Abstract
Background: ARTS-II was designed to evaluate the sirolimus-eluting stent (SES) versus ARTS-I. The objective of this analysis is to assess the safety and efficacy of the SES in diabetic patients with multivessel disease (MVD) versus both arms of ARTS-I.
Methods and results: The ARTS studies included 367 diabetic patients (ARTS-II: 159; ARTS-I-CABG: 96; ARTS-I-PCI: 112). Baseline characteristics showed a more diseased patient population in the ARTS-II study: 50.3% with 3VD vs. 35.4% (ARTS-I-CABG) and 30.8% (ARTS-I-PCI) (p=0.003). Treated or anastomosed lesions were 3.2±1.2 (ARTS-II), 2.8±0.8 (ARTS-I-CABG) and 2.5±1.1 (ARTS-I-PCI). At 30 days there was a significant difference in MACCE between ARTS-II (4.4%) and ARTS-I-PCI (12.5%) (p=0.02). At 1-year, the death rate was 2.5% (ARTS-II) vs. 3.1% (ARTS-I-CABG) and 6.3% (ARTS-I-PCI) without significant differences. Myocardial infarction rate was 0.6% (ARTS-II) vs. 2.1% (ARTS-I-CABG; p=0.56) and 6.3% (ARTS-I-PCI; p=0.01). The need for repeat revascularization was 12.6% (ARTS-II) vs. 4.2% (ARTS-I-CABG; p=0.027) and 22.3% (ARTS-I-PCI; p= 0.046). MACCE-free survival was 84.3% (ARTS-II) vs. 85.4% (ARTS-I-CABG; p=0.86) and 63.4% (ARTS-I-PCI; p<0.001). Also at 1 year, the overall MACCE rate in patients with diabetes was significantly higher than in nondiabetic patients, 15.7% vs. 8.5%, respectively [RR 1.85, 95%CI (1.16,2.97), p=0.015), due to a higher incidence of death and need for repeat revascularization, 2.5% vs. 0.4 and 12.5% vs. 5.6% in diabetes vs. nondiabetes groups, respectively.
Conclusion: Despite more extensive and treated disease, the overall MACCE-free survival in diabetic patients at 1 year in ARTS-II is similar to ARTS-I-CABG.
Introduction
Patients with diabetes mellitus have a greater incidence of atherosclerotic disease associated with a worse prognosis. The absolute risk of cardiac death is three times higher compared to nondiabetic patients1,2. In addition, diabetic patients undergoing coronary artery revascularization, have a worse outcome than nondiabetic patients3. Subgroup analysis of the Bypass Angioplasty Revascularization Investigation (BARI)4 and Emory Angioplasty versus Surgery Trial (EAST)5, both randomized studies, demonstrated that diabetic patients with multivessel coronary disease (MVD) had worse long-term outcome when treated with balloon angioplasty than with CABG. Specifically, in the BARI study patients receiving at least one internal mammary artery graft had less cardiac mortality (5.8% versus 20.6%, P=.0003), than patients treated with balloon angioplasty.
In the bare-metal stent era, multiple stenting in diabetic patients resulted in a higher incidence of in-hospital CABG, a higher need for repeat revascularization during follow-up and a lower one-year survival rate than in nondiabetic patients6. The Arterial Revascularization Therapy Study (ARTS-I) compared multivessel coronary artery stenting with CABG surgery7. In the subgroup of diabetic patients there was no statistically significant difference in mortality at 1 and at 3 years between the 2 groups8; however diabetic patients who underwent PCI required more repeat revascularization procedures8. Moreover at 5 years9, in patients with diabetes, those who underwent stenting had a mortality rate of 13.4%, versus 8.3% in those who underwent CABG (p = 0.27; RR, 1.61; 95% CI, 0.71 to 3.63). Within the stent group, diabetic patients had a significantly higher mortality rate than non-diabetic patients (13.4% vs. 6.8%; p=0.03; RR, 1.98; 95% CI, 1.11 to 3.52). There was no significant mortality difference between the diabetic and non-diabetic patients within the CABG group (8.3% vs. 7.5%; p=0.8; RR, 1.12; 95% CI, 0.54 to 2.32).
Diabetic patients treated with bare-metal stent also had a lower event-free survival at five years than non-diabetic patients. The MACCE rate at five years in diabetic patients treated with stents was 54.5%, versus 38.7% in non-diabetics (p=0.003). Conversely, there was no significant difference in the five-year MACCE rate between diabetic and non-diabetic patients treated with CABG (25.0% vs. 21.2%, p=0.42). The difference in MACCE rate between diabetic and non-diabetic patients treated with stenting is predominantly attributable to the higher rate of repeat revascularization in diabetic patients (42.9% vs. 27.5%, p=0.002).
Sirolimus-eluting stents (SES) have been shown to significantly reduce restenosis and, consequently reduce the need for repeat coronary revascularization in randomized trials10-12. The potential of SES for the treatment of multivessel disease in diabetics is unknown. The Arterial Revascularization Therapy Study II (ARTS-II) was designed to evaluate the SES versus ARTS-I13,14. The objective of this analysis is to assess the safety and efficacy of the SES in diabetic patients with MVD versus both arms of ARTS-I.
Methods
ARTS-II STUDY DESIGN
This multicentre, non-randomized, stratified, non-inferiority study was designed to evaluate sirolimus-eluting stent (SES) implantation in patients with multivessel disease using the surgical group of ARTS-I as an historical control. ARTS-I enrolled patients between April 1997 and June 1998. Both studies ARTS-I and ARTS-II used the same inclusion/exclusion criteria.13
Patients with stable or unstable angina, or silent ischemia were enrolled. The left anterior descending (LAD) artery and at least another significant lesion (>50% diameter stenosis) in a different major epicardial coronary artery had to be treated. Stents with a diameter of 2.5 to 3.5 mm and length up to 33 mm were used. Patients with any prior coronary intervention, left main coronary disease, overt congestive heart failure or a left ventricular ejection fraction of less than 30% were excluded. Additional exclusion criteria included: history of a cerebrovascular accident, transmural myocardial infarction in the preceding week, severe hepatic or renal disease, neutropenia or thrombocytopenia, intolerance or contraindication to acetylsalicylic acid or thienopyridines, need for concomitant major surgery, and life-limiting major non-cardiac diseases. The study was approved by the ethical committees of each participation institution. All patients signed informed consent prior to study entry.
Study population
All patients enrolled in the ARTS-I trial and ARTS-II were included in the present analysis. Patients were divided into 2 groups: diabetes (367) and non-diabetes (1445).
Study objectives
The primary objective of this analysis is to evaluate the diabetic patients in ARTS-II to both arms of ARTS-I with respect to MACCE at 1-year; the secondary objective is to assess 1-year outcomes between diabetic and nondiabetic in ARTS-II.
End point definitions
Death from all causes were reported, and categorised as cardiac unless there was documentation to the contrary. Cerebrovascular events (CVA) included: stroke, transient ischaemic attacks, and reversible ischaemic neurologic deficits. Within 7 days after the intervention, a diagnosis of myocardial infarction was made if new abnormal Q-waves (according to the Minnesota code) and either a ratio of serum creatine kinase MB (CK-MB) isoenzyme to total cardiac enzyme that was greater than 0.1 or a CK-MB value that was 5 times the upper limit of normal were present. Serum creatine kinase levels were measured 6 and 12 hours after the intervention and before discharge. Beginning 8 days after the intervention, either abnormal Q-waves or enzymatic changes were sufficient for a diagnosis of myocardial infarction. This two-part method of defining myocardial infarction was developed for ARTS-I to address the difficulty of diagnosing a myocardial infarction after surgery. A myocardial infarction was confirmed only after the relevant electrocardiograms had been analysed by the electrocardiographic core laboratory and adjudicated by an independent clinical event committee. All repeat revascularization procedures were recorded. Events were counted from the time of the start of the initial procedure.
Statistical analysis
Demographic and procedural characteristics of diabetic patients were compared between ARTS-II and ARTS-I (CABG and PCI). Similar comparison was performed for nondiabetic patients. Continuous variables are expressed as mean±standard deviation. Categorical variables are presented as percentages. The F-test from an analysis of variance for continuous variables and the Fisher’s exact test for categorical variables were used.
A separate multivariate regression analysis was performed to determine independent predictors of MACCE within the ARTS-II population only. Clinically important baseline and procedural characteristics were tested on a per patient basis by univariate analysis to determine suitability for inclusion in the multivariate model. These variables were then entered into a stepwise logistic regression model with entry and stay criteria of 0.20 and 0.05 respectively.
MACCE at 30 days and 1 year are presented as counts and percentages and were compared in terms of relative risks (ARTS-II vs. both ARTS-I arms) with 95% confidence intervals. Time-to-event variables are presented as Kaplan-Meier curves, and the overall incidence was tested using the log-rank test. An adjustment for the differences in the baseline characteristics between ARTS-I and ARTS-II populations was performed by univariate frailty analysis on the MACCE, using a Weibull distribution. The covariates in the model, which considered ARTS-I-CABG and ARTS-II populations, were age, hypercholesterolemia, hypertension, previous MI, family history of MI, no. of lesions type B2/C and three vessel disease. In the model, that compared the differences with ARTS-I-PCI, the same variables were included plus maximum inflation pressure and total stented length.
Results
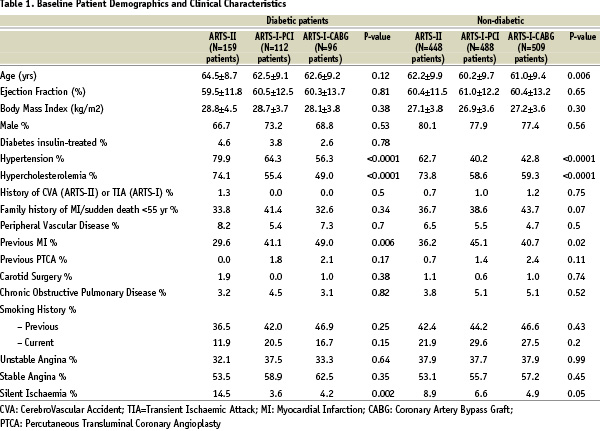
Between February 2003 and November 2003, 607 patients, of whom 159 diabetic patients, were treated at 45 participating centres in the ARTS-II study. Table 1 and 2 present the baseline demographic and angiographic characteristics of the 3 treatment groups in diabetic and nondiabetic patients.
Baseline characteristics
DIABETIC PATIENTS IN ARTS-I AND ARTS-II
ARTS-II had a significantly higher percentage of patients with hypertension: 79.9% (ARTS-II) vs. 56.3% (ARTS-I-CABG) and 64.3% (ARTS-I-PCI), p <0.0001. Also hypercholesterolemia increased from 49.0% (ARTS-I-CABG) and 55.4% (ARTS-I-PCI) to 74.1% in the ARTS-II study, p <0.0001. Among the diabetic patients, 28 (17.6%) (ARTS-II), 16 (16.7%) (ARTS-I-CABG) and 23 (20.5%) (ARTS-I-PCI) required insulin treatment. The percentage of three vessel disease was 50.3% in ARTS-II vs. 35.4% in ARTS-I-CABG and 30.8% in ARTS-I-PCI, p=0.003. The mean number of significant lesions per patient was 3.2±1.2 in ARTS-II versus 2.5±1.1 in ARTS-I-PCI, p <0.0001. ARTS-II patients received 3.6±1.5 stents with an average total stent length of 73.9±31.9 mm vs. 3.0±1.5 and 52.7±25.6 mm in ARTS-I-PCI, both with p=0.002 and p <0.0001, respectively.
The mean duration of the procedure was 83 minutes in ARTS-II versus 201 minutes in ARTS-I-CABG and 104 minutes in ARTS-I-PCI (Table 2).
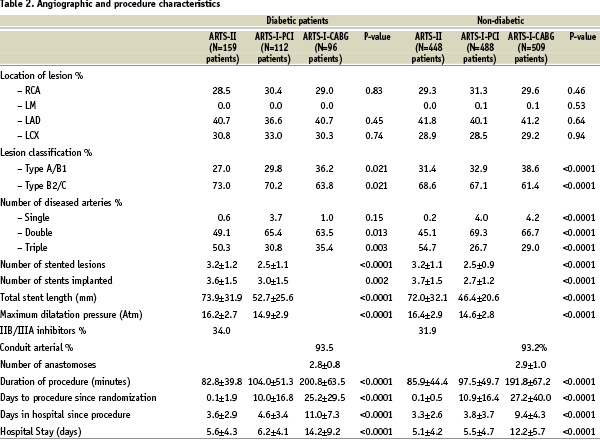
Post-procedurally, patients were hospitalized for 3.6±2.9 days after ARTS-II versus 11.0±7.3 days after ARTS-I-CABG and 4.6±3.4 days in ARTS-I-PCI.
DIABETIC VERSUS NON-DIABETIC PATIENTS IN ARTS-II
There were fewer male patients in the diabetic subgroup. Diabetic patients had a significantly higher percentage of hypertension and silent ischaemia. The use of glycoprotein IIb/IIIa inhibitors was similar between the two subgroups.
Short-term clinical outcome in diabetic patients
Up to 30 days, ARTS-II diabetics had a similar incidence of MACCE compared to ARTS-I-CABG (4.4% vs. 7.3%, p=0.40) and a lower incidence compared to ARTS-I-PCI (12.5%, p=0.02). Three CVAs were reported, all occurring in the ARTS-I-CABG arm. (Table 3)
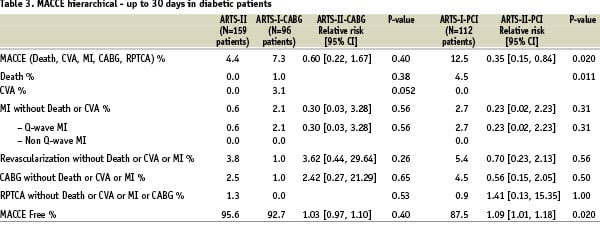
There were 2 angiographically documented sub-acute thromboses in ARTS-II (1.3%) and 2 in the ARTS-I-PCI (1.8%). All events occurred before the patients were discharged.
One-year clinical outcome in diabetic patients
Patients showed a similar incidence of MACCE in ARTS-II and ARTS-I-CABG (Table 4) (Figure 1).
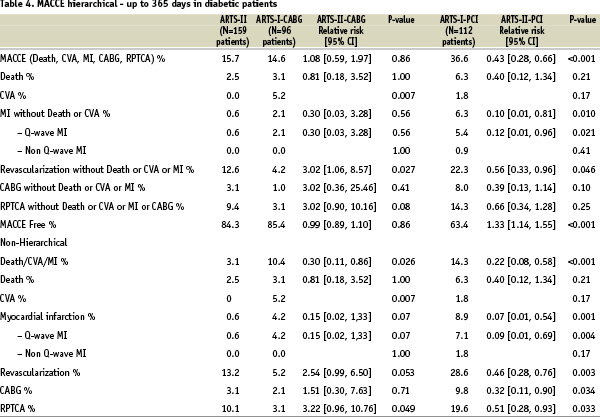
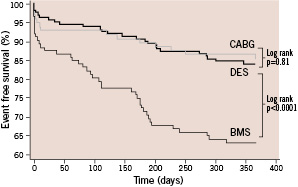
Figure 1. Kaplan-Meier curves out to 1 year in diabetic patients in ARTS-I and ARTS-II population. CABG, coronary artery bypass graft; DES, drug-eluting stent; BMS, bare metal stent.
However, patients assigned to ARTS-I-CABG had a higher incidence of cerebrovascular events than patients in ARTS-II, 0% vs. 5.2% respectively, p=0.007. Conversely, the need for repeat revascularization was higher in ARTS-II that in ARTS-I-CABG, 12.6% vs. 4.2%, respectively [RR 3.02, 95%CI (1.06,8.57), p=0.027]. As expected, ARTS-II patients had a lower incidence of MACCE than patients in ARTS-I-PCI group, 15.7% vs. 36.6% respectively [RR 0.43, 95% CI (0.28,0.66), p<0.001], mainly due to the decreased need for repeat revascularization, 12.6% in ARTS-II vs. 22.3% in ARTS-I-PCI respectively, [RR 0.56, 95%CI (0.33,0.95), p=0.046]. There was also lower incidence of myocardial infarction in ARTS-II than in ARTS-I-PCI, 0.6 vs. 6.3% respectively [RR 0.10, 95%CI (0.01,0.81), p=0.010). One late thrombosis was recorded in an insulin-treated diabetic patient in ARTS-II.
One-year clinical outcome in ARTS-II
(diabetes vs. nondiabetes)
The overall MACCE rate in patients with diabetes was significantly higher than in nondiabetic patients, 15.7% vs. 8.5%, respectively [RR 1.85, 95%CI (1.16,2.97), p=0.015), due to a higher incidence of death and need for repeat revascularization, 2.5% vs. 0.4 and 12.5% vs. 5.6% in diabetes vs. nondiabetes groups, respectively. (Table 5 and Figure 2).
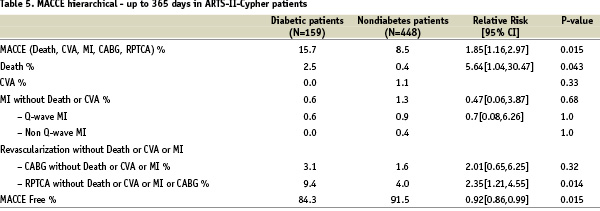
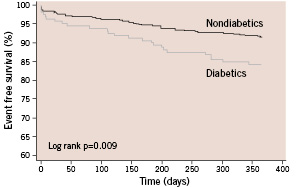
Figure 2. Kaplan-Meier curves out to 1 year diabetic vs. nondiabetes patients in ARTS-II: Freedom from Major Adverse Cardiac and Cerebral Events (MACCE)
Univariate and multivariate predictors of late clinical outcome
Independent risk factors for late clinical outcome (MACCE) in the ARTS-II population are displayed in Table 6 and 7.
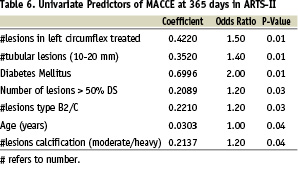
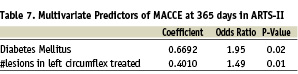
Diabetes was a risk factor for the occurrence of MACCE, (Odds Ratio 1.95, p=0.02).
Discussion
The main findings of this analysis are: (1) MACCE-free survival in diabetic patients at 1 year in ARTS-II is similar to ARTS-I-CABG (84.3% vs. 85.4%); (2) the MACCE-free survival compared to ARTS-I-PCI is higher (84.3% vs. 63.4%) primarily driven by a lower need for revascularization; (3) there was a significantly lower incidence of MACCE at 30 days in ARTS-II than in ARTS-I-PCI; (4) the presence of diabetes continues to be the most important predictor of MACCE at 1 year follow up.
Improvement in early outcomes
Despite more extensive and complex coronary artery disease with more vessels treated in diabetic patients enrolled in ARTS-II, in-hospital clinical outcomes were better than in ARTS-I-PCI patients, and similar to the ARTS-I-CABG group. The rates of in-hospital MACCE were 3.1%, 9.8%, and 7.3%, respectively. Interestingly, sub-acute stent thrombosis (<30 days) in ARTS-II was observed in only 2/159 diabetic patients; whereas one late thrombosis was recorded in an insulin-treated diabetic patient in ARTS-II despite a high number of stented lesions (3.2±1.2) and a longer total stented length (73.9±31.9 mm). The use of glycoprotein IIb/IIIa inhibitors15,16, compulsive pre-treatment with clopidogrel16,17, a more deliverable stent and increased operator experience may all have contributed to this low incidence of early/late adverse events.
Antirestenotic effect of SES
The remarkable antirestenotic effect of the sirolimus-eluting stent demonstrated in several randomized trials-10-12,19,20, has been recently confirmed in diabetic patients21,22. The result of the ARTS-II diabetic subset is in line with these results. In comparison with ARTS-I, there was a higher incidence of three-vessel disease (50%), diffuse lesions, and type C lesions in the ARTS-II group. Despite this substantially higher risk profile, the need for repeat revascularization was reduced from 22.3% in ARTS-I-PCI arm to 12.6% in ARTS-II. Interestingly, but not surprisingly, ARTS-I-CABG still has the lowest need for revascularization (4.2%). Indeed, in the ARTS-II study, the presence of diabetes was the strongest predictor of MACCE events (80% of these were revascularizations) during follow up.
Comparison with CABG
Despite the persistent advantage of CABG in terms of a lower need for revascularization compared to ARTS-II, it is interesting to note that CABG carried a higher risk for CVA, a finding already reported in the diabetic subset of ARTS-I23. Overall, at 1 year, the ARTS-II diabetic group had a very similar MACCE rate to that seen in the ARTS-I-CABG group. It is possible that progress in surgical techniques, such as a greater use of off-pump surgery, may further improve the surgical results and reduce the risk of cerebral complications.
Comparison with nondiabetics
In ARTS-II, the diabetic patients continued to have a worse outcome compared to non-diabetics, but the difference was smaller than in ARTS-I, although still significant.
Diabetes mellitus remains an independent predictor of MACCE at one year follow up and is associated with a higher incidence of death and TVR, even with SES usage. Spot treatment provided by drug-eluting coronary stents on critical lesions cannot prevent the consequences of further atherosclerosis progression and avoid co-morbidities associated with this systemic disease.
Limitations
This study is a sub-analysis of the main ARTS-I and ARTS-II trials – albeit prespecified – and hence suffers from inherent limitations, such as the lack of sufficient power because of the limited number of patients in the subgroups to provide definite answers. While the protocol required that the lesions in ARTS-II be potentially treatable by CABG, the absence of dialogue with the surgeons prior to the intervention may have caused a selection bias. Another potential bias of this study is that a five-year time difference exists between the groups that were being compared, and technology and medical practice have improved with time, as have surgical mortality rates24,25. The study is non-randomized and consequently statistical adjustment is required to correct for the differences between the current study population and the historical ARTS-I population.
However, the results of the study after adjustment for differences in risk factors did not substantially differ from the unadjusted outcome, since the patients enrolled in ARTS-II were in fact more complex in terms of demographics and lesion characteristics than those included in ARTS-I. The results of this study pertain only to 1-year follow-up and the 5-year follow-up of the diabetic patients in ARTS-I has clearly indicated an increasing difference in outcome between the surgical and percutaneously treated cohorts of patients. Whether efficacy of the percutaneous treatment using SES versus CABG in diabetic patients with multivessel disease will be maintained over a longer time period remains to be seen.
Conclusion
When compared to the outcome of the diabetic patients with multivessel disease treated with either PCI or CABG in ARTS-I, the overall MACCE-free survival rate at 1 year in ARTS-II is similar to ARTS-I-CABG and more favourable than ARTS-I-PCI.
Even when treated with drug-eluting stents, diabetes remains an important predictive risk factor for adverse clinical outcome in patients with multivessel disease.
Acknowledgement
The co-authors would like to express their gratitude to Brian G. Firth MD PhD in the drafting of the manuscript.
This study was supported by Cordis, a Johnson & Johnson company.