Abstract
Background: A prospective, randomised, single centre study was designed to test the safety and efficacy of nicorandil infusion, a potassium channel opener, prior to reperfusion in ST-elevation acute myocardial infarction (STEMI).
Methods and results: Seventy STEMI patients with TIMI 0 to 2 flow were randomly assigned to nicorandil (Group N; n = 35) or control (Group C; n = 35) and underwent direct percutaneous coronary intervention (PCI). In Group N, 2 mg of nicorandil was infused directly into the infarct area prior to reperfusion. Incidence of anterior infarction was 60% in both groups. With nicorandil infusion, additional ST elevations without chest pain were observed for a few minutes in 94% of cases. However, no ventricular fibrillation or ventricular tachycardia occurred. TIMI myocardial perfusion grade 3 was significantly higher in Group N (40% vs. 17%, p<0.01). Patients were followed for up to 8 months, with similar incidence of major clinical adverse events, however left ventricular regional wall motion score significantly improved in Group N (P < 0.05). The effect of nicorandil was seen in patients without ischaemic preconditioning (P < 0.05).
Conclusion: This study suggests that direct infusion of nicorandil prior to revascularisation may be safe and beneficial.
Introduction
Primary percutaneous coronary intervention (PCI) has improved prognosis in patients with acute myocardial infarction (AMI). However, some patients continue to have deteriorating cardiac function after primary PCI, thought to be due to reperfusion injury. Restoration of blood flow to cardiac cells damaged by ischaemia may result in irreversible injury to these cells1. Several studies have demonstrated that myocardial infarct size is larger with versus without reperfusion following ischaemia2,3.
In the reperfusion injury model, brief occlusion of the coronary artery prior to ischaemia markedly reduces infarct size4. This phenomenon is called ischaemic preconditioning. Ischaemic preconditioning is also reported to exist in humans5,6. Both sarcolemmal and mitochondrial potassium channels play a central role in ischaemic preconditioning7. It is therefore anticipated that a therapeutic drug of the potassium channel opener class would inhibit deterioration of left ventricular function in patients with AMI through a preconditioning effect. Nicorandil, N-(2-Hydroxyethyl) nicotinamide nitrate, a hybrid adenosine triphosphate (ATP)-sensitive potassium (KATP) channel opener and nitrate compound, is the only clinically available potassium channel opener at present.
It has been demonstrated that intravenous infusion of nicorandil protects against myocardial damage in patients with AMI8,9. In addition, it was reported that oral nicorandil reduces cardiac events in patients with stable angina10. Intravenous injection of nicorandil prior to PCI for patients with stable angina induces pharmacological preconditioning11. However, the cardiac protection of potassium channel openers against reperfusion injury is still unknown in patients with AMI. We hypothesised that direct infusion of nicorandil into an infarct-related artery prior to reperfusion could be safe and potentially beneficial for patients with AMI.
Methods
Patients. This was a prospective, randomised study, conducted at a single centre. The study protocol was approved by the ethics committee of our institute. Between April, 2000 and April, 2003, 122 consecutive patients with first ST-elevation AMI (STEMI) who underwent coronary intervention at our institute were enrolled. Of these, 52 patients were excluded according to the exclusion criteria: 6 patients due to age > 80 years; 12 patients with serum creatinine >2.0 mg/dL; one patient who had taken sildenafil citrate within the prior 24 hours; 6 patients with cardiogenic shock; 2 patients who underwent emergency coronary artery bypass graft after coronary angiography, and 25 patients with Thrombolysis in Myocardial Infarction (TIMI) grade 3 reperfusion on coronary angiography. STEMI was determined by continued chest pain over 30 minutes, ST-segment elevation in two contiguous electrocardiographic leads and a more than two-fold increase in serum creatine kinase. After all exclusions, 70 patients entered the study and were randomised into 2 groups. One group received nicorandil injection (Nicorandil group) prior to reperfusion following angioplasty; the other group did not receive nicorandil (control group) prior to reperfusion. An anginal attack within 24 hours prior to PCI was considered ischaemic preconditioning.
Preparation of nicorandil. Nicorandil powder for intravenous use is approved and commercially available in Japan. Nicorandil was dissolved at a concentration of 1 mg/mL in Ringer’s Lactate solution that contained 130 mEq of sodium and 4 mEq of potassium. Nicorandil becomes readily soluble in Ringer’s Lactate. Dosage of intravenous nicorandil ranges from 2 to 6 mg/hr. In intravenous administration, slow injection of 1 or 2 mg nicorandil is widely applied based on experiences in Japan. Thus, we chose the 2 mg nicorandil dose for use in this study.
Coronary intervention and nicorandil injection. Prior to angioplasty, 100 U/kg of heparin and 50 mg of lidocaine were administered intravenously. After guidewire introduction and crossing, a multifunctional probing catheter (Boston Scientific, Natick, MA, USA) was inserted distal to the culprit lesion (Figure 1).
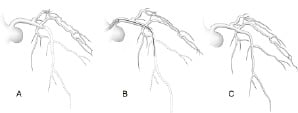
Figure 1. Method of intracoronary injection of nicorandil distal to the culprit lesion. (A) Baseline coronary angiography. (B) After guidewire introduction and crossing, a multifunctional probing catheter was inserted distal to the causative lesion. Then, 2 mg of nicorandil was injected slowly, distal to the lesion, followed by 2 ml flush of Ringer’s Lactate. (C) After the nicorandil injection, angioplasty was performed.
Once the 2 mg dose of nicorandil was slowly injected distal to the culprit lesion, 2 ml of Ringer’s Lactate was used for gentle flushing. In a preliminary study, ventricular arrhythmia was observed just after normal saline flushing in 2 of 4 cases (50%). When the flush solution was changed from normal saline to Ringer’s Lactate, no cases of complicated ventricular arrhythmia occurred. In the present study, coronary intervention was performed immediately after the nicorandil injection and flush. In the control group, no nicorandil injection was given prior to PCI. Stent implantation was then performed at the discretion of the operators.
Medication. After successful PCI, the Nicorandil group were administered intravenous Nicorandil @ 2 mg/h for 24 hours, followed by oral nicorandil @ 15 mg/day. The control group did not receive any nicorandil. No thrombolytic agents or GPIIb/IIIa antagonists were used in either group. Oral ACE-inhibitors or angiotensin receptor blockers were prescribed for all patients. Aspirin plus ticlopidine or cilostazol was used as antiplatelet therapy. In patients with spasm, calcium antagonists or nitrates were used. Beta-blockers were added if blood pressure and heart rate were acceptable.
Analylsis of coronary angiography. Quantitative coronary angiography was performed using QCA-CMS (MEDIS, Medical Imaging Systems, Leiden, Netherland). TIMI myocardial perfusion grade was assessed according to the frame count method described by Gibson et al12. These assessments were performed by an expert cardiologist who was blinded from the clinical data.
Analysis of left ventriculography. Left ventriculography was performed immediately after and 6 months post PCI. End diastolic volume index and ejection fraction were measured using area-length method. To analyse left ventricular regional wall motion, the centreline method was used. In this method, endocardial motion is measured along 100 chords constructed perpendicular to a centreline drawn midway between the end-systolic and the end-diastolic contours in the right anterior oblique projection. The motion of each chord is normalised by dividing by the length of the end-diastolic circumference. Subsequently, this value is converted into units of standard deviation (SD) from normal mean motion of each chord as derived from a normal reference. In the 30 degrees right anterior oblique projection, wall motion score (WMS) was defined as the average SD from chord #10 to #66 for anterior AMI patients. In non-anterior AMI patients, WMS was defined as the average of SD from chord #51 to #8013. ΔWMS was calculated as the value of WMS immediately after PCI minus WMS value at 6 months post PCI.
Follow-up. Follow-up data were obtained from hospital charts and supplemented by the patient’s attending physician notes for 8 months after PCI. Follow-up data included information on recurrent myocardial infarction, congestive heart failure, target lesion revascularisation, cardiac surgery, and death.
Statistical analysis. The planned sample size of 70 patients provided 80 percent statistical power to detect a 20 percent reduction of the primary end point (left ventricular regional wall motion). Statistical analysis was performed using SAS version 8.02 (Cary, NC). Difference between groups was evaluated by the Fisher’s exact test for categorical factors and student’s t test for continuous factors. A P value of less than 0.05 was considered significant.
Results
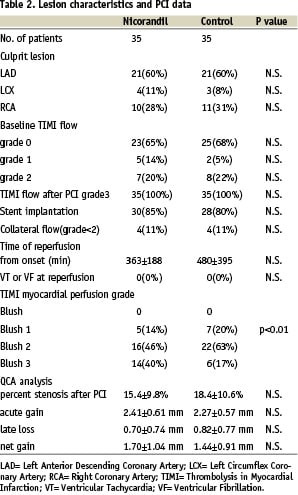
Patient characteristics. Patient characteristics are listed in Table 1.
There was no statistical difference between the 2 groups with respect to baseline characteristics. Drugs on admission or at discharge, including sulfonylureas, ACE-inhibitors, and angiotensin receptor blockers, were not significantly different between the 2 groups, and no patients had previously been treated with nicorandil on admission.
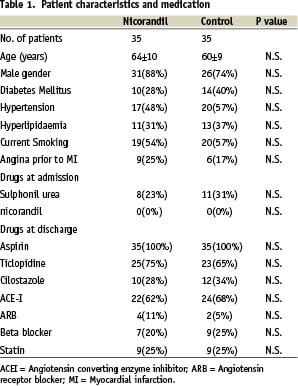
ECG changes during nicorandil infusion. Distinctive ST elevation was observed in leads consistent with infarct areas immediately after nicorandil injection. The ST elevation returned to the level prior to injection within 3 to 5 minutes. Patients did not experience additional chest pain, even with the ST elevation. ECG changes of a typical case are shown in Figure 2.
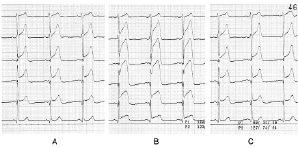
Figure 2. ECG change after injection of nicorandil into infarcted areas. Serial ECGs of V1-6 leads of a 64 year old male with anterior MI are shown. (A) Baseline ECG showed ST elevation in V2-5 leads. (B) Additional ST elevation was observed in V2-6 leads immediately after nicorandil injection. (C) Three minutes after injection, ST elevation returned to the baseline level.
Similar changes were observed in 33 of 35 cases (94%) following nicorandil injection. No ventricular arrhythmia was observed in any of the cases.
Lesion characteristics and PCI data. Lesion characteristics are described in Table 2.
Sixty percent of culprit lesions were in the left anterior descending coronary artery in both groups. TIMI flow at baseline was 0 in 65% of the Nicorandil group, and 68% in the control group (n.s.). Patients with TIMI 3 flow at baseline were excluded according to the study protocol. After PCI, coronary flow improved to TIMI 3 in all patients. Bare metal stents were implanted in 85% of patients in the Nicorandil group and in 80% of the control group. During PCI, no ventricular tachycardia or ventricular fibrillation occurred in either group. TIMI myocardial perfusion grade immediately after the PCI is shown in Figure 3.
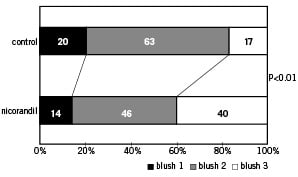
Figure 3. TIMI myocardial perfusion grade immediately after PCI.
No cases were blush 0. Blush 3 was significantly higher in the Nicorandil group (40% vs 17%, p<0.01). No statistical difference was observed in quantitative coronary angiography data between the two groups.
Clinical results. Target lesion revascularisation was 30% in the Nicorandil group, and 22% in the control group (n.s.). Clinical results are shown in Table 3.
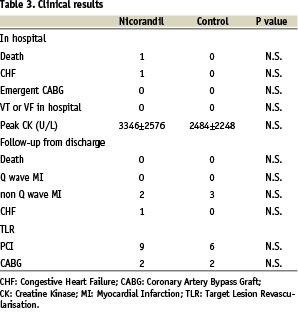
The clinical results were not statistically significantly different between the 2 groups. Maximum serum creatinine kinase level reflective of infarct size was not significantly different between the 2 groups. During the hospital treatment period, one patient died of in-stent thrombosis 24 hours after stent implantation and one patient died of complicated congestive heart failure and renal failure. In the follow-up period, in-stent thrombosis occurred in 5 patients. In 2 patients, worsening of renal failure post intervention was reported. Intraventricular thrombosis was detected in 2 patients, and 2 patients were diagnosed with cancer. For these reasons, follow-up angiography was not performed in these 13 patients.
Left ventriculogram. Left ventriculography data are shown in Table 4.
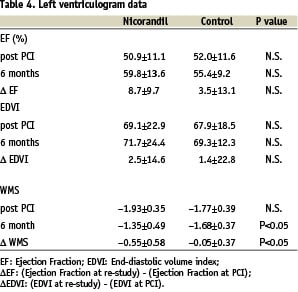
The degree of improvement in ejection fraction between treatment groups did not reach statistical significance (Nicorandil group: 50.9±11.1% to 59.8±13.6%; Control group: 52.0±11.6% to 55.4±9.2%). As for end-diastolic volume index, slight enlargement was observed in both groups, but there was no significant difference. Baseline WMS was not significantly different between the groups. However, WMS of the Nicorandil group was significantly better at 6 months (Figure 4A). Furthermore, the degree in improvement of WMS was greater in the Nicorandil group (–0.55±0.58 vs –0.05±0.37) (Figure 4B).
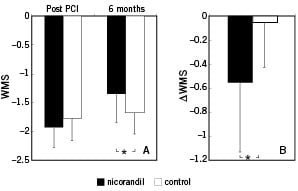
Figure 4. WMS in Nicorandil and Control Groups. (A) Closed bars represent WMS of the Nicorandil group. Open bars represent WMS of the control group. WMS immediately after PCI was not significantly different but WMS 6 months after PCI was significantly better in the Nicorandil group. The error bar shows standard deviation. “*” P < 0.05. WMS = regional wall motion score. (B) A closed bar represents ∆WMS in the Nicorandil group. An open bar represents WMS in the control group. “*” P < 0.05. ΔWMS = differentiation of regional wall motion between immediately after and 6 month after PCI.
Influence of ischaemic preconditioning. Subanalysis was performed to evaluate the influence of ischaemic preconditioning (Table 5).
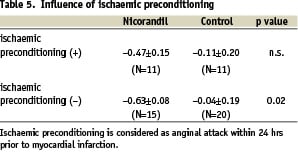
Patients were subdivided into 2 groups, with or without prior angina within 24 hours before PCI, and differences in ΔWMS between the Nicorandil group and the control group were examined. In patients without ischaemic preconditioning, ΔWMS of the Nicorandil group was significantly better than that of the control group. However, in patients with ischaemic preconditioning, the difference was not statistically significant.
Discussion
This study showed that direct infusion of nicorandil prior to revascularisation improved myocardial perfusion grade as well as regional left ventricular wall motion in patients with AMI. In previous studies, nicorandil was reported to be effective for patients with AMI. Ito et al reported that intravenous nicorandil in conjunction with coronary angioplasty preserved left ventricular function8. Sakata et al reported that intracoronary nicorandil following revascularisation restored myocardial blood flow14. Although drug infusion prior to revascularisation has been the standard in animal models15,16, to the best of our knowledge, this is the first study in humans to demonstrate the safety and efficacy of intracoronary nicorandil prior to reperfusion in patients with AMI. Improvement of WMS was 10-times more than the control in this study. In contrast, intravenous nicorandil improved WMS 2.5-times than the control8, although comparisons with different study protocols cannot be made.
It is still unclear whether intracoronary nicorandil prior to reperfusion has an additional benefit over intravenous nicorandil injection. Nicorandil can activate KATP channels through the same pathway as angina-induced ischaemic preconditioning. Thus, the protective effect of Nicorandil may be due to the pharmacologically-induced preconditioning. Ishii et al reported that intravenous nicorandil administration prior to revascularisation improved TIMI flow at post-procedure, as well as significantly lower clinical complication rates through 2.4 years follow-up. They suggested that nicorandil administration prior to revascularisation may have an advantage by providing pharmacological preconditioning for ischaemic myocardium17. We believe that intracoronary injection performed in this study safely demonstrated nicorandil administration prior to reperfusion. This method may have potential for improvement in left ventricular function.
Other than pharmacologic preconditioning, patients receiving the nicorandil injection resulted in better myocardial perfusion. This finding is also considered as an effect of KATP channels being able to dilate resistance arteries less than 100 µm in diameter18,19. Marzilli et al. reported that intracoronary adenosine as an adjunct to primary angioplasty was effective in improved ventricular function20. A KATP channels opener may offer an additional therapeutic agent to improve myocardial perfusion as well as ventricular function. Based on this mechanism, intracoronary nicorandil injection prior to reperfusion may offer an additional benefit for myocardial perfusion in patients with AMI.
In this study, compared to patients without having an anginal event prior to infarction, the effect of nicorandil in protecting left ventricular regional wall motion was not observed in patients with ischaemic preconditioning. It is still undetermined whether the pharmacologic manner had significant influence on ischaemic myocardium with already activated KATP channels by ischaemic preconditioning. Further observation is needed to establish the influence of pharmacologic preconditioning in the setting of ischaemic myocardium.
It is noteworthy that a characteristic ST elevation was observed in 94% of cases (Figure 2); however, the ST elevation was not associated with ischaemia or fatal arrhythmia, and the induced change returned to the level observed prior to nicorandil injection within a few minutes. The ST change may be due to the drug effect of Nicorandil on sarcolemmal KATP channels. Although nicorandil activates both mitochondrial and sarcolemmal KATP channels, it is selective for mitochondrial KATP channels, acting at a 10-fold lower concentration than that required to open sarcolemmal KATP channels in vitro18. Thus, the ST elevation may be useful as a marker that a sufficient dose of nicorandil was administered.
Some animal studies have shown that the use of a KATP channel opener in ischaemic myocardium-induced arrhythmia16,21. Conversely, it also has been shown that nicorandil was anti-arrhythmic when injected into the ischaemic myocardium in an animal model22. The absence of reports in humans has made it unclear whether a KATP channel opener is pro-arrhythmic or anti-arrhythmic. Although opening sarcolemmal KATP channels may increase the risk of ventricular arrhythmia23, this study showed that no ventricular arrhythmia was observed on injection or at reperfusion in the 35 consecutive cases. A larger study is required to confirm the safety because of the small sample size.
Previous studies have demonstrated that glycoprotein IIb/IIIa (GPIIb/IIIa) inhibitors improve microcirculation and mortality in patients undergoing primary PCI for AMI24,25. In this study, intracoronary GPIIb/IIIa inhibitors were not used due to unavailability in Japan. Although it remains unknown whether the benefits of intracoronary nicorandil would still have a beneficial effect compared to placebo in the era of GP IIb-IIIa inhibitors, the unique characteristics of Nicorandil as a potassium channel opener may offer adjunctive benefit to protect reperfusion injury after revascularisation. Further investigation is needed to determine the effect of Nicorandil and GPIIb/IIIa inhibitors on microcirculation and mortality in AMI patients.
To compare left ventricular wall motion in patients with AMI, many other studies have selected patients with anterior infarction. Fatal bradycardia and ventricular arrhythmia are frequent complications of inferior AMI. As our primary concern was to show the safety of nicorandil injection, both anterior and inferior AMI were included in this study.
Limitations. The small sample size of patients derived from a single centre is a limitation of this study. Multicentre studies are required to confirm the safety of intracoronary injections of this drug in a larger patient population.
Conclusions. Our research indicates that intracoronary injection of nicorandil prior to reperfusion may be a safe procedure, and that the protection of left ventricular regional wall motion seen in this study may be attributable to a pharmacologic preconditioning by nicorandil. Therefore, intracoronary nicorandil injection could be a potential therapy to protect the myocardium from reperfusion injury in patients with AMI.

