Why should cardiologists get involved?
Many are the reasons supporting the involvement of interventional cardiologists in peripheral interventions. First of all, coronary, peripheral and carotid disease are manifestations of the same systemic disease (atherosclerosis), sharing the same pathogenesis as well as the predisposing factors. Coronary atherosclerosis management represents the core activity of interventional cardiologists and they have a profound knowledge of the management of the risk factors for atherosclerosis. In addition, the patterns of catheter-based treatment and complication management are similar, and interventional cardiology is the only specialty focused exclusively on catheter-based endovascular interventions. Moreover, the same patient may have multiple manifestations of atherosclerosis (multilevel disease) and patients are delighted if the same doctor can take care of their multiple pathologies. Finally, although the patient seeks out medical attention because he complains of claudication, his long-term prognosis will be ultimately determined by coronary artery disease.
Of course, the target organs (e.g., heart, brain or kidneys) as well as the anatomy and physiology of the arterial supply are different. Therefore, dedicated training is necessary for an interventional cardiologist before embarking in peripheral procedures. Based on the extended life expectancy of patients, the association of symptomatic atherosclerosis with age and the increased prevalence of cardiovascular risk factors like obesity and diabetes, one would expect to see a massive increase in peripheral procedures performed by cardiologists. However, this does not seem to be the case, at least in Europe, with important differences within the various vascular districts treated. Nobody questions the right to make any attempt to spare patients with critical limb ischaemia devastating amputations, and these procedures have shown a steady growth, only limited by the time requested for the specialists treating these patients (diabetologists, geriatricians, vascular medicine specialists, primary care physicians), to realise the potential benefit offered by these procedures. For carotid and renal stenting, however, the situation has been very different.
The case of carotid artery stenting
Official numbers for Europe are missing, but it is a common belief that in Europe the total number of carotid stenting procedures have levelled off or have slightly decreased in the past decade while in the USA the rise has been far less impressive than expected.1,2 Your President had the privilege to be present during that pioneering era when Gary Roubin introduced carotid stenting3 and took advantage of the more liberal European legislation to come to Milan and gain experience on the use of filters to reduce the most fearsome complication of stenting, distal embolisation and periprocedural stroke. Many technical improvements have occurred since that time when he was using Wallstents and thick peripheral over-the-wire balloons. Dedicated self-expanding stents have become so flexible and miniaturised that they can be easily delivered in very tortuous anatomies. The techniques of prevention of distal embolisation have gained widespread application, and now proximal occlusion devices allow for prevention of distal embolisation in high risk lesions from the time of wire crossing. Why then did the rosy prophecies for carotid artery stenting turn out to be wrong? We live in the time of evidence based medicine, and the failure of carotid stenting to prove equivalency with surgical endarterectomy, and the perception that revascularisation offers little benefit over a conservative modern medical therapy explain the difference between expectations and reality.
The interventional cardiology community has been unable to find the energy and the resources to run a carotid “SYNTAX-like” study, a sufficiently large trial involving skilled operators, to establish if and when carotid artery stenting is equal, worse or better than surgery. The existing evidence is based on trials, frequently poorly conceived, too small to lead to conclusive results, performed in centres with insufficient experience with carotid stenting, very slow in enrolment. As a consequence, the results were available at a time when the endovascular approach had changed. With the only exception of the SAPPHIRE and possibly the CREST trials, carotid artery stenting vs. surgery trials originated outside the interventional cardiology world and lacked the design subtleties obtained in years of practice with large randomised trials in our discipline. It is hard to imagine that the minimal lifetime carotid stenting experience required in four of the six randomised trials enrolling over 300 patients was 10 (ten!) procedures and that in the same proportion of studies tutoring was allowed for investigators not meeting those requirements.4 The inexperience of the operators may well have exposed the patients undergoing carotid stenting to a double hazard due to the limited skills and the inability to select appropriate patients for the procedure. Key decisions in the procedure management such as the use of filters was left to the operators’ preference, a completely different approach from the stringent recommendations the upcoming EXCEL trial in left main coronary disease requires to follow limiting enrolment to selected centres where the operators’ competency is carefully tested. Not only is it true that the relative merits of surgery and stenting have never been properly assessed, but also the overall indications to carotid revascularisation (both endarterectomy and stenting) in patients with asymptomatic carotid stenosis have become controversial.5,6 Multiple randomised trials have shown the superiority of surgery over medical therapy in this setting, but people argue that these studies were done at a time when the medical management was clearly insufficient according to current standards (in particular due to the lack of statin therapy). The assumption that an active drug treatment is sufficient to prevent stroke is unlikely to apply to several subgroups of patients (e.g., stenosis >80%, progression of stenosis severity in spite of full treatment, evidence of asymptomatic embolisation on transcranial doppler or MRI) in whom the annual risk of stroke may be higher than commonly estimated and sufficient to justify the risk of mechanical revascularisation.5. Carotid ultrasound has received widespread use for screening of initial atherosclerotic changes, with bedside devices inexpensive and easy to use now available, but has never been tested on as large a scale as a preventive strategy to reduce the number of strokes in patients at risk. The time has come to work together with our vascular surgical colleagues, interventional radiologists and neurologists to develop a trial of revascularisation vs. medical treatment in asymptomatic patients with high grade stenoses using contemporary preventative measures and antiplatelet treatment. Use of to surgery or stenting based on the respective contraindications, selection of skilful operators, a sufficient duration of follow-up to co-compensate for the initial burden of events related to revascularisation, stringent adjudication of events with neurologists populating the clinical event committees and liberal use of imaging are key to succeed. With the continuous reduction in events with both revascularisation and medical treatment, the real challenge is the achievement of an adequate power within the constraints of budget and of limited numbers collectable in experienced centres.
Renal angioplasty: anecdotes and reality
We all can tell a story of a patient with recurrent flash pulmonary oedema and hypertension cured by a renal stent. It makes a nice anecdote to publish or show at meetings but does not impact on the reality of the negative results of clinical trials.7-9 Patients with renal stenosis and refractory hypertension are punished twice: they are denied renal stenting with at least a 30-50% success in helping drugs to control BP, while their renal stenosis contraindicates sympathetic renal denervation treatment. The only hope comes from the presence of ongoing randomised trials with strict inclusion criteria (CORAL, RADAR).
Lower limb angioplasty: a field in need... but not for cowboys
A field open for growth is peripheral artery disease, not only aorto-iliac which is widely accepted as a transcatheter indication but also femoropopliteal and, especially, below the knee treatment for critical limb ischaemia. While again the numbers in Europe are missing, in the United States the endovascular procedures have dramatically increased, and the surgical procedures, as well as major amputations, have decreased.10 (Figure 1) With respect to the specialties involved, the American data show a marked increase of procedures performed by cardiologists and especially vascular surgeons, while the number of procedures performed by radiologists have diminished.11 Here the limiting factor is more about knowledge and specific skills than competition with other specialists, but there are still hospitals and countries where cardiologists are not allowed to get involved. In claudication due to femoro-popliteal disease, the relief offered by femoro-popliteal surgical grafts is usually adequate, but associated with a non-negligible rate of periprocedural morbidity and mortality. With respect to angioplasty, recanalisation of long superficial femoral artery occlusions is technically challenging and prone to restenosis and reocclusion. Better self-expanding and possibly drug eluting stents and paclitaxel eluting balloons may help to improve long-term patency of diffusely diseased superficial femoral arteries. The goal of below the knee revascularisation is not long-term patency, but wound healing and limb salvage. Despite the many similarities between coronary and lower limb interventions, specific training is required. You cannot push wires and balloons to open arteries whose name is unfamiliar to you! We are not at the time of the pioneers and some cases seen in live courses are not enough to cope with a wide variety of anatomical and clinical challenges. Unlike the USA, only a tiny minority of cardiology centres in Europe offer training in peripheral artery disease to their fellows, a self-perpetuating phenomenon. Aclear policy dictating the rules for training in the various endovascular procedures, valid irrespectively of the main field of specialisation, and the development of joint training programs with rotation in vascular surgery, radiology and interventional cardiology should be agreed upon with vascular surgeons, interventional radiologists, and angiologists who also are interested in ensuring a high quality in the preparation of future multi-skilled trainees, and deter cowboys with inadequate backgrounds. We have to learn from our American colleagues who have already developed strict guidelines to ensure competency in some vascular interventions such as carotid stenting.12
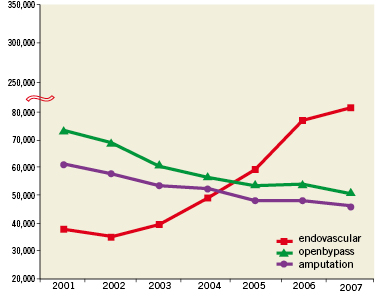
Figure 1. Admissions for peripheral arterial disease and procedures per year. Trends in vascular surgery, endovascular procedures and need for amputations between 2,148,924 hospital admissions in patients with lower extremity arterial disease over a period of seven years between 2001 and 2007, on an average 307,000±18,000 admissions per year. (Adapted from Hong et al10, with permission from Elsevier)
What about AAA?
With dedicated, covered, bifurcated stents for triple abdominal aortic aneurysm (AAA) treatment now miniaturised to 14 Fr-4 Fr smaller than the valve delivery systems and the size of an Impella left ventricular assist device –you wonder why this common pathology with well established elective indications for prevention of sudden rupture does not enter the portfolio of procedures offered by interventional cardiologists. There is nothing wrong with this, but it must come with the same cooperation and agreement with our surgical colleagues that we enjoy in most centres for TAVI. If a cardiologist wants to get involved, he should become part, together with the other specialists above, of a dedicated group for noninvasive peripheral imaging in order to optimise both patient selection and long-term, post-procedural, follow-up. It is not enough to learn the techniques of deployment of these dedicated covered stents in order to repatriate this procedure from what is generally considered to be a surgical realm. Probably the ideal way forward is the training of hybrid operators with a background both in vascular surgery and interventional cardiology and radiology. The same applies to aneurysms of the descending thoracic aorta and post-coarctations treatment (re-coarctation or aneurysms), with the difference that these less frequent pathologies should be left to the few specialists working in strategically located hospitals (post-traumatic aortic rupture is the worst emergency) and hospitals with large adult congenital heart disease programs.
The need for a “Vascular Team”
Similarly to the concept of the “Heart Team”, recently proposed in the coronary revascularisation guidelines of the European Society of Cardiology15, each institution offering treatment for vascular disease should aim at building a “Vascular Team”, composed of interventional radiologists, vascular surgeons, angiologists (in the countries where this specialty exists), cardiologists with interest/training in vascular disease management, neurologists, nephrologists and internal medicine specialists. Cardiologists have much more to offer to the program than their familiarity with transcatheter techniques, starting from their know-how for screening cardiac disease before vascular treatment, the optimisation of secondary prevention and percutaneous coronary revascularisation, if needed. The prerequisite for building such a team is that all the members are treated as peers, and everybody acknowledges the contribution the others bring to improve patient care. Appropriate guidelines encouraging and eventually mandating this cross-fertilisation and cross-training can offer hope of better treatment to many patients and avoid needless frustrations.
Cardiologists are condemned to learn more about peripheral disease
The ability to advance and deploy in crossover a 6-8 mm peripheral balloon, an appropriately sized self-expanding stent or covered stent in the iliac arteries (or subclavians) is an important contribution expected from the interventional cardiologists working for transcatheter aortic valve implantation procedures. Treatment of hypertension is part of the daily cardiology practice. It will be ironic if the boom in renal denervation treatment consequent to the convincing data of the SYMPLICITY trials13,14 benefits other specialists who are not involved, or less involved, in the diagnosis and medical management of this condition as well as the monitoring of long-term results of the procedure. If non-refractory hypertension, heart failure and other conditions such as diabetes are added to the list of potential indications for renal denervation therapy, be ready: you may need to prolong the opening hours of your cathlab and hire new personnel.