Abstract
Aim: The immediate and long-term results of balloon mitral commissurotomy (BMC) during pregnancy were evaluated in patients and in their babies looking for radiation side effects.
Methods and results: Sixty one patients (mean age: 28.5±5.0 years) had BMC at a mean age of gestation of 26.8±5.5 weeks. The procedure was successful in all patients except in one who had a severe mitral regurgitation and subsequent mitral valve replacement (MVR). All patients delivered at term vaginally in
58 (95.1%) cases. There was only one death in a patient who delivered at home. At a mean follow-up of 66.8±36.0 months, 4 patients had MVR, the remaining were in NYHA class I/II. Restenosis was found in 4 (7.2%) patients. The 63 babies (two gemellar pregnancies) had a normal weight of birth except of one case of hypotrophy. At a mean follow-up of 64.5±32.5 months, two babies died, 1 had hypotrophy, 2 had microcephaly, 8 had an IQ < 70 but none had a severe mental retardation (IQ <34). None of these events were radiation related.
Conclusion: BMC is the procedure of choice in pregnant patients with mitral stenosis. No late radiation side effects were observed in children but longer follow-up is required.
Introduction
Mitral stenosis during pregnancy carries a considerable risk for both the mother and foetus; however, until the early 1980s, surgery (closed or open mitral commissurotomy and valve replacement) was the only treatment option. Furthermore, surgical treatment during pregnancy has risks; maternal mortality ranges from 1 to 2% for either open or closed commissurotomy and foetal mortality ranges from 5 to 15% for closed commissurotomy and 10 to 33% for open mitral commissurotomy1-3.
Introduced more than two decades ago by Inoue4, balloon mitral commissurotomy (BMC) has become the treatment of choice for mitral stenosis patients with pliable or moderately diseased valves. Performed for the first time during pregnancy by Safian5 and Palacios6 in 1988, the procedure has gained wide acceptance as numerous subsequent reports revealed improvement in maternal-foetal prognosis7-20. However, some reluctance remains because of the risk of foetal radiation exposure and the associated potential for complications.
Thus the purpose of our study was to: (1) assess the immediate, mid (delivery) and long-term results of BMC during pregnancy, and (2) evaluate the babies’ status at birth and during development; specifically, focusing on potential radiation effects.
Methods
BMC procedure
The BMC procedure was performed as previously reported7,8.
We used a double balloon technique in 51 patients (83.6%) and the Inoue balloon in an additional 10 (16.4%) patients.
Study populations
Our study population comprised on one hand 61 women with severe MS that had between November 1990 and March 2003 a BMC procedure during pregnancy, and on the other hand their 63 babies (two gemellar pregnancies).
Pregnant population
The mean age was 28.5±5.0 (range 18-43) years and the mean gestation period was 26.8±5.5 (range 14-36) weeks.
Forty-six (76%) patients were in class III or IV and 15 (24%) were in class II of the New York Heart Association functional classification. Five (8.2%) patients were in atrial fibrillation.
All patients underwent a 2D echo-Doppler examination and a transoesophageal echocardiogram before the procedure. Mitral valve structure was assessed using the Wilkins score21, which averaged 7.1 ± 2.1 (range 4 to 14).
Mitral regurgitation, assessed by colour Doppler using Helmcke classification22, was grade 1 in 3 patients and grade 2 in 2 others. No patient had a significant concomitant disease of the other valves.
Children population
This population comprised 63 children (33 girls); including 4 from gemellar pregnancies. Weight at birth was 3.2±0.5 (range 1.8 to 4.4) kilograms (kg). Hypotrophy, defined as weight at birth <–2 SD of the reference curve was, observed in only 1 child. The distribution of birth weight in the population is depicted in Figure 1.
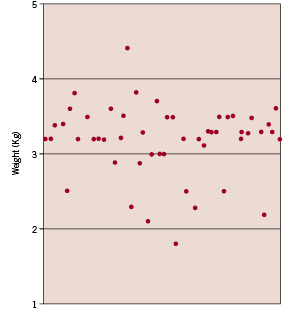
Figure 1. Distribution of weight at birth in the babies population.
The Apgar score was >9/10 in all babies. The children’s mean age at the time of evaluation was 5.3±2.7 years (range 3 months to 11 years).
Long-term follow-up
Mother’s evaluation
After delivery patients were requested to return for a clinical and echocardiographic evaluation every six months for the first two years and at yearly intervals thereafter. Clinical and echocardiographic data were obtained in 59 (96.7%) patients at a mean follow-up of 66.8±33.3 (33-133) months.
Children’s evaluation
Among the initial population of 63 babies, 60 (95.2%) were evaluated at a mean follow-up of 66.8±36.3 months after BMC. Parents were requested to give precise information about the clinical events that occurred in their child since birth, especially the reasons for consulting a paediatrician and whether a hospital admission was required. For each child, we measured, weight, height and head circumference and compared the results obtained to the normal values for the same age23. For that purpose, normal curves expressed in mean and standard deviation were used; a value within 2 standard deviations of the average curve was considered to represent normal. We also performed a mental assessment. This evaluation consisted of a determination of the intelligence quotient (IQ) using a standardised test; Differential Scales for Intellectual Efficiencies (DSIE)24. The customisation of this test for the Tunisian population was performed in a group of children from different regions of the country25.
The purpose of this evaluation was to estimate the mental age of the child and thus determine IQ according to the following formula:
Mental age
IQ =
Physiological age
A mental deficiency was defined as an IQ <70. Based on the French classification of mental abnormalities in children and adolescents26, three levels of mental deficiency were defined: mild (50 >IQ < 70), moderate (35 >IQ < 49), and severe (20 >IQ < 34). This evaluation was performed in every child by the same paediatric psychologist.
Statistical analysis
Data were entered using Norton Editor and See-Editor software. Descriptive analysis and comparison of means was performed using “Biomedical Package for statistical analysis” (BPDP) software. Results were expressed as mean ± standard deviation. The mean, pre, post and follow-up BMC variables were compared using student t-test.
After assessment of the mental development and determination of IQ in each child, we matched our population according to age and gender versus a normal population. The mean IQs in the two populations were compared using student t-test. Comparison was performed between the two populations and between each age category in both groups. Predictors of hypotrophy and mental retardation were determined using univariate analysis. Statistical analysis was performed using “Statistica” software version 5.1.
Results
Immediate results
After BMC, left atrial pressure significantly decreased from 28.5±9.5 to 14.1±5.8 mm Hg and the mean transmitral pressure gradient decreased from 22.5±8.6 to 5.4±3.5 mm Hg (p< 0.001). In contrast, cardiac index significantly increased from 3.0±0.9 to 3.7±0.8 l/min/m2. Mitral valve area (MVA), calculated by 2D- echo planimetry has significantly increased (p< 0.001; Figure 2).
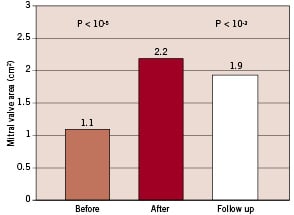
Figure 2. 2D-Echo Mitral valve area (MVA) before, after the procedure and at follow-up (F/U)
There were no procedure failures, in-hospital death or systemic embolism observed in these patients.
Mitral regurgitation (MR) was originally present in only 5 (8.1%) patients (grade II in 2 and grade I in 3); however, after BMC, it was found in 19 (31.1%) patients. There were 14 (22.9%) cases of new mitral regurgitation in addition to the 5 with prior MR that did not worsen in any case. Severe MR occurred in only one patient who underwent emergency mitral valve replacement.
Delivery
All patients delivered at term; vaginally in 58 cases (95.1%) and by caesarian section for obstetrical reasons in 3 (4.9%). One patient, from a rural area, delivered at home.
Delivery was uneventful in all cases except for the patient who delivered at home; this patient died after giving birth to an apparently healthy baby boy, who subsequently died three days later from dehydration.
Long term follow-up
Mothers evaluation
At a mean follow-up of 66.8±36.0 (3-133) months, clinical and echographic data was available in 59 patients (96.7%). One patient, who had an excellent immediate BMC result was lost to follow-up; as mentioned, one patient died following home delivery and 4 (6.5%) patients had mitral valve replacement during the follow-up period:
– One patient had recurrent restenosis following 3 BMC procedures. Her MR was grade II and she also had severe tricuspid regurgitation that required a tricuspid valve repair in addition to the mitral valve replacement.
– One patient developed bacterial endocarditis of the mitral valve 12 months after BMC resulting in severe (grade III) MR due to chordal rupture with restenosis (MVA: 1 cm2).
– One patient had restenosis 24 months after the procedure, with moderate MR that led to hospitalisation for heart failure.
– One patient required emergent mitral valve replacement after BMC (complicated by a severe MR due to chordal rupture).
The remaining patients were clinically improved; 92% were in NYHA functional class I or II.
Although 2D echo-MVA was quite large at long-term follow-up, it had significantly decreased from 2.2±0.3 cm2 to 1.9±0.4 cm2 (Figure 2). Restenosis, defined as 2D-echo MVA <1.5 cm2, was found in 4 (7.2%) patients.
Children’s evaluation
Only one child was lost to follow-up and two died (one at day 3 from dehydration and one from hepatitis at age 3). Sixty children (95.2%) were evaluated at a mean follow-up of 66.8±36.3 months after BMC. At this time, their average age was 64.5±32.5 (3-132) months. We assessed pondostatural thriving in all children; how-ever, mental development was evaluated in only 51 (those 3 years of age or older) because the DSIE test cannot be applied to younger children.
PONDOSTATURAL GROWTH
The distribution of the children’s weight according to age and gender versus normal curves is depicted in Figure 3.
Figure 3. Distribution of girls and boys according to their weight.
All children had a normal weight except for one boy with neonatal hypotrophy. All subjects had a normal height for their age and gender (Figure 4).
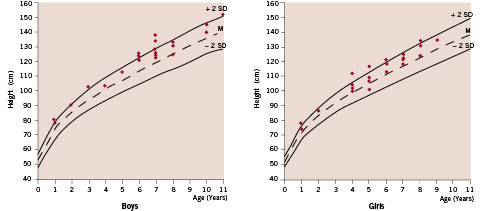
Figure 4. Distribution of girls and boys according to their height.
Similarly, head circumferences were normal except for two females with microcephaly (Figure 5).
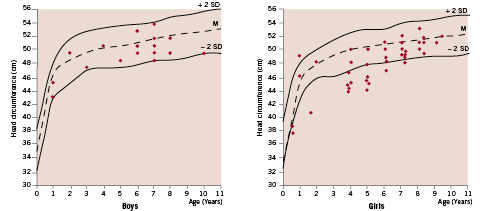
Figure 5. Distribution of girls and boys according to their head circumference.
MENTAL EVALUATION
Our IQ evaluation indicated that 43 (84.4%) children were in the normal range, whereas 8 (15.6%) had an IQ <70. Comparison of our population with a control population did not show a significant difference (p= 0.77). Mean IQ in our population was 93.8±21.5 versus 92.6±19.8 in controls.
Discussion
We aimed to evaluate the immediate, mid-term (until delivery) and long-term results of BMC during pregnancy and to assess the children for potential radiation side-effects.
Immediate results
In our series which is, to the best of our knowledge, the largest during pregnancy, BMC produced an improvement in all measured haemodynamic variables; a decrease in mitral gradient from 22.5±8.6 to 5.4±3.5 mm Hg and an increase in cardiac index from 3.0±0.9 to 3.7±0.8 l/mn/m2.
These haemodynamic results were similar to those reported in most series with a mitral gradient <6 mm Hg and a left atrial pressure <16 mm Hg after BMC (Table 1).
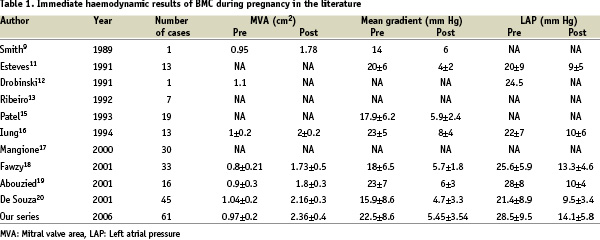
Similarly, there was an increase in MVA assessed by 2D-echo from 1.1±0.2 to 2.2±0.3 cm2. These results were also comparable to those previously reported7-20.
It is also important to note that MVA in our series was comparable to that obtained in non-pregnant patients27-32, which implies that pregnancy per se is not an obstacle to successful BMC.
We had no procedural failures. In contrast, De Souza20 reported two procedural failures in a series of 21 patients. This difference may be explained by two factors; first the young age of our patients and thus their favourable anatomy, and secondly, by the fact that our experience of BMC during pregnancy has began 3 years after the introduction of the technique in our institution that is after reaching the plateau of the learning curve.
Trivial (grade I) or moderate (grade II) MR is common after BMC, whereas severe (grade III/IV) is rare. In fact, this latter was observed in only one (1.6%) of our patients and only one (5.2%) patient of Patel’s study15. The low rate of severe MR in pregnant patients may explain the difficulty in identifying predictors of this event. In fact, there is no consensus on the predictors of severe MR following BMC in any setting27-33 and in most reports the presence of trivial MR before the procedure does not predict that event. No death was observed in this series or in any other reported series.
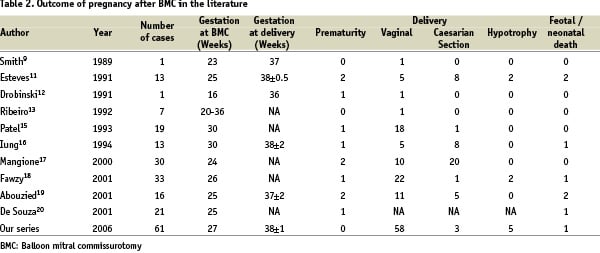
Mid-term outcome: delivery
Maternal status
In most cases, we found that BMC improved clinical parameters prior to delivery. Apart from the patient who died after delivery at home, there were no other adverse events. In fact, no deaths or delivery complications have been reported8-20. In addition to its positive impact on mortality, BMC seems to influence the way of delivery. In our study, delivery occurred vaginally in all but 3 patients; these caesarian sections were performed for obstetrical reasons. In contrast, in Mangione’s series17, two thirds of the patients delivered by caesarian section. It is uncertain whether this high percentage was due to obstetrical reasons or to a desire of the obstetrical team to avoid potential complications of vaginal delivery.
Foetal status
We observed hypotrophy in only 1 (1.6%) baby versus 2 (15.3%) in Esteves’s11 and 2 (8.7%) in Fawzy’s studies18. No predictors could be identified by univariate analysis, particularly with regard to the age of gestation that does not seem to influence the risk of hypotrophy. There were no cases of prematurity or foetal distress in our series. In contrast, the rate of prematurity in the literature ranges from 2.2% to 20%16-20, and the clinical course of these babies is often unfavourable with a high risk of death due to respiratory failure. Prematurity was the main risk factor of neonatal death in the literature2,3,16,17,20. The only death observed in our series was due to dehydration 3 days after delivery at home; likely in septic conditions.
The outcome of pregnancy after BMC in the literature is presented in Table 2.
Long-term results
Long-term results of mothers
In our series, 59 (96.7%) patients were evaluated clinically and echographically at a mean follow-up of more than 5 years. This is the highest percentage ever reported; Mangione et al.17 examined 19 patients among 30 (63%) and Fawzy et al18 23 among 33 (69%) at mean follow-up periods of 61.2±33.6 and 63.9±37.4 months respectively.
There was a significant reduction in MVA by 2D echo and Doppler compared to the immediate results in our series. 2D-MVA decreased from 2.24±0.35 to 1.99±0.47 cm2 and Doppler MVA from 2.26±0.37 to 2.02±0.51cm2 (P<10–3). Restenosis was observed in 4 patients (7.2%), two of them had mitral valve replacement, the two others were asymptomatic and therefore did not have reintervention.
Similarly, Mangione17 reported a significant reduction in MVA at follow-up that decreased from 2.01±0.21 to 1.75±0.24 cm2, and restenosis was observed in two cases (8.6%).
Fawzy18 also reported a reduction in MVA (1.97±0.36 to 1.8±0.5 cm2) with three cases (16%) of restenosis.
The rate of restenosis in our series and of Mangione was lower than reported in non- pregnant patients33. This is not surprising considering that the patients were young and had, in most cases, a favourable anatomy. The higher restenosis rate in Fawzy’s series was likely due to a selection bias because only 19 out of 33 patients were followed.
Long-term results of children
The purpose of follow-up in the children population was to look for radiation side-effects related to X-ray exposure during pregnancy. Although few studies have examined such side-effects, several investigators have assessed side-effects in subjects exposed to atomic bomb-associated radiation34-38.
Risk factors to develop radiation side effects
Radiation side effects are numerous, the most frequent are the risk of malformation, thriving and/or mental retardation and the risk of childhood cancer. Unlike the risk of cancer that is a stochastic (not dose dependent) complication, two parameters are predictors of radiation side effects: gestation age and radiation dose. For the first factor, it is accepted that the vulnerable period for foetal radiation is the first trimester39. For some side-effects, particularly mental retardation40, this vulnerable period might extend to the 25th week after ovulation (i.e. 23rd week of gestation). In our series, the mean gestation age at the time of BMC was 26.8±5.5 weeks (range from 14 to 36), which is comparable to other series. For the second factor, the threshold for the radiation dose to induce mental retardation is well known; however, it is not well defined for the risk of pondostatural retardation. The risk of severe mental retardation is likely to occur for doses greater than 0.3 Gy40-42.
Otake et al.40 reported that the threshold dose for the risk of mental retardation was 0.15 to 0.25 Gy for the period between 8 and 15 weeks post ovulation and 0.25 to 0.28 Gy at 16 and 25 weeks after ovulation. In our series, the absorbed dose was not determined however, it can be approximated. The fluoroscopy time was 14.6±5.03 (range from 3 to 26) minutes in our series and of 15±9 min and 9.2±3.4 min in Iung’s14 and Patel’s15 series respectively. The absorbed dose in Iung’s series was less than 0.5 cGy and therefore much less than the reported adverse threshold doses. In less experienced hands, fluoroscopy time might be longer but it is unlikely that in any case the absorbed dose can reach a hazardous level. The use of transoesophageal echocardiography during the procedure might be helpful in reducing the fluoroscopy time but would certainly complicate the procedure.
Thriving retardation
In animals, radiation exposure to approximately 10 rad during embryogenesis resulted in thriving retardation with a reduction in body and some organ’s weight particularly the brain41.
In man, these effects – especially reduced body weight, height and head circumference – were seen in children whose mothers were exposed to radiation in Hiroshima and Nagasaki. In fact, the reduction in head circumference was the most frequent and most significant manifestation of damage. In the most extreme cases, microcephaly was accompanied by mental retardation41.
In our series, normal thriving was seen in all children except for one hypotrophic boy who had a body weight less than –2 DS, and two girls who had head circumferences less than –2 DS. The boy’s height and head circumference at follow-up were normal. His IQ was not evaluated because he was less than 1 year old at the time of the study. Similarly, the two girls had normal weight and height and their IQ was 100 and 75 respectively. It is unlikely therefore, that these findings were radiation related. In Fawzy’s18 et Mangione’s17 reports there were no thriving retardation cases.
Mental retardation
Mental retardation is the most difficult side effect of radiation to identify. The association with microcephaly is not constant39. For example, in a group of 26 patients with severe mental retardation, only 15 (58%) had a microcephaly40. In contrast, in 62 cases with microcephaly in the same study, only 15 had severe mental retardation.
In our series, 51 children, aged from 3 to 11 years, had a mental evaluation. Based on the French classification for child and adolescent mental disorders26, no severe mental retardation (20 The statistical analysis aiming at comparing our population to a control sample did not show a significant difference between the two populations. No predictors particularly with regard to the age of gestation and the fluoroscopy time were identified by univariate analysis. In his study, which is the only one to analyse the consequences of BMC during pregnancy in children, Kinsara et al did not find any cases of mental retardation in a series of 20 cases43. We conclude that BMC is the procedure of choice in young pregnant mitral stenosis patients and has a very low incidence of adverse events. In addition, the long term outcome of children did not show any radiation side effects related to BMC during pregnancy. A longer follow-up is however necessary to rule out any late appearance of side effects particularly malignant complications. Acknowledgements We thank Peter Whittaker PhD, for reviewing this manuscript.