Abstract
Aims: Target lesion revascularization (TLR) rates of bifurcated lesions (BL) remain high, mainly due to side branch (SB) restenosis, even when drug-eluting stents (DES) are used. The aim of our study was to evaluate long-term clinical outcomes of a stepwise approach with single bare metal R stent implantation for BL.
Methods and results: In 465 patients, PCI was performed using a double guide wire, single stent in main branch (MB), and angioplasty of the SB, aiming at an optimal angiographic result of the MB and an optimal functional result (TIMI 3 flow) of the SB. 105 patients were treated for a true bifurcated lesion (TBL) and 360 patients were treated for a lesion with involvement of a significant side branch (ISB). Procedural success was achieved in all TBL and in 99% of ISB. At 1 year clinical follow-up, 8.6% treated for TBL had clinically driven TLR, 7.6% underwent repeat PCI, 1.0% underwent CABG. For patients treated for ISB, 13% had clinically driven TLR, 9.4% underwent repeat PCI, 3.6% CABG. 4 patients treated for TBL suffered non-fatal MI vs. 20 patients treated for ISB. Cardiac death occurred in 1.9% and 2.5 % respectively.
Conclusion: A simple approach in the percutaneous treatment of BL using a single bare metal R stent results in good 1 year clinical outcome comparable to the outcome reported following DES implantation.
Introduction
Percutaneous coronary interventions (PCI) of bifurcated lesions are increasingly performed in daily clinical practice. It has been estimated that treatment of bifurcation lesions accounts for 15% of all current PCI’s. PCI of bifurcated lesions is associated with lower procedural success rate, an increased rate of subsequent major adverse cardiac events (MACE) and restenosis, particularly when both the main branch and the side branch are stented1-6. The arrival of drug-eluting stents (DES) have significantly reduced the risk of restenosis in single de novo coronary lesions. However, only a few studies have evaluated the treatment of bifurcated lesions with DES. Even when using a DES, restenosis of the side branch remains a significant problem7. One of the limitations of DES in bifurcated lesions is that with the application of a “crush” or “culotte” technique, the region of double/triple layer of stent is increased, which may lead to increased local dosage of drug with subsequent impairment of endothelial function8. In addition, using a complex technique may be associated with an increased risk of stent thrombosis9-11. Furthermore, future access to the side branch re-crossing the struts with a guide wire/balloon may be difficult.
Many different treatment strategies have been proposed like “classic T-stenting”, “Y stenting”, “culotte or Trouser stenting” and “crush stenting”, but the optimal treatment of bifurcated lesions remains unclear. Only few randomised trials have been conducted and all these complex and time-consuming techniques have shown disappointing outcomes with decreased procedural success rates and increased restenosis and the need for target lesion revascularization (TLR)2,9,12-14.
Studies comparing stenting both branches versus stenting the main vessel and a balloon dilatation of the side branch show that the latter approach with a single stent is more simple and superior when using bare metal stents1-6,15-17. Major cardiac event rates at follow-up were significantly higher when the side branch was stented15,18-20. In addition, there is evidence that functional rather than angiographic success of the side branch may determine immediate and long-term procedural results, as demonstrated by the excellent
6-months patency when side branches are jailed by a single stent21.
Dedicated bifurcation stents such as JoStent, Devax Acces Stent, ML Frontier™ stent, DBS stent, Bard-XT Carina stent, AVE bifurcation stent and AST SLK-view stent have not shown a significant reduction in restenosis rates yet22-24. They are more difficult to deliver and require larger guiding catheters.
The RESTOR trial showed that treatment of a single de novo coronary lesion with the bare metal R stent is safe and effective in patients with stable and unstable angina pectoris25. In bifurcated lesions the R stent is suitable and provides good wall coverage, radial strength, conformability and as a consequence of its strut design, provides easy side-branch access26. The aim of our present single centre study was to evaluate one year clinical outcomes of the treatment of bifurcated lesions using a simple PCI technique and a single bare metal R stent.
Methods
Study design
Inclusion of this single centre study started in 1997 and was completed in 2004. We included 465 consecutive patients treated with a PCI for a bifurcated lesion with an R stent and a 3-step approach with aim to protect the side branch using a second wire. Patients with a bifurcated lesion in a native coronary artery undergoing a clinically indicated elective PCI for stable angina or for a non-ST-elevation acute coronary syndrome were included in this study. Patients undergoing primary PCI for ST-elevation myocardial infarction were excluded. Patients with a known allergy for clopidogrel or suspected thrombotic disorder or hemorrhagic disease and patients with extremely tortuous or calcified lesions that would reduce the chance of successful stent delivery were not included.
R stent
All patients were treated with a bare metal R stent (OrbusNeich, Fort Lauderdale, USA) in the main branch with provisional stenting of the side branch. The available sizes of the bare metal R stent in diameters were 2.5, 2.75, 3, 3.5, and 4 mm with a length of 9, 15, 18, and 23 mm. Bare metal R stents with diameter 3, 3.5 and 4 mm were also available with a length of 28, 33 mm. The coronary bare metal R stent has a modular structure with the centre zone consisting of a continuous dual helix lattice. This configuration provides omni-directional flexibility and high radial strength. The cells in this region can be expanded up to 4.5 mm in diameter of all available sizes and lengths to enable excellent side branch access (Figure 1).
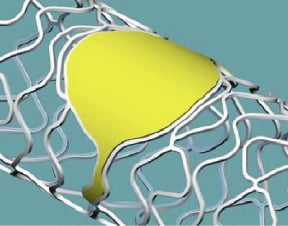
Figure 1. Ring and coil design of R stent providing good side branch access.
With side branch dilatation through a strut, distortion of other stents occurs on the contra-lateral section of the stent, often lifting a part of the stent off the vessel wall. The design of the R stent offers cells that act independently, minimizing these distortional effects.
Interventional procedure
All patients routinely received 5000 IU of unfractionated heparin and the femoral or radial access route was used. Bifurcated lesions were treated using a 3-step approach. After placement of the guiding catheter, 2 wires were introduced in the distal bed of the 2 branches. All lesions were pre-dilated in the main branch and, in case of a true bifurcated lesion (TBL), the side branch was pre-dilated with balloon angioplasty. After dilatation of the side branch, a bare metal R stent was placed in the main branch, covering the ostium of the side branch and jailing the side branch wire. After this, the stent was re-crossed through the struts by re-introducing a guide wire in the origin of the side branch and subsequent opening of the struts or “fenestrating” for second dilatation of the side branch. The aim was to achieve <50% diameter stenosis in the side branch, but residual stenosis >50% was tolerated in case of TIMI 3 flow at the end of the procedure without significant dissection or stasis of contrast medium (optimal functional rather than optimal angiographic success). In case of TIMI flow <3 in the side branch, additional prolonged dilatations were performed. The protocol included provisional side branch stenting only in case of a significant dissection in the side branch occurred or in case of TIMI 3 flow was not achieved in the side branch. Kissing balloon technique was performed to end the procedure in all TBL and was left to the operator’s discretion for lesions with involvement of a significant side branch (ISB). Patients were treated with aspirin 100 mg and 75 mg Clopidogrel daily for one month after PCI and aspirin 100 mg thereafter.
Follow-up
Follow-up was obtained after verifying patient’s vital status, by sending a questionnaire 12-14 months after the procedure. In case of no reply, a telephone contact with the patient or the patient’s relatives were used to complete follow-up information. In case a major adverse cardiac event was reported, review of hospital records, chart review, telephone contact with the referring cardiologists or the patient’s general practitioner were used to complete information. Patients with residual or recurrent anginal symptoms requiring repeat revascularization procedures were referred to our institution, and data regarding these procedures were collected.
Definitions and endpoints
A true bifurcated lesion (TBL) was defined as ≥ 50% narrowing of the vessel diameter involving both the main and side branch, based on visual assessment on the angiogram (ICPS lesion classification type 1)2. A bifurcated lesion with involvement of a significant side branch (ISB) was considered when, during PCI the side branch was considered large enough to be protected with a double wire.
The primary endpoint was target lesion revascularization (TLR) at one year follow-up, defined as revascularization of the target lesion, either in the main branch, the side branch, or both, within 5 mm margins proximal or distal to the initial lesion or stent by either repeat PCI or coronary artery bypass grafting (CABG). TLR was undertaken in the presence of either anginal symptoms or objective evidence of ischemia. Any CABG involving the target vessel was considered a target lesion revascularization.
The secondary endpoints were procedural success, target vessel revascularization (TVR) and major adverse cardiac events (MACE) within one year. Procedural success was defined as a less than 20% residual stenosis within the main branch and TIMI 3 flow at the end of PCI procedure within the main branch and side branch. TVR was defined as a revascularization of the target vessel. MACE was defined as the composite of death, myocardial infarction, and clinically driven TVR at one year. All deaths were considered cardiovascular unless an unequivocal non-cardiac cause could be identified. The definition of myocardial infarction included documented elevation of cardiac markers or the development of new Q-waves on the electrocardiogram and also included periprocedural myocardial infarctions with a CK-MB peak larger than two times the upper limit of normal.
Statistical analysis
Continuous variables with normal distribution are presented as mean±standard deviation (SD), categorical variables as number (proportion). Continuous variables were compared using independent sample t test. Categorical were compared with chi-square statistics. A p-value of <0.05 was considered significant. The statistical analysis was performed using the Statistical Package for Social Sciences software (SPSS 12.0 for Windows, SPSS inc. Chicago, Illinois, USA).
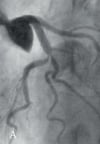

Figure 2. Angiographic images of a true bifurcated lesion in the LAD and first diagonal branch. A: Before PCI. B: Result after PCI with a single bare metal R stent placement in the main branch and balloon dilatation of the side branch, showing significant residual stenosis of the side branch. C: After 6 months follow-up, showing no significant restenosis of the main branch and improvement of residual stenosis of the side branch.
Results
Baseline demographics and procedural data
Table 1 summarizes the clinical characteristics and bifurcation lesion location of the patient population with TBL (n=105) and ISB (n=360).
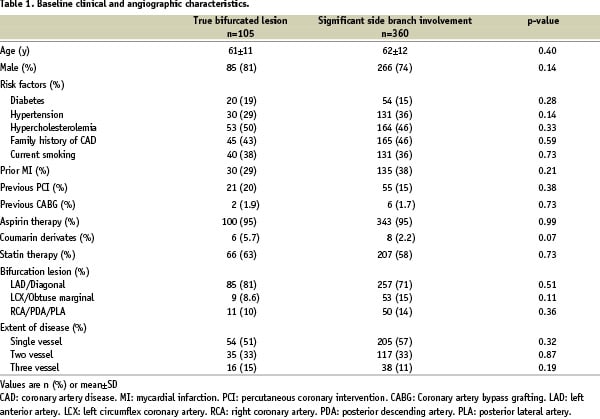
Although not significant, the two groups show small differences in the proportion of hypertensives, prior MI and bifurcation lesion treated. Lesion characteristics and procedural data of TBL and ISB are summarized in Table 2.
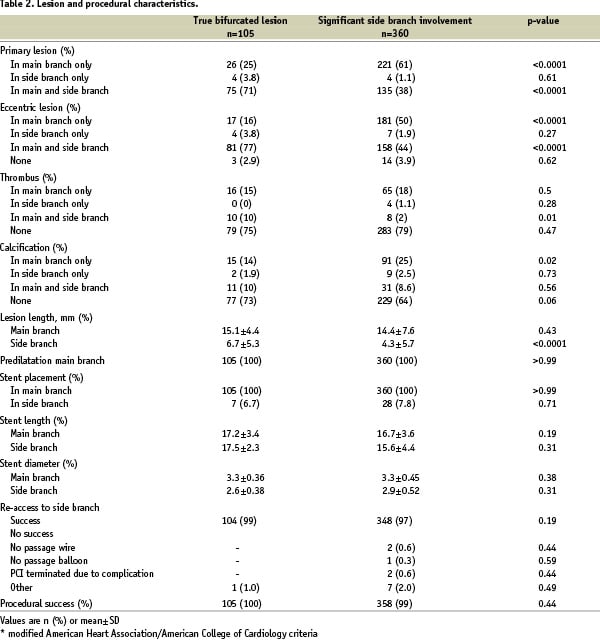
There are significant differences in primary lesion and eccentric lesion for the two groups. The lesion length of the side branch of TBL was significantly larger.
After stenting the main branch, provisional stent placement was applied in 7 patients treated for TBL versus 28 patients treated for ISB. Successful re-acces to the side branch was achieved in 99% of TBL and in 97% of ISB. Procedural success at the end of PCI procedure was achieved in all patients of the TBL group and in 99% in the ISB group.
At 1 year follow-up (range 9-14 months), 12% of all patients underwent clinically driven TLR (Table 3), 42 of whom underwent repeat PCI and 14 underwent CABG.
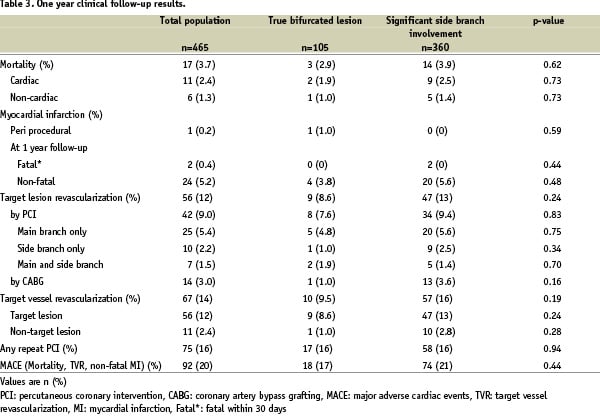
Clinically driven TLR in patients treated for TBL was 8.6%, 7.6% underwent repeat PCI and 1.0% underwent CABG. Clinically driven TLR in patients treated for ISB was 13%, 9.4% underwent repeat PCI and 3.6% underwent CABG (Table 3). TLR was mainly performed in the main branch.
In our population 5.2% of all patients suffered from a non-fatal myocardial infarction, 3.8% in patients treated for TBL and 5.6% in patients treated for ISB. One patient suffered from a periprocedural myocardial infarction and 2 patients had a fatal myocardial infarction within 30 days after PCI.
When comparing cardiac death in both groups, the incidence in patients treated for ISB was slightly higher than in patients treated with for TBL: 1.9% and 1.0% respectively. (Table 3) Total MACE was 20%; 17% in patients treated for TBL group and 21% in patients treated for ISB.
There were no significant differences in outcomes between the two groups. Univariate analysis was performed to detect independent predictors for clinically driven TLR. None of the factors examined were associated with TLR.
Discussion
The results of this single center, prospective study showed favourable long-term outcomes of clinical follow-up with low TLR rates for PCI in bifurcated lesions, as achieved with a stepwise approach using a single bare metal R stent aiming at optimal angiographic result in the main branch, combined with optimal functional result in the side branch (that is accepting significant angiographic residual stenosis when flow is optimal).
This is a large study of bifurcation procedures that prospectively included patients with a single, stepwise approach using one type of stent design. Treatment strategies in bifurcated coronary lesions
are still subject of debate. The discussion is mainly focussed on the application of techniques with the use of one or two stents, the choice of a bare metal stent or a DES, and on the use of the most proper device in terms of favourable procedural outcomes. Previous studies comparing treatment of bifurcated lesions using one or two stents demonstrated TLR rates in favour of a simple approach. Anzuini, et al.3 compared 90 patients treated for TBL with a Wiktor
stent using the “T” technique. Stent placement in the side branch resulted in a significantly increased TLR rate at 8±2 months follow-up (35.5% versus 15.5% after stenting the main branch only). Yamashita et al.6 treated 92 patients using one or two stents and applied additional techniques such as pre-treatment of lesions with debulking devices. After 6 months TLR rates were similar in the two groups (38% vs. 36% using two stents). Pan et al.16 treated 126 patients with a bifurcated lesion with a stepwise strategy similar as in our study. After stenting the main branch, compromise of the side branch persisted in 91 (72%) patients and additional dilatation had to be performed. Eventually, significant side branch stenosis remained in 12 patients in whom 5 patients provisional stenting was successful. At 15 months follow-up TVR rate was 15%. In addition, Assali et al.15 evaluated stent placement in one or two branches using a bare metal stent in 50 patients and found clinically driven TLR rates of 37.6% with two stents compared to 5.6% using 1 stent. Our results of this study confirm that favourable clinically driven TLR rates can be achieved using a single bare metal R stent. When comparing TLR rates, our results show low TLR rates for both the main and the side branches, whereas most studies show high angiographic restenosis of the side branches3,6,7. In our study, however, TLR was mainly performed in the main branch. Repeat angiography was only done if clinically indicated. Explanation for low clinically driven restenosis or re-occlusion of the side branch could be the fact that this often occurs asymptomatically.
At present, DES have not provided a satisfactory answer for bifurcated lesions. While several DES trials indicate lower bifurcation restenosis in the main branch, restenosis of the stented side branch often occurs. Colombo, et al.7 evaluated a sirolimus-eluting stent (SES) in bifurcated lesions. Patients were randomly assigned to either stenting both branches (group 1) or stenting the main branch with provisional stenting of the side branch (group 2). At six month follow-up clinically driven TLR rate in group 1 was 11.1% versus 4.5 in group 2. Angiographic follow-up showed 21.8% restenosis of the side branch in group 1 versus 14.2% in group 2. Another study by Hoye et al.27 compared treatment with a sirolimus or paclitaxel-eluting stents (PES) in 208 patients with a de novo bifurcated lesion, showing survival free of TLR at 6 months in 95.7% for SES and 86.8% for PES with stent type being the only independent predictor. Survival free MACE at six months was 93.7% for SES and 85.8% for PES. Using different stenting strategy (T-stenting, crush stenting, culotte stenting and kissing stenting) did not result in significant differences in clinical outcome. Our study shows comparable clinically driven TLR rates as in DES using a single bare metal R stent. Although MACE rates are higher in our study when compared to Hoye et al., our follow-up period was longer. In addition, the R stent may be preferred because of better access to the side branch in case of restenosis.
Stent thrombosis in bifurcated lesions treated with a DES seems to be a concern. A study by Ge et al.10 using a crush technique in 181 patients with a bifurcated lesion, reported an intraprocedural stent thrombosis of 1.7% and a postprocedural stent thrombosis of 2.8% (1.9% treated with SES and 4.0% treated with PES) at 9 months follow-up. Although, 1.7% incidence of postprocedural stent thrombosis occurred in patients who did not continue dual antiplatelet therapy, the authors stated that the data seem to point out a higher risk of stent thrombosis when two DES are implanted in a bifurcation lesion. In addition, they stated that there is a strong need to adhere dual antiplatelet therapy for a currently unknown time period. In 28 patients Hoye et al.28 studied bifurcation stenting utilizing the Culotte technique with drug-eluting stent implantation. In this study there was a stent thrombosis rate of 0%. Using a “crush” technique may lead to an increased local dosage of drug with subsequent impairment of endothelial function. This may increase the risk of stent thrombosis compared to a single stent strategy. However, published results are from non-randomised studies with only small numbers of stent thrombosis. Thus, the available data are too small to substantiate a definite statement9-11,28. In our study we had no patients with acute stent thrombosis. Unfortunately we have no angiographic data of subacute stent thrombosis in our population.
In the near future the Genous Bio-engineered R stent with murine monoclonal anti-human CD34 antibodies on the stent surface capturing Endothelial Progenitor Cells (EPC) for accelerated natural healing will be available. This may further reduce restenosis rates in bifurcated lesions. In a multi centre, prospective trial, the HEALING II (Healthy Endothelial Accelerated Lining Neointimal Growth), demonstrated the safety and efficacy of the Genous Bio-engineered R stent in single de novo coronary artery lesions. An interim analysis showed that EPC titer directly correlates with angiographic and IVUS outcome and identifies patients likely to respond to EPC capture stenting. The TLR and TVR events were restricted to the low EPC group and patients without statin therapy at the time of implant were generally restricted to the low EPC group with significant late loss29.
The optimal stent design has remained elusive. In the past, a number of dedicated stents that were capable of complete and immediate coverage of the bifurcated lesion are produced9,12,30-33. Clinical use of these devices requires great expertise of the operator9,24,31-33. In our study we used a simple technique for interventionalists in the treatment of bifurcated lesions. Successful stent delivery was achieved in all patients. Provisional stenting of the side branch had to be performed in 28 patients treated for ISB and 7 patients treated for a TBL. Kissing balloon technique was preferred at the end of procedure. In this study high rates of procedural success were achieved using a simple approach in the treatment of bifurcated lesions with PCI. In addition, the design of dedicated stents not always fit the coronary anatomy in 3D dimension decreasing side branch accessibility. Melikian et al.34 reviewed that side branch accessibility, can be complicated by wire entanglement and suggested to use a third wire to maintain the patency and to facilitate access to the side branch. The cells of the R stent can be expanded up to 4.5 mm in diameter providing good side branch accessibility. In addition, the cells of the R stent act independently in minimizing distortion when the struts are opened through balloon angioplasty. Therefore, this simple technique with a single R stent can be applied in a large variety of bifurcated lesions.
The main limitation of this study is the single centre, non-randomised design. In addition, routine angiographic follow-up data was not obtained and therefore, restenosis giving rise to minimal or no symptoms, particularly of the side branch, cannot be excluded. However, clinical follow-up data was obtained in > 99% of patients, representing all clinically driven major adverse cardiac events. A larger multicentre registry is needed to assess the validation of this study, which is currently in preparation in our institution. A simple approach of bifurcated lesions with a single bare metal R stent avoids side branch stenting in many patients and provides favourable long term clinical results, even compared to DES.

