A few months ago, I spoke to you about the familiar feeling that came back to me when I attended the ESC Congress in person after two years of digital conferences. The return to TCT, however, was a different kind of experience due to the presence of numerous innovations compared to how I remembered that meeting before the pandemic. For the first time, TCT was being held in Boston, with a new team of Course Directors and the absence of some of the classic and characteristic elements that we had gotten used to in these meetings, starting with the Main Arena and traditional rooms for presentations and symposiums.
This deconstruction of conventional spaces is a trend that is beginning to be seen more often. Presentations take place less often between four “clear” walls but are delivered instead in an open space with technologically advanced stages and a multitude of nearby chairs. At the ESC Congress, we would call them “Hubs”, and anyone who has been there recently knows what I mean. Perhaps this is a solution dictated by the need to avoid poorly ventilated environments due to the COVID-19 rules?
Around this idea of open spaces, which for me is very successful, hovers the unknown factor of audio and that of echoing sound, as we are talking about spaces set up without a physical separation between one session and another, but all in all I believe I can say that this is another bet won by the organisers.
This year, the late-breaking trials (another key feature of TCT) were presented in one of these open environments rather than in the traditional Main Arena. Some of the more nostalgic among us missed the Main Arena, while others considered the new idea disruptive and in step with the times.
EuroIntervention was there for the first time. We sponsored a session and also had three presentations during the Congress that we simultaneously published online. The synergy of the Journal with all these “restarted” in-person events is an opportunity that the pandemic has deprived us of up to now and we are determined to exploit it to the full.
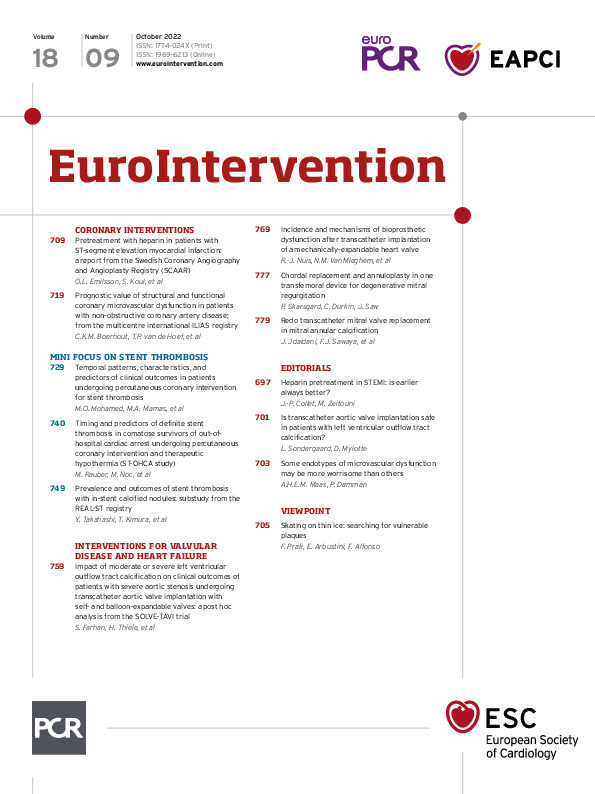
Of course, in parallel, we continue with passion to make the Journal with a collection of the best articles. Here are the ones in this issue.
We begin in coronary interventions with an article from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). Oskar Love Emilsson, Sasha Koul and colleagues studied the outcomes in ST-segment elevation myocardial infarction (STEMI) patients who had been pretreated with unfractionated heparin (UFH) before percutaneous coronary intervention (PCI). The authors found that UFH pretreatment was associated with a reduced risk of coronary artery occlusion without an increase in the risk of major in-hospital bleeding. The results concerning mortality, while showing a reduced risk, were not sufficiently robust to be confirmed. This article is accompanied by an editorial by Jean-Philippe Collet and Michel Zeitouni.
When evaluating patients with angina and non-obstructive coronary artery disease (ANOCA), what is the prognostic value of measuring coronary microvascular dysfunction (CMD) using coronary flow reserve (CFR) and minimal microvascular resistance? This question was posed by Coen K.M. Boerhout, Tim P. van de Hoef and colleagues who, using the ILIAS Registry, determined that CMD identified by impaired CFR alone was linked to an increase in major adverse cardiac events (MACE) and target vessel failure (TVF) rates whereas microvascular resistance was not. In addition, they concluded that there was no difference in the risk of MACE and TVF between a low CFR with a pathologically increased microvascular resistance (structural CMD) or not (functional CMD) in these patients. This article is accompanied by an editorial by Angela H.E.M. Maas and Peter Damman.
This issue’s mini focus is on stent thrombosis. Mohamed O. Mohamed, Mamas A. Mamas and colleagues looked at procedural outcomes of PCI for stent thrombosis in patients treated in England and Wales, studying the timing of when stent thrombosis occurred, whether within the first 24 hours post-procedure or later, then comparing the characteristics and outcomes of these cases based on this timing. They conclude that the prognosis for these patients clearly changes with different times of occurrence of the thrombosis and recommend an increased use of intravascular imaging in the higher-risk groups where they find intravascular ultrasound and optical coherence tomography to be underutilised.
Martin Rauber, Marko Noc and colleagues studied the occurrence, timing and predictors of definite stent thrombosis in comatose survivors of out-of-hospital cardiac arrest undergoing immediate PCI and therapeutic hypothermia and found stent thrombosis to have a significantly higher occurrence here than in other PCIs. Even with the use of the latest drug-eluting stents (DES) and recommended anticoagulation/antiplatelet treatment, the occurrence of stent thrombosis remained high. The authors note that in a vast majority of these cases, certain clinical signs of stent thrombosis are present such as arrhythmias or haemodynamic deterioration.
Our last article in this mini focus is on stent thrombosis and calcified nodules. Using a prespecified substudy from the REAL-ST registry, Yu Takahashi, Takeshi Kimura and colleagues found that calcified nodules could be one of the mechanisms in stent thrombosis after implantation of second-generation DES leading to higher rates of target lesion revascularisation. They recommend special attention be given to these patients with careful clinical follow-up.
In interventions for valvular disease and heart failure, the SOLVE-TAVI trial authors Serdar Farhan, Holger Thiele and colleagues examined the impact of left ventricular outflow tract (LVOT) calcification on outcomes after transcatheter aortic valve implantation (TAVI) when using either a self-expanding valve or balloon-expandable valve. They found no difference between the two valves in patients with moderate or severe LVOT calcification in terms of midterm adverse clinical outcomes. However, TAVI in these patients, regardless of the valve type used, tended to be more challenging with longer fluoroscopy times and an increased need for pre- and post-dilation. This article is accompanied by an editorial by Lars Sondergaard and Darren Mylotte.
Rutger-Jan Nuis, Nicolas M. Van Mieghem and colleagues examined the incidence and mechanism of bioprosthetic valve dysfunction in patients who had TAVI procedures using the LOTUS mechanically expandable valve. While these valves are no longer available, thousands of patients received them and are at high risk for bioprosthetic dysfunction at follow-up. These findings underline the importance of physician awareness of the danger for these patients and encourage us to pay special attention to clinical and echocardiographic signs of bioprosthetic dysfunction in these patients.
We also have one of a continuing series of “Viewpoints” in this issue, this one by Francesco Prati, Eloisa Arbustini and Fernando Alfonso on the ongoing search and challenges in identifying vulnerable plaques.
Now we’ll let the articles speak for themselves.
Supplementary data
To read the full content of this article, please download the PDF.