Abstract
Aim: To define the incidence of procedural related myocardial infarction (MI) in patients undergoing elective PCI using different definitions of MI, especially focusing on the criteria proposed by the European Society of Cardiology (ESC) and the American College of Cardiology (ACC) for the definition of MI.
Methods and results: A prospective study including 220 patients scheduled for elective PCI. To be included, preprocedural values of the following biochemical markers had to be normal; aspartate aminotransferase (AST), creatine kinase (CK) , creatinine kinase MB fraction (mass concentration) (CK-MBmass) and cardiac troponin I (cTnI).
According to different definitions the incidence of procedural related MI following PCI differed from 0,9% (previous WHO definition) to 26,4% (ESC/ACC criteria). Other commonly used definitions of MI resulted in incidence rates between these values.
Conclusions: Depending on definitions used the incidence of procedural MI following elective PCI may vary by a factor of 30. This makes comparison of MI rates between institutions difficult. Furthermore, outcome and conclusions in interventional studies with MI as an endpoint may differ according to definitions used for procedural MI. A clear description of the applied definition of procedural MI following PCI is mandatory. For epidemiological and other reasons a separate ICD code is proposed for MIs caused by PCI.
Introduction
Following percutaneous coronary interventions (PCI) markers of myocardial injury are frequently elevated1-3. The biochemical evidence of procedural myocardial injury corresponds to micro-infarctions visualised by contrast-enhanced MRI4,5. Apart from small damage, in some cases major myocardial infarction may occur. Conflicting data exist regarding the prognostic significance of increase in markers of myocardial injury following PCI. Results from studies on the glycoprotein IIb-IIIa receptor blocker abciximab demonstrated that even modest elevation of CK-MB following PCI was associated with impaired outcome6-8, while others have concluded that minor elevations in biomarkers do not influence prognosis9-13.
Most studies examining the incidence of myocardial injury following PCI have used CK-MB as the biochemical marker. With use of troponins an even more sensitive diagnosis of minor myocardial damage is possible and the incidence of elevated troponins following PCI is reported as high as 44%14.
The use of sensitive markers of myocardial injury following PCI has implications beyond those of patient prognosis. Recently the criteria for myocardial infarction were revised15. According to the document by the Joint Committee of the European Society of Cardiology (ESC) and the American College of Cardiology (ACC) maximal concentration of cardiac troponin T (cTnT) or cardiac troponin I (cTnI) following coronary intervention exceeding the decision limit defined as the 99th percentile of the value for a reference control group is defined as myocardial infarction15.
Routines may differ considerably between institutions both regarding which markers are used, definition of cut-off values and time points for blood sampling following PCI. The consequences are wide variations in the reported incidence of periprocedural myocardial infarction although patient populations, operator skills and true complications rates are similar or even identical.
Criteria for definition of myocardial infarction also differ between studies where myocardial infarction is an endpoint, making it difficult to compare the incidence of periprocedural myocardial infarction between different studies. Other important aspects are the legal and psychological ones; whether a patient is told or not that an otherwise uneventful PCI procedure was followed by a myocardial infarction is not a matter of indifference.
The aim of this study was to define the incidence of procedural related myocardial infarction in patients undergoing elective PCI using different definitions of myocardial infarction.
Methods and material
The study population comprised 220 consecutive patients (180 men and 40 women) with a median age of 58.5 years (39-84) undergoing planned, elective PCI. The majority (84%) had stable angina pectoris.
As part of our clinical routines baseline analysis of four biochemical markers; aspartate aminotransferase (AST), creatine kinase (CK), creatine kinase MB fraction (mass concentration), (CK-MBmass) and cardiac troponin I (cTnI) was performed within 24 hours prior to procedure. Only patients with baseline values below upper limit of normal (ULN) for AST, CK and CK-MBmass and below the detection limit for cTnI were included in the study.
Biochemical analyses. Standard laboratory methods were used for analysis of AST, CK and CKMBmass. ULN for AST was 35 U/l for women and 50 U/l for men, ULN for CK was 200 and 250 U/l for women and men respectively and for CK-MBmass ULN was 5 µg/l for both sexes. cTnI was analysed by a microparticle enzyme immunoassay (Abbott AxSYM, Abbott Laboratories, USA). The detection limit for cTnI by this assay is 0,24µg/l while the 99th percentile is reported between 0,3-0,8 µg/l16-18. In our laboratory values for cTnI > 0,3 µg/l were reported and this was defined as the detection limit in this study. According to the ESC/ACC criteria acceptable imprecision (coefficient of variation, CV) at the 99th percentile should be < 10%15. Since the ESC/ACC document was published a gap between the 99th percentile reference limit and the lowest troponin concentration that provides a 10% CV is clearly demonstrated18. It is generally accepted that in clinical practice cTnI concentrations at the decision limit should be measured with a CV < 10%19-21. For cTnI measured with the Abbott AxSYM assay the lowest concentration allowing a total imprecision < 10% is reported between 0,84-1,22 µg/l16,18. Based on the above data and considerations a cut-off for cTnI at 1,0 µg/l was used in the most sensitive definition of MI in this study.
Following PCI, the same biochemical markers were analysed 14-21 hours post procedure in blood drawn in the morning of the next day. ECG was recorded at baseline, immediate post PCI and the next morning.
Procedure. In this patient series intracoronary stent was implanted in 76% and there was no use of drug eluting stents as this study was conducted before these stents were available. The PCI procedure was successful in 95% of patients. There was no need for acute bypass surgery and there was no hospital mortality.
Definitions of myocardial infarction. The incidence of PCI related myocardial infarction was defined according to each of the following definitions: A) Development of pathologic Q-waves and AST or CK > 1.5xULN, B) CK-MB> 3xULN, C) CK-MB> 2xULN, D) cTnI > 2,2 µg/l, E) cTnI > 1,0 µg/l. Definition D) with a cut-off value for cTnI at 2.2 µg/l corresponds to a cTnT value of 0,1 µg/l according to results obtained in a series of blood samples analysed with both methods in our laboratory (unpublished data). The reason for including definition D) is that cTnT > 0,1 µg/l is a commonly used cut-off value for the definition of myocardial infarction in the clinical setting outside PCI.
The study was approved by the regional committee for medical ethics.
Statistical analysis
Results from biomarker analyses are presented as median values with 5 and 95 percentiles. For comparison of biomarker values pre and post PCI the Wilcoxon signed ranks test was used. Values for p < 0.05 were considered significant. Statistical analysis was performed using SPSS 13.0 (Statistical package for Social Science, SPSS Inc. Chicago, IL, USA).
Results
Post PCI values for AST, CK and CK-MBmass were above ULN in 1.8%, 2.3 % and 17.3% of patients respectively, while cTnI values above the detection limit was measured in 55% of patients following PCI (Figure 1).
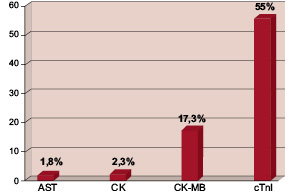
Figure 1. Incidence of increase in different biochemical markers >ULN (upper limit of normal) following PCI. AST=aspartate aminotransferase, CK= creatine kinase, CK-MBmass= creatine kinase MB fraction (mass concentration), cTnI= cardiac troponin I. For cardiac troponin I the figure demonstrates the percentage of patients with post PCI values above the detection limit.
Figure 2 shows the distribution of cTnI values above the detection limit demonstrating that in the great majority of patients with elevated cTnI this increase was minor.
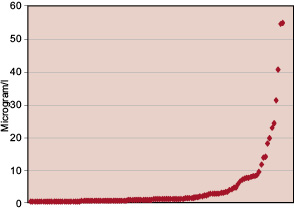
Figure 2. Distribution of cardiac troponin I values > 0,3 µg/l following PCI.
Cardiac troponin I values above the cut-off value 1,0 µg/l were present in 26,4% of patients.
In table 1 pre- and post- PCI values for AST, CK and CK-MB are compared.
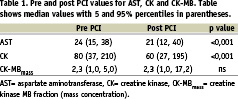
For AST and CK there was a significant decrease from baseline to the day following PCI while median value for CK-MB did not change. According to the five different definitions of myocardial infarction outlined above, the incidence of procedural myocardial infarction was 0.9% (A), 5.5% (B), 9.1%(C), 15,5% (D) and 26,4% (E) (Figure 3).
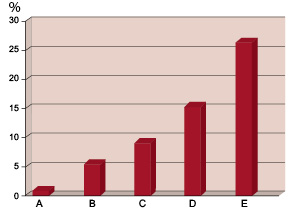
Figure 3. Incidence of myocardial infarction following PCI according to different definitions used. A: Development of pathologic Q-waves and AST or CK > 1.5xULN, B: CK-MB> 3xULN, C: CK-MB> 2xULN, D: cTnI > 2.2 µg/l, E: cTnI > 1,0 µg/l.
Only two patients satisfied definition A with development of pathological Q-waves. These patients had marked increase in all four biomarkers analysed and accordingly satisfied the criteria B-E. All the patients satisfying criterion C also satisfied criterion D and E thus demonstrating that the two definitions based on cTnI measurements did not miss any case defined with myocardial infarction based on CK-MB criteria.
Discussion
In this study we have demonstrated that depending on definitions used the incidence of periprocedural myocardial infarction following elective PCI differs by a factor of 30. The definitions we have used span the range from the classical WHO definition of myocardial infarction to the definition of procedural myocardial infarction proposed in the ESC/ACC consensus document15. It should be noted that regarding the latter definition we have used a cut-off point representing a cTnI concentration at which the total imprecision of the method is < 10%. A cut off level for cTnI at the 99th percentile would have resulted in an incidence of procedural MI even higher than 26%.
According to the ESC/ACC definition, rise of biochemical markers of myocardial damage following PCI satisfies the criteria for myocardial infarction even though the procedure otherwise is completely uneventful with no chest pain or ECG-changes. While any damage to the myocardium itself is best avoided, it is well known that minor myocardial damage may occur in a substantial number of patients undergoing PCI. The mechanism for this may be side branch occlusion, microembolisation from the lesion being dilated or other mechanisms13,21,23.
The findings in our study have several implications. Unless standardisation of definitions used, PCI results between institutions can hardly be compared with regard to incidence of periprocedural myocardial infarction. The great majority (figure 2) of myocardial infarctions in our patient series represent minor myocardial injuries that according to recent publications are without any clinical consequences12,13. Accordingly, it could be debated whether the diagnosis myocardial infarction without modification should be labelled on the patients records in these cases. It is also a matter of debate whether to use or not the words myocardial infarction when giving information to patients with minor myocardial damage following PCI.
In an intravascular ultrasound study by Iakovou et al., stent over-expansion with a greater than reference lumen cross-sectional area was accompanied by a higher periprocedural CK-MB release but a lower target lesion revascularisation rate and a trend toward lower mortality at one year11. According to this study it seems that there are PCI procedures where a rise in biochemical markers of myocardial injury is associated with improved prognosis.
Our results are comparable to those reported by others. In the Johansen et al. study of patients undergoing elective PCI CK-MB > 2xULN was reported in 12% and cTnT > 0,1 µg/l in 28%2. In the CAPTURE, EPICS and EPILOGUE studies a wide spectrum of patients underwent PCI and incidence of CK-MB > 3xULN was reported from 3,7-8,7% in these studies with a significantly lower incidence of periprocedural myocardial infarctions in patients treated with abciximab28-30.
The lower values of AST and CK the day after PCI (table 1) indicate that following PCI there was a hemodilution that could be explained by the administration of X-ray dye and intravenous fluid during and following the procedure. This hemodilution could mask minor releases of biomarkers from the myocardium thus resulting in some patients with minor myocardial injury not being diagnosed. As a consequence, even different regimens regarding hydration during and following PCI may influence the incidence of periprocedural myocardial infarction being registered.
Unless periprocedural and spontaneous myocardial infarctions are differentiated, the interpretation of changes in the epidemiology of myocardial infarction is made difficult. True variations in incidence of myocardial infarction over time and between regions is only possible if criteria for the diagnosis are harmonised and the periprocedural myocardial infarctions following PCI are identified for instance by a separate ICD code.
The clinical and prognostic significance of minor troponin rise following PCI has been debated6-8,9-13. According to Roe et al. a rise in CK-MB > 3xULN following PCI was an indicator for worse prognosis in patients with acute coronary syndromes, while periprocedural CK-MB rise below this level did not predict adverse outcome. Conflicting data regarding the prognostic implications of rise in biomarkers following PCI could be explained by lack of power in some of the studies addressing this issue.
In this study we have included some frequently used definitions of myocardial infarction in interventional studies. As myocardial infarction often is the strongest driving endpoint in these studies, definitions used for this particular endpoint will have major impact on study results. In clinical studies comparing invasive vs. noninvasive strategy in patients with unstable coronary artery syndromes, definitions of periprocedural myocardial infarction have varied25-27. Also in these studies myocardial infarction has been the most frequently occurring endpoint, and a study including intervention with PCI could turn out to be positive or negative depending on definitions used for myocardial infarction following PCI as this to a large degree will influence the number of endpoints. Furthermore, if the definition of myocardial infarction is based on minor increase in biochemical markers, the clinical significance of reducing this endpoint could be questioned. Therefore, when interpreting studies, including percutaneous coronary intervention, the definitions of periprocedural myocardial infarction used should be considered before any clinical consequences of that particular study can be drawn.
Limitations of the study
There are some limitations to this study. First, the patients studied represent a selection of PCI patients as they were all elective patients with normal baseline values for markers of myocardial injury. In patients with unstable coronary artery syndromes results could differ as unstable patients are more prone to ischaemic complications following PCI. Secondly, only one single blood sample was drawn following the procedure and the time range for this blood sampling varied between 14-21 hours post PCI. This may have resulted in some minor increases in biomarkers being missed, especially CK and CK-MB as the half life for these markers are short. With regard to cTnI, it can be anticipated that due to the longer half-life of this marker our results are representative of the true incidence of post-PCI troponin rise.
Conclusion
Depending on biochemical marker used and definition of cut-off values, the incidence of procedural related myocardial infarction following elective PCI may vary by a factor of 30. This has several implications. It makes comparison of the true complication rates between institutions difficult and confuses the interpretation of epidemiological trends. Different definitions of myocardial infarction following PCI in interventional studies may have major impact on study results as myocardial infarction often is the strongest driving endpoint in these studies. A clear description of the applied definition of periprocedural myocardial infarction following PCI is mandatory and procedural myocardial infarctions should be separated from spontaneous myocardial infarctions by a separate ICD code.