Abstract
Background: Percutaneous transcatheter occlusion with ethanol injection of septal arteries is an efficient treatment procedure of hypertrophic obstructive cardiomyopathy (HOCM). The aim of our study is to evaluate the feasibility and efficiency of septal artery embolization with microcoils.
Methods: The microcoils were delivered through the guide-wire lumen of a 2mm-diameter coaxial balloon positioned inside the target vessel as distally as possible. One or more 0.018”-straight microcoils (Hilal straight coils, Cook, USA) were used for each target vessel until complete flow obstruction was noted. The intraventricular pressure gradient was measured before, during and after the procedure. Septal branch occlusion was finally documented by coronary angiography.
Results: We treated 7 patients (pts) (male: 5 pts; mean age: 48 (10 years). All patients were symptomatic (NYHA class 3 or 4). The target vessels were successfully occluded in all patients, without complications. Moderate pain was recorded during and after the procedure and the CK level increased five- to ten-fold. The pressure gradient diminished during the procedure from 72 ± 21 mm Hg to 30 ± 15 mm Hg. The number of coils delivered ranged from 3 to 7 / patient. The embolized septal branches: 1 vessel in 5 patients; 2 vessels in 1 patient; 3 vessels in 1 case. After the procedure the pressure gradient, evaluated by transthoracic echocardiography, was 34 ± 16 mm Hg and 42 ± 12 mm Hg at 3 month-follow-up. Clinical improvement was recorded in all patients after the procedure (NYHA class 1 or 2). Temporary pacing was necessary in 3 patients during and immediately after the procedure but no patient needed permanent pacing.
Conclusions: Microcoil embolization is an efficient and safe approach for transcatheter ablation of septal hypertrophy in HOCM. This technique induced myocardial necrosis without the toxic effects of alcohol, reducing the risk of complications (permanent pace-maker implantation, ethanol flow to other myocardial regions).
Introduction
Approximately 25-30% of patients with familial hypertrophic cardiomyopathy suffer from left ventricular outflow tract obstruction: hypertrophic obstructive cardiomyopathy (HOCM). Patients (pts) with HOCM may demonstrate symptoms due to the outflow obstruction produced by hyperdynamic left ventricular contraction.
Numerous treatment options for HOCM have been suggested for patients who have severe symptoms of heart failure.
Medical therapy that reduces myocardial contractility, such as beta-adrenergic blockers, calcium channel blockers and other negative inotropic agents has demonstrated symptomatic benefit. When medical therapy fails, mechanically altering the sequence or degree of left ventricular contraction by DDD pacing or surgically reducing the hypertrophied muscle segment in the outflow tract have been described.
In 1995, Sigwart first reported selective septal ablation with ethanol for the treatment of HOCM1. Initial results showed symptom relief in the majority of patients and low short-term mortality. Patients undergoing alcohol septal ablation exhibited rapid recovery from the procedure and continued symptomatic improvement over time.
The aim of our study is to evaluate the feasibility, safety and efficiency of septal artery embolization with a modified technique in which microcoils are used to induce a controlled septal myocardial infarction, instead of alcohol injection.
Methods and material
Seven patients (pts) (mean age: 48 ± 10 years; men: 5 pts) with symptomatic HOCM verified clinically and by trans-thoracic echocardiography with mean disease duration of 4 years (range 2-7 years) were selected for this procedure. The echocardiographic and Doppler parameters included the following: left ventricular outflow tract (LVOT) gradient; end-diastolic thickness of the left ventricular posterior wall (LVPW); end-diastolic dimension of the left ventricular inter-ventricular septum (IVS); systolic anterior movement (SAM). The SAM phenomenon was classified from grade 0 (no SAM) to grade III (holosystolic septal contact). The inclusion criteria were: age > 20 years; SAM grade III; NYHA class III or IV; LVOT gradient > 50 mm Hg in sinus rhythm. Patients with LVOT gradient < 50 mm Hg in sinus rhythm, NYHA class < III and non-obstructive hypertrophic cardiomiopathy were excluded. The risks and possible complications of the intended procedure were explained to the patients and informed consent was obtained. The protocol of the technique was approved by the locally appointed ethics committee.
Technique
Diagnostic right and left heart catheterizations and coronary angiography were first carried out. The femoral arteries on both sides and the femoral vein were canulated in each patient.
An 8 French Judkins left guiding catheter introduced through the right femoral artery was positioned at the ostium of the left coronary artery. A 5 French pig tail catheter was positioned in the LV distally to the obstruction in order to evaluate the intra-ventricular pressure gradient. A temporary pacemaker lead was placed in the RV of all patients.
The initial LVOT pressure gradient was measured during sinus rhythm (figure 1) and post-extrasystolic. A septal artery was considered the target vessel (usually a first major septal branch- figure 2) if the pressure gradient dropped significantly (at least 50%) after inflating the over-the-wire balloon inside the artery for 5 minutes. If the first septal artery was not the target vessel, sequential pressure gradient measurements were repeated with the inflated balloon positioned in the next septal arteries. In 4 patients, simultaneous LV angiogram and septal artery angiogram through the coaxial balloon catheter were performed to confirm that the hypertrophied septum is supplied by the selected septal artery.
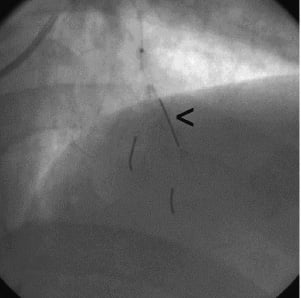
Fig. 1: A 37-year old male, known with HOCM, was admitted for persistent dyspnea on minimal exertion. The initial resting LVOT systolic gradient was 55 mm Hg (the pressure gradient is recorded during catheter withdrawal from the apex to the LV outflow tract).
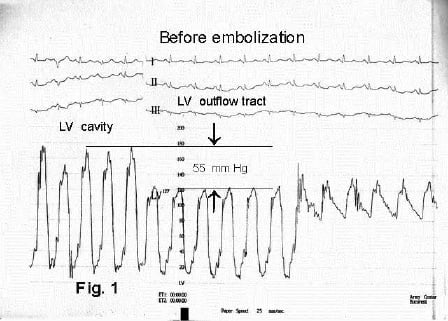
Fig. 2: The coronary angiography showed an important 1st septal artery (arrow). Balloon inflation inside the vessel induced intraventricular pressure gradient reduction by more than 50%.
The microcoils were delivered through the guide-wire lumen of a 2 mm or 2.5 mm diameter over-the-wire balloon positioned inside the target vessel as distally as possible (figure 3). One or more 0.018”-straight microcoils (Hilal straight coils, Cook, USA) were used for each target vessel until complete flow obstruction was noted (figure 4). The resting gradient and on stress intra-ventricular pressure gradient was measured after the procedure (figure 5). Septal branch occlusion was finally documented by coronary angiography (figure 6).

Fig. 3: An over-the-wire 2.0 mm balloon was positioned into the distal septal artery (arrow) and inflated at 6 atmospheres. The guidewire lumen was used to deliver the microcoils.
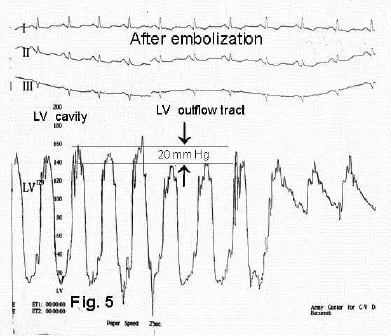
Fig. 4: Four Hilal straight microcoils (5mm/0.018” and 10mm/0.018”) were deployed in different branches of the 1st septal artery.
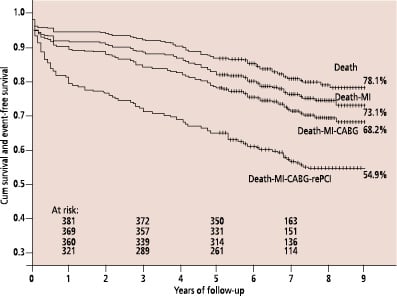
Fig. 5: The resting LVOT pressure gradient dropped to 20 mm Hg after septal embolization (arrows).
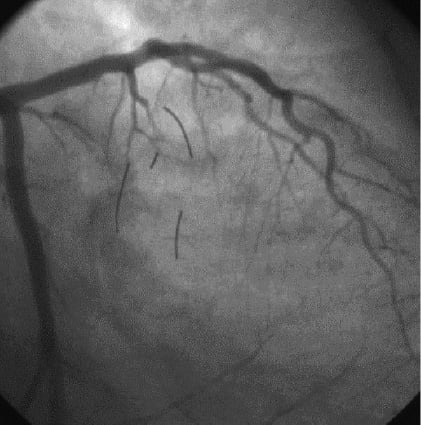
Fig. 6: The final angiogram revealed complete occlusion of the 1st septal artery.
Results
All patients were severely symptomatic (NYHA class III: 5 pts; NYHA class IV: 2 pts) despite aggressive medical therapy. All patients were on medical therapy with calcium-channel blockers and beta-blockers; 3 patients had amiodarone associated in their medication. The electrocardiograms showed pronounced LV hypertrophy with strain in all patients; one patient was in atrial fibrillation. The echocardiograms revealed significant hypertrophy of the basal septum (average thickness: 22 mm; range: 19-27 mm). The systolic anterior movement (SAM) phenomenon of the anterior mitral leaflet was grade III (prolonged systolic contact with the interventricular septum) in 100% of patients. The mean resting LVOT gradient, measured by Doppler examination, was 76 ± 15 mm Hg. Positive family history was present in 3 patients. None had undergone surgical myectomy or DDD pacemaker implantation.
The number of coils delivered ranged from 3 to 7 per patient. The embolized septal branches included: 1 vessel in 5 patients; 2 vessels in 2 patients. The target vessels were successfully occluded in all patients, without complications. The resting LVOT pressure gradient diminished during the procedure from 72 ± 21 mm Hg to 30 ± 15 mm Hg. The initial post-extrasystolic pressure gradient was 105 ± 22 mm Hg and decreased to 64 ± 15 mm Hg after embolization. Moderate pain was recorded during and after the procedure and the CK level increased five- to ten-fold. After the procedure the mean LVOT pressure gradient, evaluated by transthoracic echocardiography, was 34 ± 16 mm Hg. Clinical improvement was recorded in all patients after the procedure (NYHA class I: 2 pts; class II: 5 pts). Temporary pacing was necessary in 4 patients during and immediately after the procedure but no patient needed permanent pacing. At 3-month follow-up no cardiac death was recorded; the mean septal thickness was 18 mm and the average LVOT 42 ± 12 mm Hg at Doppler examination (6 patients); one patient was lost from the follow-up.
Discussion
The mechanism of intraventricular pressure gradient in hypertrophic cardiomyopathy suggests that several therapeutic approaches may provide symptomatic relief. These methods include negative inotropic pharmacologic therapy, argon laser myoplasty, DDD pacing, surgical septal myomectomy (sometimes combined with mitral valve replacement) and percutaneous septal ablation (using the septal artery route or direct intracavitary ablation with radiofrequency).
The induced septal infarction of the subaortic segment of the interventricular septum using alcohol instillation, has been demonstrated to be a hemodynamically effective method of reducing left ventricular outflow tract obstruction2. Clinical and hemodynamic improvements have been demonstrated at short- and medium-term follow-up3 equivalent to surgical myectomy4.
Several concerns have been raised regarding complications related to alcohol septal ablation:
- the procedure may result in a possible increased incidence of bradyarrhythmias (necessitating permanent pacing) or tachyarrhythmias5;
- alcohol leakage down the main lumen of the left anterior descending artery may cause transient impairment of flow and large cardiac enzyme release2;
- alcohol flow through septal artery connections to other coronary branches may induce myocardial infarction of other territories;
- ventricular septal rupture6;
- progressive septal fibrosis, impaired ventricular function and thinning of the walls, may predispose the patient to progressive heart failure7;
Many of these already reported or potential complications associated with alcohol instillation may induce cardiac death8.
Other percutaneous techniques of septal hypertrophy reduction have been described. Pericardium-covered stent9 and PTFE-covered stents implantated on LAD10 were reported to be efficient in reducing the LVOT pressure gradient by sealing the origins of the septal arteries; in one reported case11 medium-term results showed return of the gradient and symptoms after a few months; this was probably due to collateral circulation and the authors postulated that the initial success was related to myocardial ischemia rather than necrosis. Another study reported the persistence of the clinical and echocardiographical benefits at 3-month follow-up after covered stents were implanted in 5 pts12.
Another technique consists of septal embolization with particles of Ivalon (polyvinyl alcohol foam). The authors used the smallest available size in order to embolize the vessels at the precapillary level. With this technique applied to 13 patients, clinical and echocardiographical improvements were maintained at 3-month follow-up13.
We describe in this report the method of septal artery embolization with straight microcoils deployed into the distal septal arteries through the guide-wire lumen of an over-the-wire balloon in 7 patients with HOCM. This technique was efficient and reduced the resting LVOT pressure gradient by 59% immediately after the procedure and persisted at 3-month follow-up in 6 patients (42% reduction of the LVOT). The clinical status improved significantly in all patients. No major complications were recorded during or after the procedure and permanent pace-maker implantation was not necessary in any patient.
The mechanism by which septal artery occlusion with microcoils causes septal ablation is different from that induced with alcohol injection. Therefore, it might be possible that a purely ischemic infarction could lead to differences in outcome and complications as that reported with a chemically provoked septal necrosis. As in the case of stent graft occlusion of the septal arteries11 and opposed to septal reduction with ethanol, microcoil embolization may induce partial or temporary results in some patients because of possible collateralization, resulting in pressure gradient increase. Procedure repetition and technical refinements (deeper coil delivery inside the vessel; different type of microcoils; increased number of coils) may solve this problem.
Study limitations
This study has a few limitations. At the time the study was performed, the routine procedure did not include 2D contrast echocardiography and the target vessels were identified by sequential measurements of the pressure gradient with inflated balloon in the septal arteries. Other limitations include the reduced number of evaluated patients and the absence of long-term results.
Conclusions
Microcoil embolization is an efficient and safe approach for transcatheter ablation of septal hypertrophy in HOCM. This technique induced myocardial necrosis without the effects of alcohol, potentially reducing the risk of complications (permanent pace-maker implantation, ethanol flow to other myocardial regions). Further experience is necessary in order to asses the medium- and long-term efficiency of this technique and the associated complications.