Abstract
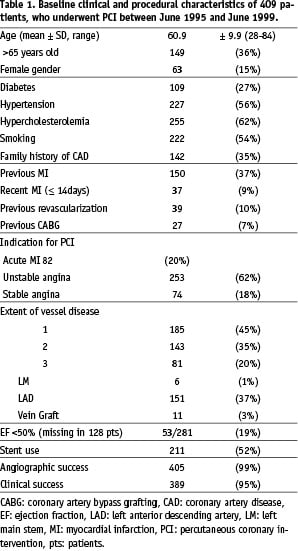
Objectives: This study reports the 9-year clinical outcome of 409 consecutive patients, who underwent coronary angioplasty with provisional stenting during the years 1995 to 1999 in the University Hospital of Northwestern Greece.
Background: Despite the rapid changes of interventional cardiology, long-term follow-up studies are useful for identifying its limitations and indicating future changes.
Methods: Baseline characteristics and information on survival, major cardiac events and symptoms were retrospectively obtained from medical records or telephone contact. Patient survival rates were calculated and predictive factors for survival and cardiac events were identified.
Results: Follow-up information was obtained in 403 patients (98.5%). Three hundred and thirty-one patients (82%) were alive with 150 (45%) being symptom free. The cumulative 5- and 9-year survival rates were 87% and 78% respectively, and the corresponding survival free from major adverse cardiac events was 65% and 55%. Independent factors affecting survival were age>65 years, diabetes, hypertension, multivessel disease and ejection fraction<50%, while stenting and the indication of acute myocardial infarction for intervention influenced independently survival from cardiac death. Non-diabetics, aged≤65, with single-vessel disease suffering from unstable or stable angina had a survival rate similar to that of the general Greek population (survival at 9 years: 92% vs. 93% respectively).
Conclusions: Certain factors influence long-term survival after balloon angioplasty with provisional stenting and almost half of the patients (45%) experience a further cardiac event during a 9 year follow-up period.
LIST OF ABBREVIATIONS AND ACRONYMS
CABG: coronary artery bypass grafting
CAD: coronary artery disease
CI: confidence interval
ECG: electrocardiogram
LVEF: left ventricular ejection fraction
MI: myocardial infarction
MVD: multivessel disease
PCI: percutaneous coronary intervention
PTCA: percutaneous transluminal coronary angioplasty
rePCI: repeat percutaneous coronary intervention
SVD: single-vessel disease
Introduction
The introduction of percutaneous transluminal coronary angioplasty (PTCA) into clinical practice by Andreas Gruentzig in 1977 changed the therapeutic management of patients with coronary artery disease1,2. The efficacy of this technique in different populations, men and women3,4, single- and multi-vessel disease5,6, young and elderly patients7,8, has been demonstrated in both the short and the long-term9-11.
Acute thrombosis and restenosis constituted the major drawbacks of balloon angioplasty during the early period12. The addition of stents in the late 80s reduced the rates of these adverse events and altered the way that coronary artery disease (CAD) patients were managed in the catheterization laboratories13. In the 1990’s, the interventional strategy applied in CAD patients was initial management of the coronary lesions with balloon angioplasty and usage of stents either in the case of a complication or a suboptimal result or electively in cases that were presumed to be of high peri-procedural risk (balloon angioplasty with provisional stenting).
Long-term (> 5 years) clinical studies, addressing the question of prognosis for survival free from major adverse events after balloon angioplasty with provisional stenting, have not been presented.
Currently, the up to 9 years clinical course of a consecutive heterogeneous patient population undergoing balloon angioplasty with provisional stenting is described and the predictors of adverse cardiac events are assessed. Furthermore, patients at low risk for future events are identified and their survival is compared to that of the general population.
Methods
Study population
Between June 1, 1995 and June 30, 1999 balloon angioplasty with provisional stenting was attempted in 442 consecutive patients residing permanently in the catchment area (Northwestern Greece) of the University Hospital of Ioannina, Greece. The reason for the percutaneous coronary intervention (PCI) in this group of patients was stable angina, unstable angina or acute myocardial infarction (MI). After the exclusion of 33 patients with chronic total occlusions, in whom the lesion was not crossed by a guide-wire and the interventional procedure was subsequently abandoned, the study cohort consisted of 409 patients (Table 1). PCI was performed according to standard clinical practice after written informed consent was given. Stents were implanted either electively, for cases that were presumed to be of high risk, or as a bail-out procedure in case of a complication or a suboptimal result. The administration of abciximab, which was available after 1997, was upon the operator’s discretion. After the procedure all patients were treated with 500 mg ticlopidine daily for 1 month and 100 mg aspirin daily for life.
Data collection and follow-up
Retrospective chart review was carried out to obtain baseline clinical characteristics, procedural information and in-hospital events. Long-term outcome data were based on telephone contact with the patients or their referring cardiologist. Attention was focused on the occurrence of major adverse cardiac events [death, non-fatal Q-wave MI (prolonged chest pain and evolution of new Q waves), coronary artery bypass grafting (CABG) and repeat percutaneous coronary intervention (rePCI)] and symptoms of angina pectoris (graded according to the Canadian Class Society classification) for surviving patients. Review of hospital records enabled us to cross-check the data and complete missing information. Complete clinical follow-up was obtained in 403 (98.5%) patients.
Definitions
Unstable angina was defined as new-onset angina (within 8 weeks), angina at rest, progressive angina or post-MI angina. Acute MI was considered to have occurred when at least 2 of the following 3 criteria were met: (1) chest pain lasting longer than 30 minutes, (2) persistent electrocardiographic changes suggestive of ischemia or (3) greater than or equal to two-fold elevations in serum creatine kinase levels with a corresponding increase in the MB isoform. Thereby, the indication for the interventional procedure was coded as acute MI if the procedure had taken place within 12h after the onset of chest pain.
A vessel was considered diseased when a luminal narrowing of 50% in a major epicardial artery or one of its major branches was estimated by visual assessment in more than one projection. Multivessel disease (MVD) was defined when more than one major coronary artery systems were diseased and complete revascularization as a 20% reduction in lesion severity with final stenosis <50% (angiographic success) in all diseased coronary arteries after interventional treatment.
Clinical success was defined as angiographic success without in-hospital complications of death, Q-wave acute MI and emergent CABG. Left ventricular ejection fraction (LVEF) was determined, where possible, by left ventriculography and was classified as moderate/low (<50%) and mildly affected/normal ≥ 50%).
Statistical analysis
Continuous variables (presented as mean ± standard deviation) were analyzed by unpaired t-test and categorical variables (presented as counts and percentages) were compared by X2 test or Fisher’s exact test when appropriate. Survival and event-free survival rates were estimated using the Kaplan-Meier method and differences between groups assessed using the log-rank test. Multivariate Cox regression with forward and backward stepping algorithms was used to identify baseline variables related to long-term survival and event-free survival independently. Baseline variables tested were age, gender, diabetes, hypertension, family history of coronary artery disease, previous MI, prior revascularization, indication for PCI, MVD, LVEF and stent use.
Baseline data was available in all patients with complete follow-up except for LVEF (available in 69% of them). Therefore, we first estimated the unadjusted and adjusted impact of LVEF on freedom from death or other events using only the data from the patients with known LVEF. Furthermore, the patients with unknown ejection fraction were classified as a separate group regarding LVEF and the main multivariate analysis was performed in all patients. In this analysis, the variable “LVEF” was included as a nominal variable with three categories (i.e. unknown, LVEF<50% and LVEF≥50%) and the category representing LVEF≥50% was used as reference category for calculating the hazard ratio versus the two other categories.
In-hospital events were included in the analysis of follow-up events. All tests were two-tailed and p value <0.05 was considered significant. The SPSS statistical software package (version 12.0 for Windows, SPSS Inc. Chicago, Illinois) was used.
Results
Median follow-up duration for the 403 patients was 6.33 years (range: 0-9 years) and median follow-up interval of the 331 survivors was 6.75 years (range: 5.1-9 years). During the follow-up period, 72 (18%) patients died, 53 patients because of cardiac causes (5 unknown causes are included) and 19 patients due to other causes (9, cancer; 3, end-stage renal disease; 3, stroke; 2, septicemia; 1, aortic dissection; 1, accident). Furthermore, 24 (6%) patients experienced a myocardial infarction and 102 (25%) patients underwent a repeat revascularization procedure (CABG, 23; angioplasty, 71; both, 8). The reason for a repeat revascularization was restenosis in 71 and a new lesion in 31 patients.
The cumulative 5- and 9-year patient survival rates were 87% and 78% respectively (survival from cardiac death 89% at 5 years, 84% at 9-years) and the corresponding survival rates for freedom from death, MI, CABG and repeat PCI were 65% and 55% (Figure).
Figure: Nine-year cumulative survival (Death), death- and myocardial infarction-free survival (Death-MI), death-, MI- and CABG-free survival (Death-MI-CABG) and death-, MI-, CABG- and repeat PCI-free survival (Death-MI-CABG-rePCI). The + sign refers to censored patients.
Regarding the anginal status of the survivors at follow-up, 150 (45%) were asymptomatic, 139 (34%) had mild angina (Class I), 36 (11%) moderate (Class II) and 6 (2%) severe angina (5, Class III; 1, Class IV). Surviving patients were classified in angina-free and symptomatic patients, and the influence of the baseline variables in the appearance of angina was assessed. Elderly (>65 years) (odds ratio [OR]: 4.8, 95% confidence interval [CI]: 2.8-8.3), women (OR: 4.1, 95% CI: 2-8.4) and patients with MVD (OR: 1.7, 95% CI: 1.1-2.6) had a significantly greater risk for presenting with angina at follow-up.
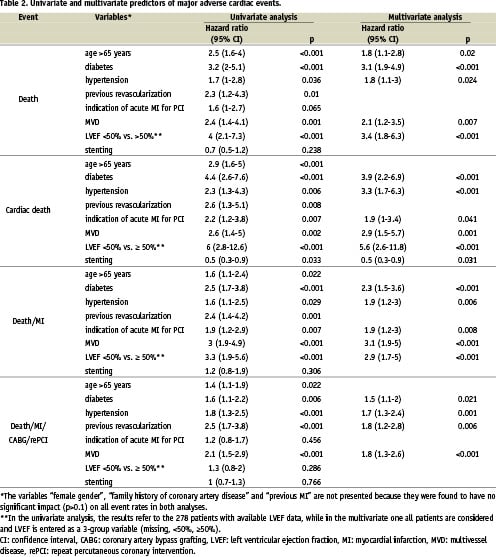
Predictors of major adverse cardiac events
In the univariate analysis, old age (>65 years), diabetes, hypertension, history of previous revascularization, indication of acute MI for PCI, MVD and impaired LVEF (<50%) were found to have the most significant negative impact on survival (Table 2). Multivariate Cox proportional-hazards model in patients with known LVEF demonstrated that moderate/low LVEF had a major significant impact on mortality (hazard ratio [HR]: 3.3, 95% CI: 1.8-6.3). When all patients were included in the analysis, the following independent
predictors of survival were identified: age>65 years (HR: 1.8, 95% CI: 1.1-2.8), diabetes (HR: 3.1, 95% CI: 1.9-4.9), hypertension (HR: 1.8, 95% CI: 1.1-3), MVD (HR: 2.1, 95% CI: 1.2-3.5) and LVEF <50% vs. (50% (HR: 3.4, 95% CI: 1.8-6.3). Furthermore, diabetes, hypertension, MVD and LVEF <50% were proven to be independently associated with most of the different composite events, while coronary stenting was found to favour survival from cardiac death as an independent predictor (Table 2).
In addition, stable or unstable angina patients aged <− 65, who did not suffer from diabetes and MVD, were found to have a very high survival rate (96% at 5 and 92% at 9 years), which was similar to the cumulative expected survival rate of the general population in Greece, matched for age and gender (97% at 5 and 93% at 9 years).
Discussion
In the mid 1990’s, the strategy employed by interventional cardiologists was “balloon angioplasty with provisional stenting”. Currently, we report the first extended clinical follow-up of 409 patients representative of the Greek population, who underwent balloon angioplasty with provisional stenting between 1995 and 1999, and the predictors of major adverse cardiac events. Our study group included patients undergoing PCI mainly because of an acute coronary syndrome, constituting thus “real world” percutaneous coronary interventions in that era.
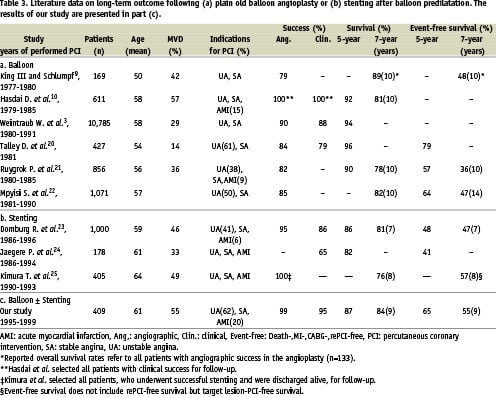
Comparison with other interventional practices
The overall survival in our patient group was similar to that of previously reported long-term follow-up studies of plain old balloon angioplasty performed mainly in the eighties (Table 3a). This, rather not expected, finding could be possibly accounted for by significant differences between patient populations. Our patients were older, more likely to have MVD and were referred for PCI mostly because of unstable angina, while patients suffering from an evolving acute MI were not excluded and corresponded to 20% of all patients. However, the event-free survival rates in the present study (55% at 9 years) were more favourable despite the less propitious baseline characteristics, which clearly represent patients encountered in recent and current interventional practice. Our findings were highly comparable to those of studies following up the clinical outcome of a “general” patient population after coronary stenting in the early nineties (Table 3b).
Factors influencing adverse events
Certain factors (e.g. age, diabetes, MVD, LVEF) still dominate on shaping the clinical course of a patient after an interventional procedure. Elderly (>65 years) and younger patients were found to have significant differences in 9-year survival and event-free survival rates in favour of the younger and “age>65” was identified as an independent predictor of mortality. Similar findings have been reported in the past; van Domburg et al. found a difference of 29% (p<0.0001) in the 15-year survival rate after PTCA in favour of patients <60 years11.
It is well known that diabetes not only increases the incidence of CAD, but also contributes to a less favourable prognosis in CAD patients. In the Registry of National Heart, Lung and Blood Institute, the adjusted mortality calculated at 9 years after PTCA was twice as high in diabetics versus non-diabetics14, while the experience of Emory University confirmed the survival benefit of non-diabetics15. Our results demonstrate similar advantages of non-diabetics, since diabetes was found to affect independently all major adverse cardiac events at follow-up and stenting did not seem to alter this negative effect.
As it has been previously reported, the extent of CAD is a well-accepted determinant of survival. Henderson et al. compared the long-term clinical results of coronary angioplasty in 448 SVD and 451 MVD patients and reported higher rates of cardiac death, MI, CABG and angina at follow-up (39% vs. 27%) in MVD patients16. In addition, data of 10,783 patients from Emory University affirmed that patients have increasing in-hospital and long-term mortality as the severity of disease increases17. In accordance with the above-mentioned reports, our findings demonstrate the same disadvantages of MVD patients for presence of angina at follow-up and for occurrence of any adverse event after a PCI.
The negative influence of impaired left ventricular function on a patient’s mortality demonstrated in the past18,19, was confirmed in the present study; LVEF <50% was identified as the most significant independent predictor of all-cause and cardiac mortality.
Based on the aforementioned data, survival following a PCI may vary substantially according to the patient’s specific characteristics. In our study population, rather young patients <− 65 years) suffering from unstable or stable angina, who were not diabetic and had single-vessel disease presented a very low risk for future events and their survival was almost identical to that of the general Greek population, matched for age and sex. These findings are in accordance with the previously reported for the Dutch population11.
Study limitations. This is a single-centre retrospective study and therefore the results are limited by the shortcomings inherent to this type of studies. The study population is of medium-size, a fact which may diminish the statistical importance of some of the results. Nevertheless, this study reports an extended long-term clinical outcome of consecutive highly unselected patients treated in the everyday interventional practice.
Conclusion
Certain factors, known from previous reports to predict long-term outcome, were identified to play a significant role in mortality and event-free survival in a Greek patient population who underwent balloon angioplasty with provisional stenting. Non-diabetics aged <− 65 with single-vessel disease suffering from unstable or stable angina presented a group with low long-term mortality.