Abstract
Aim: Percutaneous coronary intervention (PCI) of left main (LM) coronary artery stenosis may become an alternative to the standard therapy, coronary artery bypass graft surgery (CABG). The purpose of the present study was to describe the outcome after LM PCI in three cohorts of patients: patients with low surgical risk, patients with high surgical risk or patients considered inoperable, and patients with acute ST elevation MI.
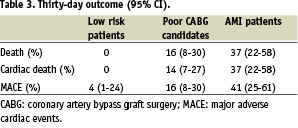
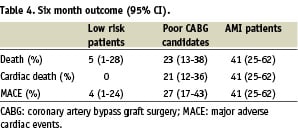
Methods and results: 104 consecutive patients who had LM PCI at the Department of Cardiology, Skejby University hospital between 1999 and 2004 were investigated. The patients were divided into three groups according to PCI indication and operability: surgical low risk patients and suitable lesions for PCI (n=27), poor CABG candidates (age > 80 years, severe comorbidity or inoperability) (n=50), and patients presenting with AMI (n=27). In the three groups mean ages±SD were: 60±14, 76±9, and 68±12 years, respectively. At thirty days follow-up the cumulative incidence of major adverse cardiac events (MACE); cardiac death, MI, or target lesion revascularization (95% CI) were 4 (1-24)%, 16 (8-30)%, and 41 (25-61)%, respectively. At 6 months the cumulative incidence of MACE were 4 (1-24)%, 27 (17-43)%, and 41 (25-62)%.
Conclusions: PCI of LM coronary artery stenosis can be performed with good outcome in patients with low surgical risk and with acceptable outcome in surgical high risk patients or patients considered inoperable. Patients with AMI and culprit lesion in the LM have a high mortality in the acute phase, but mid-term prognosis is good if the patient is successfully treated with PCI. This follow-up study underlines the importance of risk stratification in the heterogeneous group of patients undergoing LM PCI.
Percutaneous coronary intervention (PCI) of unprotected left main (LM) coronary artery stenosis may become an alternative to coronary artery bypass graft surgery (CABG) in selected patients for various reasons: It may be performed as an emergency procedure in patients with acute myocardial infarction (AMI) and cardiogenic shock. It is a treatment option in patients with a high surgical risk or patients considered inoperable, and it can be performed in surgically low risk patients where the LM lesion has suitable anatomy for stenting. Before PCI is considered an alternative to CABG, an acceptable PCI outcome must be documented. In surgically low risk patients only a low mortality and cardiac event rate can be accepted, while a higher level of adverse events may be accepted in a higher surgical-risk subset of patients or in patients considered inoperable. The purpose of the present study was to describe the outcome in three cohorts of patients: patients with low surgical risk (group 1), poor CABG candidates (group 2), and patients with ST elevation AMI (group 3).
Methods
Study population
Patients presenting with significant (>50% stenosis by visual estimation) LM disease, referred to Skejby Hospital, University of Aarhus for coronary revascularization were evaluated by interventional cardiologists and cardiac surgeons. The decision to recommend PCI or surgery was based on: clinical characteristics, suitable anatomy for stenting, quality of peripheral coronary vessels and quality of arterial and/or venous conduits for grafting material. PCI was performed when one of the three following conditions was present:
1. Suitable anatomy for stenting in a patient with a preference for PCI.
2. Suitable anatomy for PCI and absolute or relative contraindications to surgery due to severe comorbidity or high surgical risk. Patients aged ≥ 80 years were considered to be high risk surgical candidates.
3. Acute ST elevation myocardial infarction.
We report the results from 104 consecutive patients who had LM-PCI between January 1999 and December 2004. Patients with previous CABG to the left coronary artery (protected LM) were excluded.
Procedures and medications
Coronary angioplasty and stent implantation were performed according to the practice of complete coverage of the diseased segment. Angiographic success was defined as residual stenosis <30% by visual analysis in the presence of Thrombolysis in Myocardial Infarction (TIMI) flow grade 3. At the start of the procedure, a bolus of unfractionated heparin (at 70 to 100 IU/kg) was administered. Glycoprotein IIb/IIIa inhibitors were used at the discretion of the operator. A loading dose of 300 mg clopidogrel was administered prior to the procedure to those not previously taking thienopyridines (from 1999 to august 2000 ticlopidine was used). At least one month of clopidogrel treatment (75 mg/d) was recommended for patients treated with a bare metal stent (BMS) and at least 3 months for patients treated with a drug eluting stent (DES). DES was not implanted routinely but could be used at the operators’ discretion after March 2003. All patients were advised to maintain the use of aspirin lifelong.
Follow-up and definitions
Clinical follow-up was scheduled for all patients after three months. Angiographic follow-up was scheduled between three and six months or earlier if non-invasive evaluation or clinical presentation suggested ischemia. All patients received a questionnaire between 9 and 12 month after the PCI with questions about any repeat PCI, CABG, MI, angina or any hospitalization. All data were registered prospectively in a database. Information about events was obtained by review of hospital records from Skejby Hospital, referring hospitals, and general practitioners. Telephone interview of patients and/or their general practitioners was done when needed. All deaths were considered to be of cardiac origin unless a non-cardiac origin was established clinically or at autopsy. Acute MI was diagnosed by symptoms and/or ECG changes and a rise in CK-MB >3 times normal value. Target lesion revascularization was defined as a repeated PCI intervention or CABG of the left coronary artery to treat a luminal stenosis within the stent or in the 5-mm distal or proximal segments adjacent to the stent, including the ostium of the left anterior descending artery and/or circumflex artery.
The primary outcome was the occurrence of major adverse cardiac events (MACE), defined as (1) cardiac death, (2) nonfatal MI, or (3) target lesion revascularization. The European system for cardiac operative risk evaluation (Euroscore)1 was used to estimate the risk of death at 30 days if the patient would have been treated with CABG.
Statistical analysis
Data were analyzed with Stata (Stata Corporation, USA). Continuous variables are expressed as mean±1 SD. Comparisons among the groups were made by one-way analysis of variance and chi-square tests. Significance was defined as a probability less than 0.05. Observation time and euroscore are expressed as median values with interquartile ranges. Rates of death, cardiac death, and MACE (with 95% confidence intervals) during the follow-up period were evaluated according to the Kaplan-Meier method.
Results
Baseline demographic and clinical data are presented in table 1.
The patients with low surgical risk were younger (60±14 years), and had a better left ventricular ejection fraction (EF) (55±15%). In contrast, the higher risk patients were older (76±9 years) and had lower EF (47±15%). Classification of patients as poor candidates for CABG (group 2) was done according to the following causes: Age ≥ 80 years (n=18), LM occlusion occurring during coronary angiography (n=2), LM dissection during LAD PCI (n=1), CX and LAD not graftable (n=3), lack of graft material (n=4), significant cerebrovascular disease (n=2), refusal to receive blood transfusion (n=2), severe obesity (n=1), high dose prednisolone treatment (n=1), severe aortic calcification (n=4), impaired pulmonary function (FEV1 < 1 litre) (n=4), cardiogenic shock without AMI (n=2), cancer (n=4), VT and age 79 years (n=1), multiple risk factors (diabetes, claudicatio intermittens, and reduced ejection fraction) (n=1). The median value for the Euroscore (interquartile range) was 2% (1-5), 8% (5-16), and 18% (7-31), in the three groups respectively.
Angiographic and procedural data are presented in table 2.
Left main stenosis with involvement of the bifurcation was less frequent in the patients with low surgical risk. Thrombus material was mainly seen in patients with AMI. Stents were placed in all low risk patients, in 48 of 50 in the higher risk group and in 26 of the 27 AMI patients.
Overall, thirty-one patients died during the observation period. Only one patient with low surgical risk died; a non-cardiac death due to disseminated cancer. Seventeen among the 50 patients considered poor CABG candidates died, and the cause was cardiac in 12 patients. Thirteen of the 27 AMI patients died. Twelve were cardiac deaths and seven of these were due to pump failure in the catheterization room.
Ten patients had a target lesion revascularization, and the cause was instent restenosis in five patients. Two patients were treated with CABG, and three patients were treated with a repeat PCI (one with brachytheraphy). Only one instent restenosis was observed among the patients that were treated with DES. The patient was initially treated with culotte stenting, and the restenosis was focal in both the ostium of the CX and the LAD. The patient was successfully treated with kissing balloon inflation. One patient had a verified stent thrombosis.
Figure 1 and 2 show the Kaplan-Meier curves for cardiac death and MACE, respectively.
Fig. 1. Probability of cardiac death (%) during follow-up period in patients with low surgical risk (N=27), poor CABG candidates (N=50), and AMI patients (N=27).
Fig. 2. Probability of major cardiac event (%): cardiac death, nonfatal AMI or target lesion revascularization during follow-up period in patients with low surgical risk (N=27), poor CABG candidates (N=50), and AMI patients (N=27).
Median observation time with interquartile range for death and cardiac death were 239 (177-647), 233 (94-355), and 227 (0-357) days for the patients with low surgical risk, the poor CABG candidates and the AMI patients, respectively. The corresponding figures for observation time to MACE were 237 (138-647), 208 (94-349), and 227 (0-320) days, respectively. The figures for the estimated events rates at thirty days and six month with 95% confidence intervals are shown in table 3 and table 4.
Among group 1 and 2 patients, 35 were treated with a BMS and 42 were treated with a DES. Patients receiving a BMS and DES differed according to time of treatment: only 6 of the 35 BMS treated patients were treated after March 2003 while all in the DES group were treated after March 2003. There was no statistical difference in age, proportion of males, proportion of patients with high surgical risk, and left ventricular ejection fraction between BMS and DES treated patients. In the group 1 and 2 patients we did not observe any significant difference in MACE rate between patients receiving a DES compared to patients receiving a BMS. MACE at 6 months in group 1 and 2 was 21% for BMS and 19% for DES (p=0.2). DES was not used routinely in AMI patients.
Discussion
Our major findings are that PCI of selected LM lesions can be performed with: (1) low event rates in patients with low surgical risk: (2) with acceptable event rates in inoperable or surgically high risk patients. In contrast PCI for severe left main stenosis or occlusion during AMI was associated with high acute mortality rate. Thus, the outcome of LM PCI is highly dependent on the clinical situation and on patient selection.
Previous reports
Several small studies have reported the outcome of LM PCI in different groups of patients, but different patient selection criteria make the results difficult to compare2-6. The largest registry, the ULTIMA registry reported outcome in 279 patients2. In low risk patients no peri-procedural deaths were observed and the 1 year mortality was only 3.4%. In patients considered at intermediate risk the 1 year mortality was 24%. In patients, who were considered at high surgical risk the 1 year mortality was above 56%. Forty patients underwent emergency LM-PCI due to AMI. In these patients the in-hospital mortality was as high as 55%7. These observations are in agreement with our mortality rates.
Silvestri et al.3 also stratified their patients into good and poor CABG candidates and found 30 day MACE rate of 0% and 13%, respectively. Park et al.5 have reported results in low risk patients with mean age at 59 years and a preserved LV function (> 40%). At six month the MACE rate was 6% in patients treated with bare metal stents and 2% in patients treated with drug eluting stents. Our MACE rates correspond very well to their observations.
Comparison with surgery
In the patients with low surgical risk we observed one major coronary event but no cardiac deaths during the first 6 months, corresponding to a 30 day mortality of 0%. The estimated 30 day mortality was 2% in these patients if CABG had been performed instead. The 30 day cardiac death rate in the poor CABG candidates was 14%; somewhat above the Euroscore estimated mortality of 8%. However, many of the poor CABG candidates had contraindications to surgery and therefore a cardiac death rate of 14% may be acceptable in patients with severe symptoms.
We observed high thirty-day mortality (37%) in AMI patients. The Euroscore estimated the 30-day mortality to 18% indicating that CABG also is high risk procedure in acute MI. The high mortality rate suggests that acute or subacute CABG should be considered as an alternative to PCI in the setting of MI with culprit lesion of the LM. However, some of our procedures were bail-out procedures in patients with cardiogenic shock and fading life functions impossible to bridge to CABG.
DES vs BMS
Chieffo et al.6 have recently reported their results of elective LM PCI. In patients treated with bare metal stents a MACE rate at 6 months was 35.9% versus 20.0% in DES treated patients (p=0.04). The corresponding figures for MACE at 6 months in our elective LM PCI (group 1 and 2) was 21% for BMS and 19% for DES (p=ns). The RESEARCH and T-SEARCH registry found 6 month MACE at 35% for BMS and 15% for DES reaching statistical significance8. Restenosis is a problem in LM PCI, and accounts for a substantial proportion of MACE. The use of DES may reduce the rate of restenosis also in LM PCI, and in case of restenosis the neointima formation may be more focal8. Because of the risk of restenosis, despite the use of DES, angiographic follow-up is recommended routinely in LM PCI.
Stent thrombosis
Stent thrombosis is a major concern in LM PCI where the event may be fatal. We observed one stent thrombosis (in a patient with low surgical risk), which occurred 8 days after the initial IVUS guided LM PCI. The patient was treated with both aspirin and clopidogrel, but did not receive GPIIb/IIIa inhibitor during PCI. The patient presented with an ST segment elevation MI and thrombosis of the stent in the proximal part of the LAD. This patient was successfully treated with balloon angioplasty. Stent thrombosis as a cause of death in some of the poor CABG candidates cannot be excluded. One patient died after 13 days due to a ST elevation AMI and 3 patients died suddenly. One AMI patient died of reinfarction after 3 days. Stent thrombosis is a major concern in LM PCI. IVUS guidance of stent sizing/expansion and lifelong clopidogrel treatment may reduce this risk.
Study limitations
This series of patients represents a selected group of patients. All LM lesions had suitable anatomy for stenting (group 1 and 2) and the operator had a preference for PCI. The procedures were performed over long period of time (5 years). In this period operator experience increased and the use of drug eluting stents was introduced. Grouping the patients into three cohorts makes the sample sizes smaller and the estimated event rates have wide confidence intervals. However, the data clearly demonstrates that the patient selection significantly influence the result. In future follow-up studies we suggest that patients are grouped into surgical low risk patients, poor CABG candidates, and AMI patients based on objective comparable criteria including angiographic criteria.
Conclusion
We conclude that LM PCI can be safely performed in carefully selected patients. Routine introduction of the treatment, however, must await results of large randomized studies between PCI and CABG preferably with long term follow-up. We suggest that LM interventions are grouped according to surgical low risk, surgical high risk and AMI.

