of TIMI grade 3 flow was the only variable to show the significant difference in comparison between the survivors and non-survivors of the study.
Acute thrombotic occlusion of the stent was rare. As a result, 60% (15/25) of the patients survived hospital discharge and 56% (14/25) of them returned to their daily lives. Long term clinical outcomes were also remarkable in terms of no additional mortality and only 2 patients required PCI and CABG, respectively, given the grave prognosis of this high-risk subset of the patients. Since the initial strategy of stent-for-all the left main lesions appeared to minimize the time loss of reperfusion to the myocardium compared with emergent CABG and to clarify the risk of the lesion anatomy, elective CABG was later selected for the PCI-unsuitable lesion morphology, once the patients were stabilized. The approach had further contributed to narrow down the patients best suited for PCI in the case of restenosis and this might have been a factor associated with a low restenosis rate among the survivors. On the other hand, significant number of the patients (6/25) who achieved TIMI grade 3 flow by the stent deployment could not sustain recovery, which will highlight the limitation of our understanding and treatment strategy in the AMI complicated by cardiogenic shock. With the advent of revolutional development of drug-eluting stent (D.E.S.), wider application of D.E.S. for AMI and LMT disease appears quite promising for both short- and long-term outcomes11,12. Therefore, primary stenting as a means of prompt revascularization for the unprotected LMS could not only provide the chance for survival, but also serve as a basis of therapeutic option even in a limited resource utilization system.
Limitations
This is a small report of observational nature, derived from a single center. Besides higher rate of respiratory control and prolonged use of IABP suggested need for enormous systemic support even after successful revascularization. Drug-eluting stents and clopidogril were not approved for clinical use during the study. Further study is needed to confirm our results in a more large scale trial for the patients who are most in need of help to survive.
Conclusions
With the advent of stent technology and conventional supportive measures combined, unprotected left-main shock syndrome could be treated safely by a judicious use of bare metal stent, resulting in an acceptable mortality and morbidity. Further improvement of long-term outcome would be expected in the contemporary drug-eluting stent era.

